Abstract
Fatty acid–binding proteins (FABPs) play a pivotal role in the metabolism of fatty acids and are expressed in a tissue-specific manner. FABP1 is most abundantly expressed in the liver where it accounts for about 10% of the total cytosolic protein and is thought to have diagnostic utility. To comprehensively determine FABP1 expression in normal and neoplastic tissues, a tissue microarray containing 17,071 samples from 150 different tumor types and subtypes as well as 608 samples of 76 different normal tissue types was analyzed by immunohistochemistry. Among normal tissues, a strong FABP1 immunostaining was observed in hepatocytes, proximal tubuli of the kidney and epithelium of small intestine, appendix, and the colorectum. FABP1 positivity was found in 24 of 150 tumor categories, including 17 tumor categories with at least 1 strongly positive case. The highest FABP1 positivity rates were seen in colorectal adenomas (86%), in colorectal adenocarcinomas (71.1%), and in hepatocellular carcinomas (65.3%), followed by mucinous carcinoma of the ovary (34.6%), cholangiocarcinoma (21.6%), and various adenocarcinomas from the digestive tract (10–23%). Eleven additional entities had positivity rates between 0.2 and 6.5%. FABP1 staining was not seen in 169 primary adenocarcinomas of the lung. In colorectal cancer, reduced FABP1 expression was linked to poor-grade, right-sided tumor location, microsatellite instability (p < 0.0001 each), and absence of BRAF V600E mutations (p = 0.001), but unrelated to pT and pN status. FABP1 expression has considerably high tumor specificity. As FABP1 expression was virtually absent in adenocarcinomas of the lung, FABP1 immunohistochemistry might be particularly helpful to assist in the identification of metastatic colorectal or gastrointestinal adenocarcinoma to the lung.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatty acid–binding proteins (FABPs) constitute a family of at least 9 proteins, which play a pivotal role in the metabolism of fatty acids and related molecules. All FABPs are expressed in a tissue-specific manner, and their levels of expression are considered to be proportional to the rate of fatty acid metabolism [1,2,3,4]. Fatty acid–binding protein 1, also termed liver FABP (L-FABP), is expressed from the FABP1 gene located at human chromosome 2p11.2 [5]. The 14-kilodalton protein is most abundantly expressed in the liver where it accounts for about 10% of the total cytosolic protein [6, 7]. FABP1 is involved in the binding, transport, and metabolism of long-chain fatty acids in the liver [6, 7]. Unlike other members of the FABP family, the large hydrophobic binding pocket located in the FABP1 structure is capable of binding to a particularly broad spectrum of hydrophobic ligands and to simultaneously attach multiple ligands [8]. FABP1 ligands include bilirubin, bile acids, or monoglycerides but also benzodiazepines, fibrates, β-blockers, and non-steroidal anti-inflammatory drugs [9, 10]. FABP1 plays a significant role in preventing cytotoxicity/activity of these molecules [9]. Several mutations of the FABP1 gene have been linked to specific metabolic conditions including obesity, cardiovascular disease, and diabetes [8, 11].
Because of its high tissue specificity, FABP1 expression analysis by immunohistochemistry might have diagnostic utility. Studies using FABP1 immunohistochemistry have so far described FABP1 positivity in 47–100% of hepatocellular carcinomas [12, 13], 47.4–83.3% of various subtypes of lung cancer [14], 30–81.5% of colorectal carcinomas [15, 16], 38.6% of gastric adenocarcinomas [17], 27–36.4% of various kidney cancer subtypes [18], and in 12.1% of pancreatic carcinomas [19]. Many other tumor entities have so far not been systematically analyzed.
In order to comprehensively assess the potential diagnostic utility of FABP1 expression in cancer, a preexisting set of tissue microarrays containing more than 17,000 tumor tissue samples from 150 different tumor types and subtypes as well as 76 non-neoplastic tissue categories was analyzed by immunohistochemistry (IHC) in this study.
Material and methods
Tissue microarrays (TMAs)
The normal TMA was composed of 8 samples from 8 different donors for each of 76 different normal tissue types (608 samples on one slide). The cancer TMAs contained a total of 17,071 primary tumors from 150 tumor types and subtypes. Detailed histopathological data on tumor phenotype and molecular data on microsatellite instability, RAS mutations, and BRAF V600E mutations were available from the majority of 2351 colorectal adenocarcinomas. The composition of both normal and cancer TMAs is described in detail in the “Results” section. All samples were from the archives of the Institute of Pathology, University Hospital of Hamburg, Germany; the Institute of Pathology, Clinical Center Osnabrück, Germany; and the Department of Pathology, Academic Hospital Fuerth, Germany. Tissues were fixed in 4% buffered formalin and then embedded in paraffin. The TMA manufacturing process was described earlier in detail [20, 21]. In brief, one tissue spot (diameter: 0.6 mm) was transmitted from a cancer containing donor block in an empty recipient paraffin block. The use of archived remnants of diagnostic tissues for manufacturing of TMAs and their analysis for research purposes as well as patient data analysis has been approved by local laws (HmbKHG, §12) and by the local ethics committee (Ethics Commission Hamburg, WF-049/09). All work has been carried out in compliance with the Helsinki Declaration.
Immunohistochemistry (IHC)
Freshly prepared TMA sections were immunostained on one day in one experiment. Slides were deparaffinized with xylol, rehydrated through a graded alcohol series, and exposed to heat-induced antigen retrieval for 5 min in an autoclave at 121 °C in pH 7,8 Dako target Retrieval Solution™ (Agilent, CA, USA; #S2367). Endogenous peroxidase activity was blocked with Dako Peroxidase Blocking Solution™ (Agilent, CA, USA; #52,023) for 10 min. Primary antibody specific against FABP1 protein (mouse monoclonal, MSVA-501 M, #3737-501 M, MS Validated Antibodies, Hamburg, Germany) was applied at 37 °C for 60 min at a dilution of 1:150. Bound antibody was visualized using the EnVision Kit™ (Agilent, CA, USA; #K5007) according to the manufacturer’s directions. The sections were counterstained with haemalaun. For tumor tissues, the percentage of FABP1-positive tumor cells was estimated, and the staining intensity was semi-quantitatively recorded (0, 1 + , 2 + , 3 +). For statistical analyses, the staining results were categorized into four groups as described before [22]: negative, no staining at all; weak staining, staining intensity of 1 + in ≤ 70% or staining intensity of 2 + in ≤ 30% of tumor cells; moderate staining, staining intensity of 1 + in > 70%, or staining intensity of 2 + in > 30% but in ≤ 70% or staining intensity of 3 + in ≤ 30% of tumor cells; and strong staining, staining intensity of 2 + in > 70% or staining intensity of 3 + in > 30% of tumor cells. Examples of tumors with different scores are shown in Suppl. Figure 1.
Statistics
Statistical calculations were performed with JMP 14 software (SAS Institute Inc., NC, USA). Contingency tables and the chi2 test were performed to search for associations between FABP1 immunostaining and tumor phenotype. A p value of ≤ 0.05 was defined as significant. Cox proportional hazard regression analysis was performed to test the statistical independence of associations between pathological and molecular variables.
Results
FABP1 in normal tissues
A strong FABP1 immunostaining was observed in hepatocytes of the liver, in proximal tubular cells of the kidney, and in epithelial cells of the small intestine, appendix, and the colorectum. In the entire intestine, the staining was strongest in the surface epithelium and sometimes low or even inexistent in the crypt bases. In the stomach epithelium, FABP1 staining was usually absent. Focal positivity was seen, however, in case of intestinal metaplasia. In case of very strong staining of intestinal or liver cells, adjacent structures often also showed FABP1 immunostaining. This is considered a contamination artifact due to diffusion of the antigen. Representative images of FABP1-positive normal tissues are shown in Fig. 1.
FABP1 immunostaining in normal tissues. The panels show a strong (3 +) cytoplasmic FABP1 staining of hepatocytes in the liver (A), surface epithelium of the appendix (B), and the ileum (C) as well as in proximal tubular cells of the kidney (D). FABP1 expression can be so strong in these tissues that considerable contamination artifacts occur in adjacent cells/tissues (A–C). FABP1 staining is lacking in the renal medulla (E) and in the stomach epithelium (F)
FABP1 in cancer
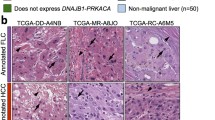
A positive FABP1 immunostaining was detectable in 1980 (14%) of the 14,597 analyzable tumors, including 470 (3.2%) with weak, 563 (3.9%) with moderate, and 947 (6.5%) with strong immunostaining. Overall, 24 (16%) of 150 tumor categories showed detectable FABP1 expression with 17 (11%) tumor categories including at least one case with strong positivity (Table 1). Representative images of FABP1-positive tumors are shown in Fig. 2. By far the highest positivity rates were seen in colorectal adenomas (44–88%), in colorectal adenocarcinomas (71%), and in hepatocellular carcinomas (65%), followed by mucinous carcinoma of the ovary (35%), cholangiocarcinoma (22%), and various adenocarcinomas from the digestive tract (10–23%). Of note, none of our FABP1-positive cholangiocarcinomas qualified for a diagnosis of combined HCC-cholangiocarcinoma as all of these tumors showed a predominantly small-glandular growth pattern and did not show any HepPar1 or arginase1 immunostaining (data not shown). Eleven further tumor entities had positivity rates between 0.2 and 6.5%. A graphical representation of a ranking order of tumor entities according to their rate of FABP1-positive and strongly positive cases is given in Fig. 3. FABP1 expression was not found in any of 252 arrayed lung cancers, including 169 adenocarcinomas of the lung. FABP1 was also negative in all 85 pulmonary adenocarcinomas for which data were available from previous studies on CK20 [23], villin [24], and SATB2 [25]. Evidence for a possible enteric/intestinal differentiation had been found in 20 (24%) of these tumors because of a positive staining for at least one of these intestinal markers (Supplementary Table 1). The relationship between FABP1 immunostaining and histopathological and molecular features of colorectal adenocarcinomas and hepatocellular carcinomas are shown in Table 2. In colorectal cancer, reduced FABP1 expression was strikingly linked to histologic grade, microsatellite instability (MSI), and tumor location in the right side of the colon (p < 0.0001 each), and absence of BRAF V600E mutations (p = 0.001) but was unrelated to pT and pN status or RAS mutation status. A multivariate analysis including MSI, pT, pN, and histologic grade showed that associations between these parameters and reduced FABP1 expression was driven by the histologic grade and stage (p ≤ 0.05; Supplementary Table 2). Within 84 MSI tumors, reduced FABP1 expression was weakly associated with L0 status (p = 0.0203) and tumor location in the right colon (p = 0.0023). Within 1067 MSS tumors, reduced FABP1 expression was weakly associated with right-sided tumor location (p = 0.0372). In hepatocellular carcinomas, reduced FABP1 expression was linked to advanced stage (p = 0.0002), presence of lymph node metastasis (p = 0.0042), and female gender (p = 0.0002).
FABP1 immunostaining in cancer. The panels show a cytoplasmic FABP1 immunostaining of variable intensity in samples from hepatocellular carcinoma (A), cholangiocarcinoma (B), gastric adenocarcinoma (C), esophageal adenocarcinoma (D), colorectal adenocarcinoma (E), and an adenocarcinoma of the papilla of Vater (F). In several samples, FABP1 expression is so high that contamination artifacts occur in adjacent cells/tissues. FABP1 staining is completely absent in samples from a ductal adenocarcinoma of the pancreas (G) and an adenocarcinoma of the lung (H)
Discussion
Considering the large scale of our study, emphasis was placed on the appropriate validation of our FABP1 immunohistochemistry assay. Based on recommendations of the International Working Group for Antibody Validation (IWGAV), we compared our FABP1 staining data with expression data obtained by another independent method [26]. Normal tissue RNA expression data derived from three different publicly accessible databases [27,28,29,30] were therefore compared with immunostaining results in 76 different normal tissue categories. This broad range of tissues is likely to contain most proteins that are normally expressed at relevant levels in cells of adult humans and should therefore enable the detection of most undesired cross-reactivities of tested antibodies. Specificity of our assay was supported by the limitation of FABP1 immunostaining to kidney, liver, and the intestine. These are the only organs for which significant FABP1 RNA expression had been described.
Our data provide a comprehensive overview on the prevalence and intensity of FABP1 immunostaining across a large variety of human tumor entities. The findings demonstrate that FABP1 expression occurs at highest frequency (65–80%) in hepatocellular carcinomas and colorectal adenocarcinomas, at lower frequency (35%) in mucinous carcinoma of the ovary and in other adenocarcinomas of the digestive tract (10–25%), and only rarely (< 5%) in a limited number of other tumor types. These data not only expand the existing literature but also clarify existing findings which in part are highly discordant with our data. A total of 15 previous studies have reported IHC findings on FABP1 in 12 different tumor entities (results summarized in Fig. 4). While multiple studies describe FABP1 expression frequencies that are in the range of our findings in hepatocellular carcinomas [31,32,33], colorectal adenocarcinomas [16, 34], pancreatic adenocarcinomas [19], and gastric adenocarcinoma [17], we were unable to detect any FABP1-positive cases among 169 adenocarcinomas of the lung, 12 small cell carcinomas of the lung, and 157 chromophobe carcinomas of the kidney. For all these entities, others have described substantial fractions of FABP1-positive cases [14, 18]. Absence of FABP1 expression in lung and kidney cancer is also supported by RNA expression studies summarized in the ICGC/TCGA databases (https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga) and The Human Protein Atlas [30].
Our comprehensive set of data on FABP1 immunostaining in tumors suggests a potential diagnostic utility of FABP1 immunohistochemistry in surgical pathology. While it is obvious from our data that a positive FABP1 immunostaining in a metastatic tissue of unknown origin would pinpoint towards the liver or the gastrointestinal tract as the most likely sites of cancer origin, the highest diagnostic utility may be derived from the constant absence of FABP1 immunostaining in 169 analyzed adenocarcinomas of the lung. As the lung is a common site of metastases, the distinction of primary lung adenocarcinoma from metastatic adenocarcinoma is a frequent diagnostic problem which has high therapeutic implications. A potential utility for this application is particularly supported by the absence of FABP1 staining in 20 pulmonary adenocarcinomas for which cytokeratin 20, SATB2, and/or villin positivity had suggested a possible intestinal/enteric differentiation. A low likelihood of pulmonary adenocarcinomas to become FABP1 positive is also supported by the complete lack of FABP1 RNA expression in 510 pulmonary adenocarcinomas described in the TCGA Pan Cancer Atlas database (https://www.cancer.gov/about-nci/organization/ccg/research/structural-genomics/tcga). A positive FABP1 immunostaining in an adenocarcinoma in the lung may therefore be highly suggestive of an extra-pulmonary tumor origin and favor a metastasis derived from a colorectal cancer or another cancer of the gastrointestinal tract. However, considering that only 71% of our colorectal adenocarcinomas were FABP1 positive and the even lower frequency of FABP1 positivity in other gastrointestinal adenocarcinomas, a negative FABP1 staining cannot serve as evidence for a pulmonary origin of an adenocarcinoma in the lung. Moreover, in case of an adenocarcinoma in the pancreas, FABP1 positivity would argue in favor of a carcinoma derived from the ampulla of Vater (23% positive) and against a ductal adenocarcinoma (1.8% positive). Loss of FABP1 expression in a hepatic tumor has been described as a feature of hepatocellular adenoma [35, 36]. However, our data show that 50–70% of advanced and metastatic hepatocellular carcinomas and up to 20% of low-stage and grade carcinomas may be FABP1 negative. These observations are in line with earlier reports [31, 37, 38] suggesting that a lack of FABP1 staining should be interpreted with care to avoid misdiagnosing a well-differentiated hepatocellular carcinoma as hepatocellular adenoma.
It is of note that FABP1 expression in normal and neoplastic tissues is usually either high or absent. In immunohistochemical analysis, this often results in such an abundant staining reaction that bound antibody can also be seen in the vicinity of FABP1-expressing cells. Such a spill-over of FABP1 protein may either be caused by some physiologic intravital diffusion of the highly abundant FABP1 protein or reflect an ischemia-induced artifact caused by autolytic cell damage occurring between removal of the tissue from the patient and completed tissue fixation. Such “contamination artifacts” must be considered if metastatic tissue is seen in biopsies from the liver because they can lead to questionable staining or false positivity.
The successful analysis of more than 2000 colorectal adenocarcinomas enabled us to analyze the relationship between FABP1 expression, tumor phenotype, and molecular data in this tumor entity. That low FABP1 expression was strongly linked to high-grade, MSI, and right-sided tumor location but unrelated to pT and pN stage is consistent with the results of two earlier studies. In a study on 695 colorectal carcinomas, Wood et al. [39] described a strong link of low FABP1 with MSI and high histologic grade but also failed to find significant associations with advanced stage or patient survival. Lawrie et al. [15] analyzed 249 colorectal adenocarcinomas and found a relationship between low FABP1 and high grade but did not see associations with tumor stage. The mechanism causing low FABP1 expression in colorectal adenocarcinomas with MSI is unclear. Wood et al. [39] suggested a possible role of PPARγ and the interferon γ pathway. It also appears possible that one or several genes that are required for FABP1 expression are inactivated by accumulating mutations in MSI cancers. Silencing of FABP1 expression by specific molecular events is not uncommon. In hepatocellular adenomas, efficient silencing of FABP1 can be caused by biallelic inactivation of hepatocyte nuclear factor 1α (HNF1A) which occurs in 35–40% of cases [40]. That reduced FABP1 expression was driven by high grade—a feature that is commonly related to MSI— and not by MSI in our multivariate analysis may suggest, however, that FABP1 expression loss is merely an indicator of poor differentiation and may not have further biological meanings. With respect to molecular mechanisms for FABP1 inactivation, it is also remarkable that FABP1 expression is virtually absent in kidney cancers, although the protein is abundantly seen in the normal kidney.
In summary, our data show that FABP1 expression has high tumor specificity and preferentially occurs in hepatocellular carcinomas, colorectal carcinomas, mucinous ovarian cancer, and other gastrointestinal adenocarcinomas. As FABP1 expression is virtually absent in adenocarcinomas of the lung, FABP1 immunohistochemistry might be most helpful for its distinction from metastatic adenocarcinoma to the lung.
Data availability
All data generated or analyzed during this study are included in this published article. Raw data are available upon reasonable request.
References
Amiri M, Yousefnia S, Seyed Forootan F, Peymani M, Ghaedi K, Nasr Esfahani MH (2018) Diverse roles of fatty acid binding proteins (FABPs) in development and pathogenesis of cancers. Gene 676:171–183. https://doi.org/10.1016/j.gene.2018.07.035
Smathers RL, Petersen DR (2011) The human fatty acid-binding protein family: evolutionary divergences and functions. Hum Genomics 5:170–191. https://doi.org/10.1186/1479-7364-5-3-170
Storch J, Thumser AE (2010) Tissue-specific functions in the fatty acid-binding protein family. J Biol Chem 285:32679–32683. https://doi.org/10.1074/jbc.R110.135210
Thumser AE, Moore JB, Plant NJ (2014) Fatty acid binding proteins: tissue-specific functions in health and disease. Curr Opin Clin Nutr Metab Care 17:124–129. https://doi.org/10.1097/MCO.0000000000000031
Sweetser DA, Birkenmeier EH, Klisak IJ, Zollman S, Sparkes RS, Mohandas T, Lusis AJ, Gordon JI (1987) The human and rodent intestinal fatty acid binding protein genes A comparative analysis of their structure, expression, and linkage relationships. J Biol Chem 262:16060–16071
Vergani L, Fanin M, Martinuzzi A, Galassi A, Appi A, Carrozzo R, Rosa M, Angelini C (1990) Liver fatty acid-binding protein in two cases of human lipid storage. Mol Cell Biochem 98:225–230. https://doi.org/10.1007/BF00231388
Wang G, Bonkovsky HL, de Lemos A, Burczynski FJ (2015) Recent insights into the biological functions of liver fatty acid binding protein 1. J Lipid Res 56:2238–2247. https://doi.org/10.1194/jlr.R056705
Furuhashi M, Hotamisligil GS (2008) Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov 7:489–503. https://doi.org/10.1038/nrd2589
Chuang S, Velkov T, Horne J, Porter CJ, Scanlon MJ (2008) Characterization of the drug binding specificity of rat liver fatty acid binding protein. J Med Chem 51:3755–3764. https://doi.org/10.1021/jm701192w
McKillop IH, Girardi CA, Thompson KJ (2019) Role of fatty acid binding proteins (FABPs) in cancer development and progression. Cell Signal 62:109336. https://doi.org/10.1016/j.cellsig.2019.06.001
Lee CH, Lui DTW, Lam KSL (2021) Adipocyte fatty acid-binding protein, cardiovascular diseases and mortality. Front Immunol 12:589206. https://doi.org/10.3389/fimmu.2021.589206
Suzuki T, Watanabe K, Ono T (1990) Immunohistochemical demonstration of liver fatty acid-binding protein in human hepatocellular malignancies. J Pathol 161:79–83. https://doi.org/10.1002/path.1711610113
Wang B, Tao X, Huang CZ, Liu JF, Ye YB, Huang AM (2014) Decreased expression of liver-type fatty acid-binding protein is associated with poor prognosis in hepatocellular carcinoma. Hepatogastroenterology 61:1321–1326
Kawamura T, Kanno R, Fujii H, Suzuki T (2005) Expression of liver-type fatty-acid-binding protein, fatty acid synthase and vascular endothelial growth factor in human lung carcinoma. Pathobiology 72:233–240. https://doi.org/10.1159/000089417
Lawrie LC, Dundas SR, Curran S, Murray GI (2004) Liver fatty acid binding protein expression in colorectal neoplasia. Br J Cancer 90:1955–1960. https://doi.org/10.1038/sj.bjc.6601828
Pei H, Zhu H, Zeng S, Li Y, Yang H, Shen L, Chen J, Zeng L, Fan J, Li X, Gong Y, Shen H (2007) Proteome analysis and tissue microarray for profiling protein markers associated with lymph node metastasis in colorectal cancer. J Proteome Res 6:2495–2501. https://doi.org/10.1021/pr060644r
Hashimoto T, Kusakabe T, Watanabe K, Sugino T, Fukuda T, Nashimoto A, Honma K, Sato Y, Kimura H, Fujii H, Suzuki T (2004) Liver-type fatty acid-binding protein is highly expressed in intestinal metaplasia and in a subset of carcinomas of the stomach without association with the fatty acid synthase status in the carcinoma. Pathobiology 71:115–122. https://doi.org/10.1159/000076465
Tolle A, Jung M, Lein M, Johannsen M, Miller K, Moch H, Jung K, Kristiansen G (2009) Brain-type and liver-type fatty acid-binding proteins: new tumor markers for renal cancer? BMC Cancer 9:248. https://doi.org/10.1186/1471-2407-9-248
Sharaf RN, Butte AJ, Montgomery KD, Pai R, Dudley JT, Pasricha PJ (2011) Computational prediction and experimental validation associating FABP-1 and pancreatic adenocarcinoma with diabetes BMC Gastroenterol 11:5. https://doi.org/10.1186/1471-230X-11-5
Dancau AM, Simon R, Mirlacher M, Sauter G (2016) Tissue Microarrays Methods Mol Biol 1381:53–65. https://doi.org/10.1007/978-1-4939-3204-7_3
Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4:844–847. https://doi.org/10.1038/nm0798-844
Simon R, Mirlacher M, Sauter G (2010) Immunohistochemical analysis of tissue microarrays. Methods Mol Biol 664:113–126. https://doi.org/10.1007/978-1-60761-806-5_12
Dum D, Menz A, Volkel C, De Wispelaere N, Hinsch A, Gorbokon N, Lennartz M, Luebke AM, Hube-Magg C, Kluth M, Fraune C, Moller K, Bernreuther C, Lebok P, Clauditz TS, Jacobsen F, Sauter G, Uhlig R, Wilczak W, Steurer S, Minner S, Marx AH, Simon R, Burandt E, Krech T (2022) Cytokeratin 7 and cytokeratin 20 expression in cancer: A tissue microarray study on 15,424 cancers. Exp Mol Pathol 126:104762. https://doi.org/10.1016/j.yexmp.2022.104762
Dum D, Lennartz M, Menz A, Kluth M, Hube-Magg C, Weidemann S, Fraune C, Luebke AM, Hornsteiner L, Bernreuther C, Simon R, Clauditz TS, Sauter G, Uhlig R, Hinsch A, Kind S, Jacobsen F, Moller K, Wilczak W, Steurer S, Minner S, Burandt E, Marx AH, Krech T, Lebok P (2022) Villin expression in human tumours: a tissue microarray study on 14,398 tumours Expert Rev Mol Diagn. https://doi.org/10.1080/14737159.2022.2104122
Dum D, Kromm D, Lennartz M, De Wispelaere N, Büscheck F, Luebke AM, Burandt E, Menz A, Kluth M, Hube-Magg C, Hinsch A, Höflmayer D, Weidemann S, Fraune C, Möller K, Lebok P, Sauter G, Simon R, Uhlig R, Wilczak W, Minner S, Krech R, Bernreuther C, Marx AH, Steurer S, Jacobsen F, Clauditz TS, Krech T (2022) SATB2 expression in human tumors: a tissue microarray study on more than 15,000 tumors Arch. Pathol. Lab, Med (In press)
Uhlen M, Bandrowski A, Carr S, Edwards A, Ellenberg J, Lundberg E, Rimm DL, Rodriguez H, Hiltke T, Snyder M, Yamamoto T (2016) A proposal for validation of antibodies. Nat Methods 13:823–827. https://doi.org/10.1038/nmeth.3995
Consortium GT (2013) The genotype-tissue expression (GTEx) project. Nat Genet 45:580–585. https://doi.org/10.1038/ng.2653
Lizio M, Abugessaisa I, Noguchi S, Kondo A, Hasegawa A, Hon CC, de Hoon M, Severin J, Oki S, Hayashizaki Y, Carninci P, Kasukawa T, Kawaji H (2019) Update of the FANTOM web resource: expansion to provide additional transcriptome atlases. Nucleic Acids Res 47:D752–D758. https://doi.org/10.1093/nar/gky1099
Lizio M, Harshbarger J, Shimoji H, Severin J, Kasukawa T, Sahin S, Abugessaisa I, Fukuda S, Hori F, Ishikawa-Kato S, Mungall CJ, Arner E, Baillie JK, Bertin N, Bono H, de Hoon M, Diehl AD, Dimont E, Freeman TC, Fujieda K, Hide W, Kaliyaperumal R, Katayama T, Lassmann T, Meehan TF, Nishikata K, Ono H, Rehli M, Sandelin A, Schultes EA, t Hoen PA, Tatum Z, Thompson M, Toyoda T, Wright DW, Daub CO, Itoh M, Carninci P, Hayashizaki Y, Forrest AR, Kawaji H, consortium F, (2015) Gateways to the FANTOM5 promoter level mammalian expression atlas. Genome Biol 16:22. https://doi.org/10.1186/s13059-014-0560-6
Thul PJ, Akesson L, Wiking M, Mahdessian D, Geladaki A, Ait Blal H, Alm T, Asplund A, Bjork L, Breckels LM, Backstrom A, Danielsson F, Fagerberg L, Fall J, Gatto L, Gnann C, Hober S, Hjelmare M, Johansson F, Lee S, Lindskog C, Mulder J, Mulvey CM, Nilsson P, Oksvold P, Rockberg J, Schutten R, Schwenk JM, Sivertsson A, Sjostedt E, Skogs M, Stadler C, Sullivan DP, Tegel H, Winsnes C, Zhang C, Zwahlen M, Mardinoglu A, Ponten F, von Feilitzen K, Lilley KS, Uhlen M, Lundberg E (2017) A subcellular map of the human proteome Science 356. https://doi.org/10.1126/science.aal3321
Cho SJ, Ferrell LD, Gill RM (2016) Expression of liver fatty acid binding protein in hepatocellular carcinoma. Hum Pathol 50:135–139. https://doi.org/10.1016/j.humpath.2015.12.002
Inoue M, Takahashi Y, Fujii T, Kitagawa M, Fukusato T (2014) Significance of downregulation of liver fatty acid-binding protein in hepatocellular carcinoma. World J Gastroenterol 20:17541–17551. https://doi.org/10.3748/wjg.v20.i46.17541
Reis H, Padden J, Ahrens M, Putter C, Bertram S, Pott LL, Reis AC, Weber F, Juntermanns B, Hoffmann AC, Eisenacher M, Schlaak JF, Canbay A, Meyer HE, Sitek B, Baba HA (2015) Differential proteomic and tissue expression analyses identify valuable diagnostic biomarkers of hepatocellular differentiation and hepatoid adenocarcinomas. Pathology 47:543–550. https://doi.org/10.1097/PAT.0000000000000298
Yamazaki T, Kanda T, Sakai Y, Hatakeyama K (1999) Liver fatty acid-binding protein is a new prognostic factor for hepatic resection of colorectal cancer metastases. J Surg Oncol 72:83–87. https://doi.org/10.1002/(sici)1096-9098(199910)72:2%3c83::aid-jso8%3e3.0.co;2-c
Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Sa Cunha A, Rullier A, Cubel G, Couchy G, Imbeaud S, Balabaud C, Zucman-Rossi J (2007) Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology 46:740–748. https://doi.org/10.1002/hep.21743
Margolskee E, Bao F, de Gonzalez AK, Moreira RK, Lagana S, Sireci AN, Sepulveda AR, Remotti H, Lefkowitch JH, Salomao M (2016) Hepatocellular adenoma classification: a comparative evaluation of immunohistochemistry and targeted mutational analysis. Diagn Pathol 11:27. https://doi.org/10.1186/s13000-016-0475-5
Liu L, Shah SS, Naini BV, French S, Wu TT, Torbenson MS, Chandan VS (2016) Immunostains used to subtype hepatic adenomas do not distinguish hepatic adenomas from hepatocellular carcinomas. Am J Surg Pathol 40:1062–1069. https://doi.org/10.1097/PAS.0000000000000624
Torbenson M (2018) Hepatic adenomas: classification, controversies, and consensus. Surg Pathol Clin 11:351–366. https://doi.org/10.1016/j.path.2018.02.007
Wood SM, Gill AJ, Brodsky AS, Lu S, Friedman K, Karashchuk G, Lombardo K, Yang D, Resnick MB (2017) Fatty acid-binding protein 1 is preferentially lost in microsatellite instable colorectal carcinomas and is immune modulated via the interferon gamma pathway. Mod Pathol 30:123–133. https://doi.org/10.1038/modpathol.2016.170
Bioulac-Sage P, Balabaud C, Zucman-Rossi J (2010) Subtype classification of hepatocellular adenoma. Dig Surg 27:39–45. https://doi.org/10.1159/000268406
Acknowledgements
We are grateful to Melanie Witt, Inge Brandt, Maren Eisenberg, and Sünje Seekamp for excellent technical assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
DD, RS, GS, TK: contributed to conception, design, data collection, data analysis, and manuscript writing.
FB, NG, VR, ML, AML, EB, AHM, DH, PL, FJ, SM, TSC, CB, NCB, DD, TK: participated in pathology data analysis and data interpretation.
TK, AHM collection of samples.
DD, TK: immunohistochemistry analysis.
RS, ML, AO, CHM: data analysis.
DD, RS, GS, TK: study supervision.
All authors agreed to be accountable for the content of the work.
Corresponding author
Ethics declarations
Ethical approval
The usage of archived diagnostic left-over tissues for manufacturing of TMAs and their analysis for research purposes as well as patient data analysis has been approved by local laws (HmbKHG, §12,1) and by the local ethics committee (Ethics commission Hamburg, WF-049/09). All work has been carried out in compliance with the Helsinki Declaration.
Conflict of interest
The FABP1 antibody clone MSVA-501 M was received from MS Validated Antibodies GmbH (owned by a family member of GS).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dum, D., Ocokoljic, A., Lennartz, M. et al. FABP1 expression in human tumors: a tissue microarray study on 17,071 tumors. Virchows Arch 481, 945–961 (2022). https://doi.org/10.1007/s00428-022-03394-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-022-03394-5