Abstract
Cells of the immune defence, especially leukocytes, often have to perform their function in tissue areas that are characterized by oxygen deficiency, so-called hypoxia. Physiological hypoxia significantly affects leukocyte function and controls the innate and adaptive immune response mainly through transcriptional gene regulation via the hypoxia-inducible factors (HIFs). Multiple pathogens including components of bacteria, such as lipopolysaccharides (LPS) trigger the activation of leukocytes. HIF pathway activation enables immune cells to adapt to both hypoxic environments in physiological and inflammatory settings and modulates immune cell responses through metabolism changes and crosstalk with other immune-relevant signalling pathways. To study the mutual influence of both processes in vivo, we used a human endotoxemia model, challenging participants with an intravenous LPS injection post or prior to a 4-h stay in a hypoxic chamber with normobaric hypoxia of 10.5% oxygen. We analysed changes in gene expression in whole blood cells and determined inflammatory markers to unveil the crosstalk between both processes. Our investigations showed differentially altered gene expression patterns of HIF and target genes upon in vivo treatment with LPS and hypoxia. Further, we found evidence for effects of hypoxic priming upon inflammation in combination with immunomodulatory effects in whole blood cells in vivo. Our work elucidates the complex interplay of hypoxic and inflammatory HIF regulation in human immune cells and offers new perspectives for further clinical research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
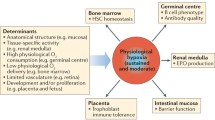
The immune system governed by a complex network of cells and signalling molecules acts as a defence mechanism against infections. In particular, white blood cells must adapt to varying oxygen levels, which can significantly impact their function [4]. In inflammatory conditions like sepsis, where leukocytes face challenges from both hypoxia and infection, immune cell adaptation to inadequate oxygen supply becomes crucial [8]. Hypoxia significantly influences leukocyte function in both physiological and pathological settings by altering leukocyte function and fate with the potential for dysfunctional immune responses and harm to tissues [4, 61].
The transcription factor hypoxia-inducible factor (HIF) plays a central role in adaptation to hypoxia, regulating oxygen-dependent genes to enhance numerous physiological processes [24, 60]. Thereby, HIFs regulate the majority of oxygen-dependent genes and induce genes for enhanced erythropoiesis, iron transport, vascular growth, nitric oxide synthesis, phosphate metabolism, glycolysis and gluconeogenesis [11, 18, 49, 54, 55].
The transcription factor complex HIF-1, comprising oxygen-regulated α-subunits and a constitutively expressed nuclear β-subunit, orchestrates this response. It is of note that regulation of HIF-1 follows a post-translational manner [32, 45]. In normoxic conditions, HIF-α subunits are hydroxylated by prolyl 4-hydroxylase domain (PHD) hydroxylases and degraded by the proteasome [17, 32]. Thereby, the activity of the three homologous hydroxylases PHD1, PHD2 and PHD3 is strictly dependent on the oxygen concentration, which is why they are considered to be the oxygen sensors of the cells [3, 13]. Under oxygen starvation, HIF-α subunits accumulate, translocate into the nucleus and activate HIF-dependent target genes [17, 60].
To counteract oxygen deprivation and thus guarantee cell survival, various strategies increase oxygen availability and delivery. Erythropoietin (EPO) stimulates red blood cell production, while vascular endothelial growth factor (VEGF) promotes angiogenesis [15, 16, 21, 55]. Adrenomedullin (ADM) induces vasodilation, angiogenesis and cell proliferation [5, 7, 46, 63]. Cellular adaptation involves enhanced anaerobic glycolysis, increased glucose uptake mediated by increased expression of glucose transporter 1 (GLUT-1) and the key metabolic enzyme pyruvate dehydrogenase kinase 1 (PDK-1) in parallel to inhibition of oxidative phosphorylation [11, 54].
In leukocytes, inflammatory mediators activate the HIF pathway, further driving gene activation in hypoxia. Pathogens, cytokines, chemokines and environmental changes can directly or indirectly activate HIF-dependent gene regulation [9]. Inflammatory cytokines like tumour necrosis factor alpha (TNF-α) have been shown to induce HIF-dependent gene expression through pathways involving phosphatidylinositol 3‐kinase (PI3K) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) [26, 28].
Exogenous substances, such as LPS, can induce a cellular HIF response, serving as a model for studying inflammatory conditions. It is known from myeloid cells that LPS increases expression of HIF1A mRNA, mediated by LPS-binding to Toll-like receptor 4 (TLR4) and NF-κB-dependent signalling involving p44/42 mitogen-activated protein kinase (MAPK) [22, 23]. The crosstalk between NF-κB and HIF is reciprocal: The HIF1A gene contains binding sites for NF-κB, and NF-κB is important for basal HIF-1 transcription, linking these two master regulatory pathways of innate immunity and hypoxia adaptation [59].
The reciprocal crosstalk between NF-κB and HIF emphasizes their interconnected roles in innate immunity and hypoxia adaptation during inflammation.
The interaction between hypoxia and inflammation, termed inflammatory hypoxia, plays a pivotal role in various diseases such as malignancies, chronic obstructive pulmonary diseases and sepsis [44]. In sepsis patients, the hyperinflammatory phase is characterized by an overexpression of HIF-1, while the immunotolerant phase is marked by reduced HIF-1 levels, contributing to immune dysfunction [19, 20, 50]. These findings suggest that hypoxia signalling holds significant therapeutic potential for manipulating and treating inflammatory diseases, including high-altitude illnesses and sepsis, once the mutual impacts are clearly defined [12]. It should be emphasized that nearly all discoveries thus far have been made in experimental animals, in vitro settings or under pathological conditions in patients. Consequently, it remains challenging to ascertain whether these processes can be directly extrapolated to physiological conditions in vivo among healthy individuals.
However, it is not clear how and to what extent oxygen deprivation and inflammatory responses interact in vivo in human blood cells. To elucidate the complex interplay of hypoxic and inflammatory HIF regulation in vivo and to provide new perspectives for further clinical research, we conducted a human subject study combining both stimuli. We investigated the impact of in vivo hypoxia (10.5% oxygen in the air) on HIF pathway activation in human blood before and after injection of immunostimulating Escherichia coli LPS as a model of acute infection. To assess the effect of hypoxic priming, i.e. hypoxic exposure prior to the LPS stimulus, and the effect of immunostimulation on the hypoxic response, we determined blood and vital parameters.
Methods
Study design and study population
The study was designed as a randomised, double-blind, crossover trail. Healthy male subjects were exposed to 4 h of normobaric hypoxia at 10.5% oxygen in the air following either LPS stimulation (HOX-LPS) of the immune system (intravenous injection of E. coli, HOK364; 0.4 ng LPS per kg body weight) or administration of LPS before 4 h of normobaric hypoxia (LPS-HOX). Transfer time between the two phase of the study (4 h after LPS injection and 4 h of hypoxic exposure) was half an hour.
The study population consisted of 30 healthy male participants (mean age 25.8 ± 2.9 years), with a CRP level below 2 mg/l. Regular use of medication, a body mass index (BMI) greater than 30 and a confirmed COVID-19 infection were the exclusion criteria. Participants of both groups (i.e. HOX-LPS and LPS-HOX) did not differ at baseline levels in age, body mass index, school education, blood pressure, heart rate or white blood cell (WBC) count (Table 1). All volunteers underwent an extensive physical and psychiatric assessment (self‐reported questionnaires and interviews about their medical history) along with a full blood examination, performed and subsequently evaluated by physicians of the Institute of Physiology at the University Medicine Essen. Written and informed consent was obtained from each enrolled individual human subject. Further official approval was obtained from the responsible Ethics Committee of the University Hospital Essen (No 18-8258-BO). The study was conducted according to the principles of the Declaration of Helsinki.
Study conduct
Participants were challenged with a single injection of LPS (Escherichia coli, HOK364, 0.4 ng LPS per kg body weight) before or after a 4-h stay in a hypoxia chamber, simulating a high altitude of 4500 m with normobaric oxygen concentration of 10.5% O2. Thereby, the subjects were exposed to a reduced fraction of oxygen in the inspiratory gas (10.5%) which is half of the oxygen fraction in air. Before LPS injection, oxygen saturation was controlled to be above 95%. In addition to blood sampling at baseline and follow-up, blood was taken on both study days to determine immunological and hypoxic parameters (Fig. 1). On the study days, a butterfly infusion set was used for venous blood sampling and LPS injection. Blood samples were collected 1 h before the first stimulus (depending on the protocol: the injection with LPS or the stay inside the hypoxic chamber) and 2, 4, 6, 8 and 24 h after the start of the respective study protocol (Fig. 1). Blood samples were immediately processed for gene expression analysis. Blood oxygenation was measured with a finger pulse oximeter throughout the study. A final medical examination was performed 1 week after LPS application. The participants tolerated the procedure well as expected. The LPS injection triggered an increase in body temperature (mild fever), which was accompanied by common side effects like headache and mild shivering in some subjects. Exposure to hypoxia caused mild freezing and tiredness in some participants. All participants were at a stable state of health during the whole study protocol.
Study design and blood sampling times. Schematic illustration of the two different study protocols and corresponding blood sampling times. Blood samples were taken at six different time points (baseline, + 2, + 4, + 6, + 8 and + 24 h). The study included study protocols with human subjects being treated with a single lipopolysaccharide (LPS) injection in combination with 4 h exposure to 10.5% O2 hypoxia before (HOX-LPS) or after the injection (LPS-HOX)
White blood cell count
For the assessment of the WBC count, blood samples were collected every 2 h (+ 2, + 4, + 6, + 8, + 24 h). These samples were then stored in EDTA monovettes at room temperature (RT) until additional processing. WBC count was measured using an automated three-part differential haematology analyser (XP-300, Sysmex).
Collection of whole blood cells
For direct stabilisation of RNA of whole blood cells, the PAXgene® blood RNA collection system (Qiagen, Mississauga, Canada) was used. Of whole blood, 2.5 ml was drawn into PAXgene® blood RNA tubes and transferred to − 80 °C after storage at RT for 24 h, according to the manufacturer’s protocol.
RNA preparation and qRT-PCR
RNA of whole blood samples was isolated using the PAXgene® blood RNA Kit (Qiagen, Mississauga, Canada) according to the manufacturer’s protocol.
Real-time PCR (RT-PCR) with SYBR green fluorescent dye (Eurogentec, Verviers, Belgium) and the CFX96TM Real-Time System (Bio-Rad Laboratories GmbH, Munich, Germany) were used for quantification of genes. We reverse-transcribed 100 ng of total RNA into cDNA, which was amplified by 40 cycles of 95 °C for 15 s and 60 °C for 90 s with gene-specific primers (Supplementary Table) and normalized to ACTB (actin). Primer specificity was checked by Primer-BLAST and confirmed by size analysis of the PCR amplicons [56]. Expression was normalized to the respective untreated control of each blood donor individually and calculated with the 2 − ΔΔCT method for statistical analysis and set as an induction relative to the respective controls.
Statistical analyses
Statistical analyses were performed using GraphPad Prism 8.4.3 software (GraphPad, San Diego, CA) and PASW statistics (version 29; SPSS). All values are reported as the mean ± standard deviation. Subject data did not fulfil Gaussian distribution at several time points (BMI, school education) with low sample size, non-parametric calculations were used. Sociodemographic (age, BMI, school education) characteristics were compared between the two study groups using Mann–Whitney U and chi2 test. All gene expression data sets were analysed as repeated measurements of each single participant over time. Data sets were checked for Gaussian distribution of data points via statistical testing via the Anderson–Darling, D’Agostino-Pearson omnibus and Shapiro–Wilk test. Additionally, Gaussian distribution was confirmed via the QQ plot and analysed using the mixed-effects model. Non-Gaussian distributed data sets were transformed to Gaussian distributed data and analysed accordingly. For data comparison within treatment groups, Tukey’s multiple comparisons test was used. For data comparison between treatment groups, Sidak’s multiple comparisons test was used; Statistical significance is displayed as * = p < 0.05, ** = p < 0.01, *** = p < 0.001 or **** = p < 0.0001.
Results
Hypoxic priming leads to upregulation of LPS-induced body temperature and affects blood pressure in healthy men
Hypoxia — with or without the injection of LPS — expectedly led to changes in oxygen saturation. The injection of LPS increased the body temperature throughout the study protocol.
Exposure to hypoxia significantly reduced blood oxygen saturation at 1 to 4 h compared to baseline levels reaching an average SpO2 of 81.9 (± 0.7)%, below normal values of 98.8 (± 0.1)%, equivalent to about 50 mmHg or 6.7 kPa [6]. LPS treatment did not alter oxygen saturation. Notably, after hypoxic priming, oxygen saturation had returned to normal values before LPS administration.
Hypoxic exposure did not affect body temperature in healthy men, while LPS treatment resulted in a significant temperature increase at + 3 h post-injection compared to baseline levels. Interestingly, LPS administration after hypoxic priming induced a more pronounced temperature increase at 2 h and 3 h post-LPS injection compared to LPS controls before the hypoxic phase (Fig. 2).
Effect of hypoxia and LPS administration on blood oxygen saturation and body temperature. Oxygen saturation significantly decreased in the hypoxia chamber and decreased under hypoxia after LPS injection. Oxygen saturation remained unchanged after LPS administration with or without a prior hypoxic phase (10.5% O2, normobaric). Hypoxia itself had no effect on body temperature, while LPS injection significantly increased body temperature 3 h afterwards. Participants with a hypoxic phase prior to the LPS stimulation showed an even more significant increase in body temperature and inflammatory response. Data are means ± SD. Mixed-effects analysis; *p < 0.05, ***p < 0.001, ****p < 0.0001; n = 13–15
Effect of HOX-priming on LPS-induced changes in blood leukocytes in healthy men
Exposure to hypoxia had no impact on WBC count while LPS treatment resulted in a statistically significant increase in WBC at + 4 h post-injection compared to baseline levels (baseline 5622 ± 955 vs. LPS treatment 10.967 ± 1143, n < 0.0001). However, hypoxic priming did not alter the LPS-induced increase in WBC compared to LPS treatment alone (LPS treatment alone 10.967 ± 1143 vs. HOX-LPS 9953 ± 2276).
In vivohypoxic and inflammatory priming causes distinct changes in gene expression of whole blood cells
For the first time, we show that LPS injection induced a significant upregulation of HIF-1α mRNA in human blood cells within 4 h. Likewise, exposure to normobaric hypoxia (10.5% oxygen) induced HIF-1α mRNA at 4 h (Fig. 3). HIF-1α mRNA stayed significantly elevated in all three groups until 24 h. Further, the mRNA of the HIF-1 target gene glucose transporter 1 (GLUT-1) was significantly decreased 4 h after LPS treatment (also when followed by hypoxia), but not in subjects exposed to 4 h of hypoxic priming before LPS injection. In both groups, LPS-hypoxia and hypoxia-LPS mRNA for GLUT-1 remained significantly increased after 24 h (Fig. 3). Adrenomedullin (ADM) expression was not changed after LPS followed by hypoxia. However, hypoxic priming boosted the LPS effect three- to sevenfold (Fig. 3). Hypoxia-inducible factor 2α and other typical HIF targets such as pyryuvate-dehydrogenase-1 (PDK1) and vascular endothelial growth factor (VEGF) were not affected within the 8-h study duration (Supplemental Figure).
Effects of hypoxia and LPS on HIF and target gene expression of whole blood cells. Relative gene expression of whole blood cells, from blood samples of human subjects that were treated with a single E. coli lipopolysaccharide (LPS) injection (0.4 ng/kg) and a 4-h phase of exposure to hypoxia (normobaric, 10.5% O2) prior or after LPS injection. Shown are mRNA expression fold changes from hypoxia-inducible factor 1α (HIF1A), glucose transporter type 1 (GLUT-1/SCLA2) and adrenomedullin (ADM). Expression levels of mRNA were normalised to ACTB and are presented as 2 − (ΔΔCT) values (mean ± SD, mixed-effects analysis with repeated measures and Tukey’s or Sidak’s multiple comparisons test; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, n = 8–13)
Since some prolyl-hydroxylases (PHD) are HIF-1 targets, we determined mRNA regulation in whole blood. While PHD3 showed no significant changes, hypoxia as well as subsequent LPS in the HOX-LPS group led to significant reduction of PHD1 already after 2 h of hypoxia or 4 h LPS (Fig. 4). Interestingly, the response pattern of both groups (HOX-LPS vs. LPS-HOX) was similar independent of the order of stimuli. PHD2 mRNA upregulation was unaffected by hypoxic priming, but the hypoxic increase after prior LPS treatment (LPS-HOX group) became highly significant compared to baseline (Fig. 4).
Effects of hypoxia and LPS on the PHD gene expression of whole blood cells. Relative gene expression of whole blood cells from blood samples of human subjects that were treated with a single E. coli lipopolysaccharide (LPS) injection (0.4 ng/kg) and a 4-h phase of exposure to hypoxia (normobaric, 10.5% O2) prior or after LPS injection. Shown are mRNA expression fold changes from prolyl hydroxylases 1–3 (PHD1, PHD2, PHD3). Expression levels of mRNA were normalised to ACTB and are presented as 2 − (ΔΔCT) values (mean ± SD, mixed-effects analysis with repeated measures and Tukey’s or Sidak’s multiple comparisons test; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001; n = 8–13)
LPS increased the expression of the inflammatory cytokine Interleukin 6 (IL6) significantly, with a similar trend in tumour necrosis factor-alpha (TNFA). Interestingly, hypoxic priming led to a significant decrease of TNFA after 4 h but increased the following LPS effect (6 h time point). The expression of IL6 was no longer increased when LPS was administered after hypoxia (Fig. 5).
Effects of hypoxia and LPS on the inflammatory gene expression of whole blood cells. Relative gene expression of whole blood cells, from blood samples of human subjects that were treated with a single E. coli lipopolysaccharide (LPS) injection (0.4 ng/kg) and a 4-h phase of exposure to hypoxia (normobaric, 10.5% O2) prior or after LPS injection. Shown are mRNA expression fold changes from interleukin 6 (IL6) and tumour necrosis factor alpha (TNFA). Expression levels of mRNA were normalised to ACTB and are presented as 2 − (ΔΔCT) values (mean ± SD, mixed-effects analysis with repeated measures and Tukey’s or Sidak’s multiple comparisons test; *p < 0.05, **p < 0.01; n = 8–13)
Discussion
In our study, we investigated the crosstalk of hypoxic and inflammatory stimuli on peripheral blood cells in human subjects using an experimental endotoxemia model [1]. To our knowledge, this was the first study investigating possible in vivo hypoxic priming effects on immune activation. We used a cross-over protocol where healthy young males were challenged with an in vivo intravenous injection of lipopolysaccharide (LPS E. coli HOK364, 0.4 ng/kg) before or after exposure to in vivo hypoxia, simulated at an altitude of 4500 m (normobaric, 10.5% O2, 4 h).
Typical and well-studied symptoms with an onset 2 h after the in vivo LPS injection can include flu-like symptoms with fever, myalgia and headache [1, 36,37,38]. This was consistent with our observations. Exposure to hypoxia on the other hand is less studied under normobaric conditions but more under longer-lasting high-altitude (hypobaric) hypoxia [27, 41, 42]. Up to date, no other study focused on the effects of LPS-induced immune activation regarding the HIF pathway nor the potential influence of hypoxic priming on immune cell regulation. To close that gap, we analysed vital parameters of study participants and gene expression in peripheral blood cells.
Effects of LPS injection and in vivo hypoxia on blood oxygen saturation body temperature
Upon the challenge of participants with LPS, we observed elevated body temperature and increase in white blood cell counts, which all fits to previous reports in the literature [47, 53]. In vivo exposure to hypoxia leads to a reduction in blood oxygen saturation (SpO2) but no changes in body temperature.
Following a 3-h exposure to hypoxia, blood oxygen saturation declined from 98.8% to a mean of 83.1% corresponding to approximately 55 mmHg or 7.35 kPa [6]. Oxygen tension varies broadly within the human body, ranging from approximately 80 to 100 mmHg in arterial blood to tissue levels of 9–19 mmHg under physiological conditions. In most cells, the acute hypoxic response mediated by HIF activation will start at levels lower than the recorded PO2 values of around 55 mmHg corresponding to the above-mentioned measurements of SpO2 under hypoxia. Nevertheless, we identified significant effects on gene regulation in peripheral blood cells supporting our hypothesis of potential hypoxic priming effects even after short-term hypoxia [4, 6]. Obviously, hypoxia as applied in our protocol will lower PO2 values in all organs, which are passed by circulating leukocytes, and it is conceivable that leukocyte HIF accumulation will also take place during tissue passage. Moreover, HIF activation will also begin in the parenchyma of peripheral organs to release HIF-dependent gene products such as cytokines or growth factors.
Hypoxic priming has been shown to have complex effects on the immune response, particularly in the context of LPS-induced inflammation. Hempel et al. found that hypoxia can increase the release of the inflammatory cytokines IL-1 and TNF, potentially due to decreased prostaglandin E2 synthesis [29]. This suggests that hypoxic priming may exacerbate the pro-inflammatory effects of LPS. However, the specific mechanisms underlying this interaction are not yet fully understood.
Gene expression changes in whole blood upon in vivo exposure to hypoxia and LPS immunostimulation
Upon LPS injection, the mRNA levels of HIF1A in whole blood cells exhibited a significant increase 4 and 24 h post-LPS injection confirming previous reports from in vitro studies investigating the impact of LPS injections [50]. This increase in HIF-1A mRNA may have long-term effects on HIF activation in whole blood cells and leukocytes and boosts the cellular response to hypoxia when HIF protein becomes stable.
The expression of the HIF target gene ADM showed an interesting picture in whole blood cells. ADM is a multifaceted peptide that plays a significant role in the inflammatory response. It is produced and secreted by peripheral blood monocytes, and monocyte-derived macrophages, with its secretion increasing as these cells differentiate [35]. Furthermore, ADM production is stimulated by cytokines, growth factors and LPS in vascular smooth muscle cells, suggesting its involvement in endotoxin shock, atherosclerosis and inflammation [58]. ADM expression is most likely linked to HIF regulation with some independent regulatory mechanisms via HIF-1 and NF-κB through IL-1β as shown in in vitro models [22, 28, 30, 62]. Moreover, previous data on ADM expression in patients with sepsis had revealed a correlation between reduced HIF1A levels and lower ADM expression in peripheral leukocytes [50]. Herein, significant stimulation of ADM expression by LPS required hypoxic priming (Fig. 3). Thereby, it could be possible that hypoxic priming directly boosted the LPS effect or that the effect of the hypoxia is prolonged up to 8 h and becomes apparent only after a longer amount of time. Against a delayed reaction argues the fact, which hypoxic response mechanisms need to be and are known to be very fast-acting to ensure sufficient adaption to oxygen shortage. Nevertheless, even hypoxia alone led to a significant increase in ADM expression. Currently, it is unclear why LPS without prior hypoxia did not increase ADM mRNA despite elevated HIF1A mRNA levels.
In contrast, the HIF target PHD2 showed the expected amplification by LPS for the subsequent hypoxic stabilisation of HIF-1α protein resulting in increased HIF-dependent gene expression (Fig. 4). PHD2 is considered the predominant hydroxylase mediating the degradation of HIFα proteins [2]. Thus, it remains to be studied whether the LPS-boosted PHD2 accumulation can act through a negative feedback mechanism on HIFα proteins [17, 40]. The other studied HIF target GLUT-1 was found to be significantly downregulated upon challenge with LPS in whole blood cells but increased with the subsequent hypoxic stimulus (Fig. 3). Potentially, this response contributes to changes in energy metabolism as previously proposed [24, 31, 33, 51]. Interestingly, GLUT-1 expression was upregulated in both groups at 24 h compared to baseline conditions (Fig. 3). This differential response of HIF target genes to an inflammatory stimulus, which increases HIF1A mRNA and hypoxic activation of HIF-1, highlights the complexity in the regulation of HIF-1 as a transcription factor complex, controlled by hypoxia and inflammation [43, 48].
LPS treatment slightly increased the expression levels of the inflammatory cytokine TNFA in blood cells after 2 h. This rapid and acute immune activation aligns with findings from human studies utilizing the endotoxemia model, underscoring the systemic inflammatory response to LPS [1, 36, 38]. Interestingly, this LPS induction was affected by hypoxic priming, showing the increased upregulation of TNFA mRNA after exposure to hypoxia. In contrast, IL6 was substantially increased by in vivo exposure to LPS under normoxia but remained at basal levels after hypoxic priming, i.e. exposure to hypoxia before LPS injection significantly dampened IL6 expression.
Based on our findings, we anticipate alterations in protein expression, leading to subsequent effects on cellular behaviour, as evidenced by the observed rapid adaptation at the RNA level and enduring effects on mRNA levels (Fig. 3: 24 h: HIF-1A, GLUT, ADM; Fig. 4: PHD2). While there remains potential for translational regulation, our analysis indicates that for the genes investigated, changes in protein levels typically mirror alterations in transcription. However, our current study protocol has not permitted the demonstration of any discernible effects on the immune phenotypic behaviour or metabolic adaptation of the cells. Future investigations may incorporate extended observation periods or ex vivo challenge of immune cells in vitro to elucidate these aspects further.
Taken together, these observations indicate that in vivo hypoxia with 10.5% oxygen is sufficient to have an impact on inflammatory induced gene expression and potentially modulates immune reaction of whole blood cells and especially leukocytes. We assume that the RNA extracted from whole blood samples of subjects predominantly originates from leukocytes, with only a minimal fraction stemming from reticulocytes or red blood cells since red blood cells are lysed at the beginning of the blood sampling before RNA isolation and numerous publications demonstrate gene expression of leukocytes after PAXgene® RNA isolation. Remarkably, however, previous research indicates that mature red blood cells primarily contain microRNAs and mRNA transcripts associated with erythrocyte differentiation and function [10]. This supports the assumption that our observed changes in gene expression are primarily influenced by the abundance of leukocyte RNA in the sampled whole blood [10].
Numerous critical and chronic illnesses, including sepsis, acute respiratory distress syndrome, chronic obstructive pulmonary disease and sleep apnea, are linked to hypoxaemia with an inflammatory component [44]. The mechanisms involved in oxygen sensing and hypoxia signalling represent potential therapeutic targets for managing those and inflammatory diseases [12]. A substantial endeavour has been dedicated to the development of pharmacologic activators of HIF through the inhibition PHDs, commonly referred to as prolyl hydroxylase inhibitors (PHIs) [25, 52, 57]. These drugs have entered clinical use to ameliorate anaemia due to EPO deficiency. EPO is a classical HIF target, and therapy with PHIs successfully aims at increasing HIF-dependent expression in EPO-producing renal cells. However, leukocytes will also react to PHIs with HIF accumulation such as under hypoxia. It remains to be studied whether PHI treatment will have similar effects as hypoxic priming of leukocytes.
Limitations
Evidence suggests that high altitude-hypoxia affects blood leukocytes, for example, the redistribution of circulating T cells, but not B lymphocytes [14, 41, 42]. Additionally, reduced cytokine levels following prolonged exposure to high-altitude hypoxia over the course of days to weeks, particularly under unstimulated baseline conditions, have been reported [14, 41]. Controversially, in other studies, increased IL-6 levels were measured upon hypoxia in human blood, which was interpreted as facilitating angiogenesis through the induction of VEGF and EPO [27, 34, 39]. In the present study, we were, however, neither able to provide protein data from blood leukocytes nor changes in the immune cell phenotypic behaviour influenced by hypoxia.
When comparing our in vivo data to human high-altitude studies, it is important to consider that we specifically designed our study to explore acute short-term effects, with a maximum observation duration of 24 h. Consequently, our findings may not be directly comparable to those from studies conducted over weeks in hypobaric hypoxia.
Taken together, hypoxia and inflammation are integrated and present a multi-layered interplay, which depends highly on the order of occurring stimuli. Not only acute hypoxia but also HIF-increasing PHIs have the potential to shape immune reactions and immune cell–specific responses. Further investigations will elucidate this interplay in more detail on a molecular basis to better understand pathologies with inflammatory hypoxia.
Data Availability
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Andreasen AS, Krabbe KS, Krogh-Madsen R, Taudorf S, Pedersen BK, Moller K (2008) Human endotoxemia as a model of systemic inflammation. Curr Med Chem 15:1697–1705. https://doi.org/10.2174/092986708784872393
Berra E, Benizri E, Ginouves A, Volmat V, Roux D, Pouyssegur J (2003) HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1alpha in normoxia. EMBO J 22:4082–4090. https://doi.org/10.1093/emboj/cdg392
Bruick RK, McKnight SL (2001) A conserved family of prolyl-4-hydroxylases that modify HIF. Science 294:1337–1340. https://doi.org/10.1126/science.1066373
Chen Y, Gaber T (2021) Hypoxia/HIF modulates immune responses. Biomedicines 9. https://doi.org/10.3390/biomedicines9030260
Chen L, Qiu JH, Zhang LL, Luo XD (2012) Adrenomedullin promotes human endothelial cell proliferation via HIF-1alpha. Mol Cell Biochem 365:263–273. https://doi.org/10.1007/s11010-012-1267-1
Collins JA, Rudenski A, Gibson J, Howard L, O’Driscoll R (2015) Relating oxygen partial pressure, saturation and content: the haemoglobin-oxygen dissociation curve. Breathe (Sheff) 11:194–201. https://doi.org/10.1183/20734735.001415
Cormier-Regard S, Nguyen SV, Claycomb WC (1998) Adrenomedullin gene expression is developmentally regulated and induced by hypoxia in rat ventricular cardiac myocytes. J Biol Chem 273:17787–17792. https://doi.org/10.1074/jbc.273.28.17787
Dehne N, Brune B (2009) HIF-1 in the inflammatory microenvironment. Exp Cell Res 315:1791–1797. https://doi.org/10.1016/j.yexcr.2009.03.019
Devraj G, Beerlage C, Brune B, Kempf VA (2017) Hypoxia and HIF-1 activation in bacterial infections. Microbes Infect 19:144–156. https://doi.org/10.1016/j.micinf.2016.11.003
Doss JF, Corcoran DL, Jima DD, Telen MJ, Dave SS, Chi J-T (2015) A comprehensive joint analysis of the long and short RNA transcriptomes of human erythrocytes. BMC Genomics 16:952. https://doi.org/10.1186/s12864-015-2156-2
Ebert BL, Gleadle JM, O’Rourke JF, Bartlett SM, Poulton J, Ratcliffe PJ (1996) Isoenzyme-specific regulation of genes involved in energy metabolism by hypoxia: similarities with the regulation of erythropoietin. Biochem J 313(Pt 3):809–814. https://doi.org/10.1042/bj3130809
Eltzschig HK, Carmeliet P (2011) Hypoxia and inflammation. N Engl J Med 364:656–665. https://doi.org/10.1056/NEJMra0910283
Epstein AC, Gleadle JM, McNeill LA, Hewitson KS, O’Rourke J, Mole DR, Mukherji M, Metzen E, Wilson MI, Dhanda A, Tian YM, Masson N, Hamilton DL, Jaakkola P, Barstead R, Hodgkin J, Maxwell PH, Pugh CW, Schofield CJ, Ratcliffe PJ (2001) C. elegans EGL-9 and mammalian homologs define a family of dioxygenases that regulate HIF by prolyl hydroxylation. Cell 107:43–54. https://doi.org/10.1016/s0092-8674(01)00507-4
Facco M, Zilli C, Siviero M, Ermolao A, Travain G, Baesso I, Bonamico S, Cabrelle A, Zaccaria M, Agostini C (2005) Modulation of immune response by the acute and chronic exposure to high altitude. Med Sci Sports Exerc 37:768–774. https://doi.org/10.1249/01.mss.0000162688.54089.ce
Fandrey J (2004) Oxygen-dependent and tissue-specific regulation of erythropoietin gene expression. Am J Physiol Regul Integr Comp Physiol 286:R977-988. https://doi.org/10.1152/ajpregu.00577.2003
Fandrey J, Frede S, Jelkmann W (1994) Role of hydrogen peroxide in hypoxia-induced erythropoietin production. Biochem J 303(Pt 2):507–510. https://doi.org/10.1042/bj3030507
Fandrey J, Gorr TA, Gassmann M (2006) Regulating cellular oxygen sensing by hydroxylation. Cardiovasc Res 71:642–651. https://doi.org/10.1016/j.cardiores.2006.05.005
Firth JD, Ebert BL, Pugh CW, Ratcliffe PJ (1994) Oxygen-regulated control elements in the phosphoglycerate kinase 1 and lactate dehydrogenase A genes: similarities with the erythropoietin 3’ enhancer. Proc Natl Acad Sci U S A 91:6496–6500. https://doi.org/10.1073/pnas.91.14.6496
Fitzpatrick SF (2019) Immunometabolism and sepsis: a role for HIF? Front Mol Biosci 6:85. https://doi.org/10.3389/fmolb.2019.00085
Fluck K, Breves G, Fandrey J, Winning S (2016) Hypoxia-inducible factor 1 in dendritic cells is crucial for the activation of protective regulatory T cells in murine colitis. Mucosal Immunol 9:379–390. https://doi.org/10.1038/mi.2015.67
Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, Semenza GL (1996) Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol Cell Biol 16:4604–4613. https://doi.org/10.1128/MCB.16.9.4604
Frede S, Freitag P, Otto T, Heilmaier C, Fandrey J (2005) The proinflammatory cytokine interleukin 1beta and hypoxia cooperatively induce the expression of adrenomedullin in ovarian carcinoma cells through hypoxia inducible factor 1 activation. Cancer Res 65:4690–4697. https://doi.org/10.1158/0008-5472.CAN-04-3877
Frede S, Stockmann C, Freitag P, Fandrey J (2006) Bacterial lipopolysaccharide induces HIF-1 activation in human monocytes via p44/42 MAPK and NF-kappaB. Biochem J 396:517–527. https://doi.org/10.1042/BJ20051839
Greijer AE, van der Groep P, Kemming D, Shvarts A, Semenza GL, Meijer GA, van de Wiel MA, Belien JA, van Diest PJ, van der Wall E (2005) Up-regulation of gene expression by hypoxia is mediated predominantly by hypoxia-inducible factor 1 (HIF-1). J Pathol 206:291–304. https://doi.org/10.1002/path.1778
Haase VH (2011) (2021) Hypoxia-inducible factor-prolyl hydroxylase inhibitors in the treatment of anemia of chronic kidney disease. Kidney Int Suppl 11:8–25. https://doi.org/10.1016/j.kisu.2020.12.002
Haddad JJ, Harb HL (2005) Cytokines and the regulation of hypoxia-inducible factor (HIF)-1alpha. Int Immunopharmacol 5:461–483. https://doi.org/10.1016/j.intimp.2004.11.009
Hartmann G, Tschop M, Fischer R, Bidlingmaier C, Riepl R, Tschop K, Hautmann H, Endres S, Toepfer M (2000) High altitude increases circulating interleukin-6, interleukin-1 receptor antagonist and C-reactive protein. Cytokine 12:246–252. https://doi.org/10.1006/cyto.1999.0533
Hellwig-Burgel T, Rutkowski K, Metzen E, Fandrey J, Jelkmann W (1999) Interleukin-1beta and tumor necrosis factor-alpha stimulate DNA binding of hypoxia-inducible factor-1. Blood 94:1561–1567
Hempel SL, Monick MM, Hunninghake GW (1996) Effect of hypoxia on release of IL-1 and TNF by human alveolar macrophages. Am J Respir Cell Mol Biol 14:170–176. https://doi.org/10.1165/ajrcmb.14.2.8630267
Hofbauer KH, Schoof E, Kurtz A, Sandner P (2002) Inflammatory cytokines stimulate adrenomedullin expression through nitric oxide-dependent and -independent pathways. Hypertension 39:161–167. https://doi.org/10.1161/hy1201.097201
Hu CJ, Wang LY, Chodosh LA, Keith B, Simon MC (2003) Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation. Mol Cell Biol 23:9361–9374. https://doi.org/10.1128/MCB.23.24.9361-9374.2003
Huang LE, Gu J, Schau M, Bunn HF (1998) Regulation of hypoxia-inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway. Proc Natl Acad Sci U S A 95:7987–7992. https://doi.org/10.1073/pnas.95.14.7987
Kim JW, Tchernyshyov I, Semenza GL, Dang CV (2006) HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab 3:177–185. https://doi.org/10.1016/j.cmet.2006.02.002
Klausen T, Olsen NV, Poulsen TD, Richalet JP, Pedersen BK (1997) Hypoxemia increases serum interleukin-6 in humans. Eur J Appl Physiol Occup Physiol 76:480–482. https://doi.org/10.1007/s004210050278
Kubo A, Minamino N, Isumi Y, Katafuchi T, Kangawa K, Dohi K, Matsuo H (1998) Production of adrenomedullin in macrophage cell line and peritoneal macrophage. J Biol Chem 273:16730–16738. https://doi.org/10.1074/jbc.273.27.16730
Labrenz F, Wrede K, Forsting M, Engler H, Schedlowski M, Elsenbruch S, Benson S (2016) Alterations in functional connectivity of resting state networks during experimental endotoxemia - An exploratory study in healthy men. Brain Behav Immun 54:17–26. https://doi.org/10.1016/j.bbi.2015.11.010
Lasselin J, Benson S, Hebebrand J, Boy K, Weskamp V, Handke A, Hasenberg T, Remy M, Focker M, Unteroberdorster M, Brinkhoff A, Engler H, Schedlowski M (2020) Immunological and behavioral responses to in vivo lipopolysaccharide administration in young and healthy obese and normal-weight humans. Brain Behav Immun 88:283–293. https://doi.org/10.1016/j.bbi.2020.05.071
Lichte P, Grigoleit JS, Steiner EM, Kullmann JS, Schedlowski M, Oberbeck R, Kobbe P (2013) Low dose LPS does not increase TLR4 expression on monocytes in a human in vivo model. Cytokine 63:74–80. https://doi.org/10.1016/j.cyto.2013.04.014
Mazzeo RS, Donovan D, Fleshner M, Butterfield GE, Zamudio S, Wolfel EE (1985) Moore LG (2001) Interleukin-6 response to exercise and high-altitude exposure: influence of alpha-adrenergic blockade. J Appl Physiol 91:2143–2149. https://doi.org/10.1152/jappl.2001.91.5.2143
Metzen E, Berchner-Pfannschmidt U, Stengel P, Marxsen JH, Stolze I, Klinger M, Huang WQ, Wotzlaw C, Hellwig-Burgel T, Jelkmann W, Acker H, Fandrey J (2003) Intracellular localisation of human HIF-1 alpha hydroxylases: implications for oxygen sensing. J Cell Sci 116:1319–1326
Mishra KP, Ganju L (2010) Influence of high altitude exposure on the immune system: a review. Immunol Invest 39:219–234. https://doi.org/10.3109/08820131003681144
Oliver SJ, Macdonald JH, Harper Smith AD, Lawley JS, Gallagher CA, Di Felice U, Walsh NP (2013) High altitude impairs in vivo immunity in humans. High Alt Med Biol 14:144–149. https://doi.org/10.1089/ham.2012.1070
Palazon A, Goldrath AW, Nizet V, Johnson RS (2014) HIF transcription factors, inflammation, and immunity. Immunity 41:518–528. https://doi.org/10.1016/j.immuni.2014.09.008
Pham K, Parikh K, Heinrich EC (2021) Hypoxia and inflammation: insights from high-altitude physiology. Front Physiol 12:676782. https://doi.org/10.3389/fphys.2021.676782
Pugh CW, O’Rourke JF, Nagao M, Gleadle JM, Ratcliffe PJ (1997) Activation of hypoxia-inducible factor-1; definition of regulatory domains within the alpha subunit. J Biol Chem 272:11205–11214. https://doi.org/10.1074/jbc.272.17.11205
Ribatti D, Nico B, Spinazzi R, Vacca A, Nussdorfer GG (2005) The role of adrenomedullin in angiogenesis. Peptides 26:1670–1675. https://doi.org/10.1016/j.peptides.2005.02.017
Richardson RP, Rhyne CD, Fong Y, Hesse DG, Tracey KJ, Marano MA, Lowry SF, Antonacci AC, Calvano SE (1989) Peripheral blood leukocyte kinetics following in vivo lipopolysaccharide (LPS) administration to normal human subjects. Influence of elicited hormones and cytokines. Ann Surg 210:239–245. https://doi.org/10.1097/00000658-198908000-00018
Rius J, Guma M, Schachtrup C, Akassoglou K, Zinkernagel AS, Nizet V, Johnson RS, Haddad GG, Karin M (2008) NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature 453:807–811. https://doi.org/10.1038/nature06905
Rolfs A, Kvietikova I, Gassmann M, Wenger RH (1997) Oxygen-regulated transferrin expression is mediated by hypoxia-inducible factor-1. J Biol Chem 272:20055–20062. https://doi.org/10.1074/jbc.272.32.20055
Schafer ST, Frede S, Winning S, Bick A, Roshangar P, Fandrey J, Peters J, Adamzik M (2013) Hypoxia-inducible factor and target gene expression are decreased in patients with sepsis: prospective observational clinical and cellular studies. Anesthesiology 118:1426–1436. https://doi.org/10.1097/ALN.0b013e31828baa67
Schito L, Semenza GL (2016) Hypoxia-inducible factors: master regulators of cancer progression. Trends Cancer 2:758–770. https://doi.org/10.1016/j.trecan.2016.10.016
Schönberger T, Fandrey J, Prost-Fingerle K (2021) Ways into understanding HIF inhibition. Cancers (Basel) 13 https://doi.org/10.3390/cancers13010159
Schultz MJ, van der Poll T (2002) Animal and human models for sepsis. Ann Med 34:573–581. https://doi.org/10.1080/078538902321117797
Semenza GL, Roth PH, Fang HM, Wang GL (1994) Transcriptional regulation of genes encoding glycolytic enzymes by hypoxia-inducible factor 1. J Biol Chem 269:23757–23763
Shweiki D, Itin A, Soffer D, Keshet E (1992) Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 359:843–845. https://doi.org/10.1038/359843a0
Spandidos A, Wang X, Wang H, Seed B (2010) PrimerBank: a resource of human and mouse PCR primer pairs for gene expression detection and quantification. Nucleic Acids Res 38:D792-799. https://doi.org/10.1093/nar/gkp1005
Sugahara M, Tanaka T, Nangaku M (2017) Prolyl hydroxylase domain inhibitors as a novel therapeutic approach against anemia in chronic kidney disease. Kidney Int 92:306–312. https://doi.org/10.1016/j.kint.2017.02.035
Sugo S, Minamino N, Shoji H, Kangawa K, Kitamura K, Eto T, Matsuo H (1995) Interleukin-1, tumor necrosis factor and lipopolysaccharide additively stimulate production of adrenomedullin in vascular smooth muscle cells. Biochem Biophys Res Commun 207:25–32. https://doi.org/10.1006/bbrc.1995.1148
van Uden P, Kenneth NS, Webster R, Muller HA, Mudie S, Rocha S (2011) Evolutionary conserved regulation of HIF-1beta by NF-kappaB. PLoS Genet 7:e1001285. https://doi.org/10.1371/journal.pgen.1001285
Wang GL, Semenza GL (1993) Characterization of hypoxia-inducible factor 1 and regulation of DNA binding activity by hypoxia. J Biol Chem 268:21513–21518
Watts ER, Walmsley SR (2019) Inflammation and hypoxia: HIF and PHD isoform selectivity. Trends Mol Med 25:33–46. https://doi.org/10.1016/j.molmed.2018.10.006
Zaks-Zilberman M, Salkowski CA, Elsasser T, Cuttitta F, Vogel SN (1998) Induction of adrenomedullin mRNA and protein by lipopolysaccharide and paclitaxel (Taxol) in murine macrophages. Infect Immun 66:4669–4675. https://doi.org/10.1128/IAI.66.10.4669-4675.1998
Zhang Y, Xu Y, Ma J, Pang X, Dong M (2017) Adrenomedullin promotes angiogenesis in epithelial ovarian cancer through upregulating hypoxia-inducible factor-1alpha and vascular endothelial growth factor. Sci Rep 7:40524. https://doi.org/10.1038/srep40524
Acknowledgements
The authors would like to thank all participants of the study. Further thanks goes to all involved technical assistants in the involved institutes.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was partly funded by centre grants of the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) project number 316803389—SFB 1280 (TP A18 to M.S.). Oliver Witzke is supported by an unrestricted grant of the Rudolf-Ackermann-Stiftung (Stiftung für Klinische Infektiologie).
Author information
Authors and Affiliations
Contributions
Conceptualization, T.S., B.T., O.W., J.F. and M.S.; methodology, T.S., B.T., M.J. and J.F.; investigation, T.S., B.T., M.J., T.H-G. and A.F.; resources, J.F., M.S.; writing—original draft preparation, T.S.; writing—review and editing, T.S., M.J., T.H-G., A.F., M.S. and J.F.; visualization, T.S.; supervision, B.T., J.F. and M.S.; project administration, B.T., J.F. and M.S.; funding acquisition, J.F and M.S.. All authors have reviewed and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Further official approval was obtained from the responsible Ethics Committee of the University Hospital Essen (No. 18–8258-BO). The study was conducted according to the principles of the Declaration of Helsinki. Boards and guidelines followed must be named when applicable.
Consent to participate
Written and informed consent was obtained from each enrolled individual human subject in the study.
Conflict of interest
The other authors have nothing to disclose and declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• In vivo hypoxia shapes inflammatory response.
• Human whole blood cells are sensitive to normobaric hypoxia.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schönberger, T., Jakobs, M., Friedel, AL. et al. Exposure to normobaric hypoxia shapes the acute inflammatory response in human whole blood cells in vivo. Pflugers Arch - Eur J Physiol (2024). https://doi.org/10.1007/s00424-024-02969-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00424-024-02969-2