Abstract
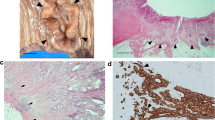
MFAP5, a 25-kD microfibril-associated glycoprotein that is involved in elastic microfibril assembly, has been demonstrated to be significantly downregulated in tumor stroma by previous gene expression study. The aim of this study was to confirm the reduced expression of MFAP5 in colonic tumor stroma using immunohistochemistry and to explore the utility of MFAP5 as a marker to facilitate diagnosing an invasive component versus pseudoinvasion in colon polyps. In all 19 colon cancer resection cases evaluated, while there was intact MFAP5 immunoreactivity in the uninvolved normal connective tissue, there was marked reduction of MFAP5 immunoreactivity in the desmoplastic stroma surrounding the invasive component. The difference in MFAP5 expression levels was most pronounced within the tumor, while a more heterogeneous expression pattern was observed at the tumor invasive front. Reduction of MFAP5 staining was also observed in the stroma around mucin pools in 6 out of 9 sections from mucinous adenocarcinomas and in areas with high-grade dysplasia. For the polypectomy cases, intact expression of MFAP5 was seen in the stroma surrounding the displaced adenomatous glands in 9 out of 12 polyps with pseudoinvasion. Loss of expression of MFAP5 was observed in the stroma surrounding small foci of invasive adenocarcinoma in 8 of 10 malignant polyps. MFAP5 is a useful marker that may help distinguish normal connective tissue from stroma within invasive colonic adenocarcinoma. MFAP5 may facilitate the distinction between pseudoinvasion and true invasive cancer in colonic adenomatous polyps with a sensitivity of 80% (confidence interval 44–96%) and a specificity of 75% (confidence interval 43–93%) in this small cohort.




Similar content being viewed by others
References
Hui L, Chen Y (2015) Tumor microenvironment: sanctuary of the devil. Cancer Lett 368:7–13. https://doi.org/10.1016/j.canlet.2015.07.039
LeBleu VS, Kalluri R (2018) A peek into cancer-associated fibroblasts: origins, functions and translational impact. Dis Model Mech 11:dmm029447. https://doi.org/10.1242/dmm.029447
Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A et al (2015) Proteomics. Tissue-based map of the human proteome. Science 347:1260419. https://doi.org/10.1126/science.1260419
Jia Z, Wang Y, Sawyers A, Yao H, Rahmatpanah F, Xia X-Q, Xu Q, Pio R, Turan T, Koziol JA, Goodison S, Carpenter P, Wang-Rodriguez J, Simoneau A, Meyskens F, Sutton M, Lernhardt W, Beach T, Monforte J, McClelland M, Mercola D (2011) Diagnosis of prostate cancer using differentially expressed genes in stroma. Cancer Res 71:2476–2487. https://doi.org/10.1158/0008-5472.CAN-10-2585
Deford P, Brown K, Richards RL, King A, Newburn K, Westover K, Albig AR (2016) MAGP2 controls Notch via interactions with RGD binding integrins: identification of a novel ECM-integrin-Notch signaling axis. Exp Cell Res 341:84–91. https://doi.org/10.1016/j.yexcr.2016.01.011
Nehring LC, Miyamoto A, Hein PW, Weinmaster G, Shipley JM (2005) The extracellular matrix protein MAGP-2 interacts with Jagged1 and induces its shedding from the cell surface. J Biol Chem 280:20349–20355. https://doi.org/10.1074/jbc.M500273200
Marti P, Stein C, Blumer T, Abraham Y, Dill MT, Pikiolek M, Orsini V, Jurisic G, Megel P, Makowska Z, Agarinis C, Tornillo L, Bouwmeester T, Ruffner H, Bauer A, Parker CN, Schmelzle T, Terracciano LM, Heim MH, Tchorz JS (2015) YAP promotes proliferation, chemoresistance, and angiogenesis in human cholangiocarcinoma through TEAD transcription factors. Hepatol Baltim Md 62:1497–1510. https://doi.org/10.1002/hep.27992
Miyamoto A, Lau R, Hein PW, Shipley JM, Weinmaster G (2006) Microfibrillar proteins MAGP-1 and MAGP-2 induce Notch1 extracellular domain dissociation and receptor activation. J Biol Chem 281:10089–10097. https://doi.org/10.1074/jbc.M600298200
Li R, Herriges JC, Chen L, Mecham RP, Sun X (2017) FGF receptors control alveolar elastogenesis. Dev Camb Engl 144:4563–4572. https://doi.org/10.1242/dev.149443
Barbier M, Gross M-S, Aubart M, Hanna N, Kessler K, Guo D-C, Tosolini L, Ho-Tin-Noe B, Regalado E, Varret M, Abifadel M, Milleron O, Odent S, Dupuis-Girod S, Faivre L, Edouard T, Dulac Y, Busa T, Gouya L, Milewicz DM, Jondeau G, Boileau C (2014) MFAP5 loss-of-function mutations underscore the involvement of matrix alteration in the pathogenesis of familial thoracic aortic aneurysms and dissections. Am J Hum Genet 95:736–743. https://doi.org/10.1016/j.ajhg.2014.10.018
Karimi A, Milewicz DM (2016) Structure of the elastin-contractile units in the thoracic aorta and how genes that cause thoracic aortic aneurysms and dissections disrupt this structure. Can J Cardiol 32:26–34. https://doi.org/10.1016/j.cjca.2015.11.004
Schubert JA, Landis BJ, Shikany AR, Hinton RB, Ware SM (2016;170A) Clinically relevant variants identified in thoracic aortic aneurysm patients by research exome sequencing. Am J Med Genet A 170:1288–1294. https://doi.org/10.1002/ajmg.a.37568
Mohamed SA, Sievers HH, Hanke T, Richardt D, Schmidtke C, Charitos EI et al (2009) Pathway analysis of differentially expressed genes in patients with acute aortic dissection. Biomark Insights 4:81–90
Bhosale PG, Cristea S, Ambatipudi S, Desai RS, Kumar R, Patil A, Kane S, Borges AM, Schäffer AA, Beerenwinkel N, Mahimkar MB (2017) Chromosomal alterations and gene expression changes associated with the progression of leukoplakia to advanced gingivobuccal cancer. Transl Oncol 10:396–409. https://doi.org/10.1016/j.tranon.2017.03.008
Yang X, Wu K, Li S, Hu L, Han J, Zhu D, Tian X, Liu W, Tian Z, Zhong L, Yan M, Zhang C, Zhang Z (2017) MFAP5 and TNNC1: potential markers for predicting occult cervical lymphatic metastasis and prognosis in early stage tongue cancer. Oncotarget 8:2525–2535. https://doi.org/10.18632/oncotarget.12446
Ceder R, Haig Y, Merne M, Hansson A, Zheng X, Roberg K, Nees M, Iljin K, Bloor BK, Morgan PR, Fadeel B, Grafström RC (2012) Differentiation-promoting culture of competent and noncompetent keratinocytes identifies biomarkers for head and neck cancer. Am J Pathol 180:457–472. https://doi.org/10.1016/j.ajpath.2011.10.016
Leung CS, Yeung T-L, Yip K-P, Pradeep S, Balasubramanian L, Liu J, Wong KK, Mangala LS, Armaiz-Pena GN, Lopez-Berestein G, Sood AK, Birrer MJ, Mok SC (2014) Calcium-dependent FAK/CREB/TNNC1 signalling mediates the effect of stromal MFAP5 on ovarian cancer metastatic potential. Nat Commun 5:5092. https://doi.org/10.1038/ncomms6092
Leung CS, Yeung T-L, Yip K-P, Wong K-K, Ho SY, Mangala LS, Sood AK, Lopez-Berestein G, Sheng J, Wong STC, Birrer MJ, Mok SC (2018) Cancer-associated fibroblasts regulate endothelial adhesion protein LPP to promote ovarian cancer chemoresistance. J Clin Invest 128:589–606. https://doi.org/10.1172/JCI95200
Spivey KA, Banyard J (2010) A prognostic gene signature in advanced ovarian cancer reveals a microfibril-associated protein (MAGP2) as a promoter of tumor cell survival and angiogenesis. Cell Adhes Migr 4:169–171
Panarelli NC, Somarathna T, Samowitz WS, Kornacki S, Sanders SA, Novelli MR, Shepherd NA, Yantiss RK (2016) Diagnostic challenges caused by endoscopic biopsy of colonic polyps: a systematic evaluation of epithelial misplacement with review of problematic polyps from the bowel cancer screening program, United Kingdom. Am J Surg Pathol 40:1075–1083. https://doi.org/10.1097/PAS.0000000000000641
Shepherd NA, Griggs RKL (2015) Bowel cancer screening-generated diagnostic conundrum of the century: pseudoinvasion in sigmoid colonic polyps. Mod Pathol 28:S88–S94. https://doi.org/10.1038/modpathol.2014.138
Byun TJ, Han DS, Ahn SB, Cho HS, Eun CS, Jeon YC, Sohn JH, Oh YH (2009) Pseudoinvasion in an adenomatous polyp of the colon mimicking invasive colon cancer. Gut Liver 3:130–133. https://doi.org/10.5009/gnl.2009.3.2.130
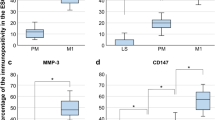
Yantiss RK, Bosenberg MW, Antonioli DA, Odze RD (2002) Utility of MMP-1, p53, E-cadherin, and collagen IV immunohistochemical stains in the differential diagnosis of adenomas with misplaced epithelium versus adenomas with invasive adenocarcinoma. Am J Surg Pathol 26:206–215
Contributions
LZ: Study design, collecting data, analyzing data, preparing manuscript, revising manuscript
MW: Analyzing data, preparing manuscript
JLH: Analyzing data, technical support, preparing manuscript, revising manuscript
TK, TA, SYX: Contributing cases, analyzing data
JH: Study design, collecting data, analyzing data, preparing manuscript
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study has been approved by the Institutional Review Board of University of Chicago.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Figure 1
Staining pattern of MFAP5 in tumor stroma in comparison with SMA. MFAP5 staining is significantly reduced (lost) in tumor stroma (left, arrow), but SMA staining is preserved (right, arrow). (JPG 167 kb)
Supplementary Figure 2
Staining pattern of MFAP5 in benign colon in comparison with desmin and SMA. While the exact function of MFAP5 protein is unknown, MFAP5 immunostain, unlike desmin or SMA, does not stain smooth muscle. It appears to stain both myofibroblasts (similar to SMA) and extracellular matrix material. (JPG 167 kb)
Supplementary Figure 3
High power view of MFAP5 staining pattern in benign lamina propria, benign submucosa and tumor stroma. MFAP5 stains both myofibroblasts and extracellular matrix in benign mucosa and submucosa. There is no MFAP5 staining in stroma adjacent to invasive tumor. (JPG 188 kb)
Supplementary Figure 4
MFAP5 staining pattern at tumor invasive front. MFAP5 staining loss can be heterogeneous at the invasive front, especially in T3 tumors in this small cohort. (JPG 178 kb)
Supplementary Figure 5
MFAP5 expression in areas with abundant mucin. MFAP5 expression is reduced in the stroma next to mucin pools in 6 out of 9 sections with abundant mucin production (A and B, blue arrow -MFAP5 loss in tumor stroma). The MFAP5 expression pattern is more heterogeneous in 3 sections, with loss of expression in some areas (blue arrow) but retained expression in other areas (red arrow) (C). (JPG 171 kb)
Supplementary Figure 6
MFAP5 expression in areas with ulceration. While there appears to be negative staining in the ulcerated areas, these areas also contain prominent inflammatory cell infiltrates and proliferating capillaries, which are also negative for MFAP5, complicating interpretation. (JPG 213 kb)
Rights and permissions
About this article
Cite this article
Zhao, L., Westerhoff, M., Hornick, J.L. et al. Loss of microfibril-associated protein 5 (MFAP5) expression in colon cancer stroma. Virchows Arch 476, 383–390 (2020). https://doi.org/10.1007/s00428-019-02649-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-019-02649-y