Abstract
The disposal of ammonia, the main proton buffer in the urine, is important for acid–base homeostasis. Renal ammonia excretion is the predominant contributor to renal net acid excretion, both under basal condition and in response to acidosis. New insights into the mechanisms of renal ammonia production and transport have been gained in the past decades. Ammonia is the only urinary solute known to be produced in the kidney and selectively transported through the different parts of the nephron. Both molecular forms of total ammonia, NH3 and NH4+, are transported by specific proteins. Proximal tubular ammoniagenesis and the activity of these transport processes determine the eventual fate of total ammonia produced and excreted by the kidney. In this review, we summarized the state of the art of ammonia handling by the kidney and highlighted the newest processes described in the last decade.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Respiratory (CO2 production) and metabolic processes (food intake and cellular metabolism) continuously add acid to the body, challenging acid–base balance. The adjustment of extracellular pH in a narrow range from 7.36 to 7.44 is critical for cellular and organ performances. For this reason, disorders of acid–base homeostasis are associated with the worsening of kidney function and a higher morbidity and mortality in patients with chronic kidney disease (CKD) [3]. Moreover, it has been shown in the general population under physiological conditions that polymorphisms in genes involved in renal ammonia transport and metabolism are associated with values of urine pH and may contribute to the pathogenesis of kidney diseases associated with acid retention [22]. Extracellular pH affects bone density and stability, and mild chronic metabolic acidosis has been suspected to contribute to osteopenia and osteoporosis [1, 61]. Rickets and osteomalacia are often observed in patients with inborn syndromes of renal tubular acidosis. Extracellular acidosis affects skeletal muscle metabolism and induces a catabolic state [3].
The kidney is one of the key organs controlling and maintaining a normal systemic acid–base status, through three mechanisms: the reabsorption of filtered bicarbonate, the de novo generation of ammonium (NH4+) and bicarbonate, and the excretion of net acid, mostly under the form of ammonium. Amino acid metabolism in the standard non-vegan or non-vegetarian Western diet is an acidifying diet rich in animal protein and results in endogenous acid production of around 0.8 to 1.0 mEq/kg/day [12]. To replenish the body’s bicarbonate content, the proximal tubule produces ammonium, which is secreted by the collecting duct (CD) in the form of ammonia and protons to form ammonium in the urine. Dysfunction of either of these two steps leads to proximal (pRTA) and distal (dRTA) renal tubular acidosis, respectively. Ammonia excreted in the final urine as NH4+ leads to the formation of a new equimolar bicarbonate, while ammonia returning to the systemic circulation via the renal vein is metabolized by the liver to urea and glutamine [57].
Biochemistry of ammonia
Under biological conditions, total ammonia (t-ammonia) exists both as ammonia (NH3) and its protonated form ammonium (NH4+). The relative concentration of each of these forms in bodily fluids is driven by the buffering reaction NH3 + H+– > NH4+. The abundance of t-ammonia makes NH3 the main H+ buffer in the urine.
In the body, the pKa of this reaction is around 9.2. Thus, under physiological conditions, as the biological fluids exhibit a pH below the pKa, most of the t-ammonia exists as NH4+; for example, NH3 accounts for a mere 1% of the t-ammonia in serum at pH 7.4 and is only present in trace amounts in urine where pH is generally below 6 [49].
Overview of ammonia transport in the nephron
Four decades ago, micropuncture and in vivo microperfusion studies assessed the fate of ammonia in the kidney. T-ammonia is produced and secreted into the luminal fluid at the level of the proximal tubule [19, 20, 45, 47]. In the loop of Henle, and more predominantly, in the medullary thick ascending limb, t-ammonia is reabsorbed and concentrated by countercurrent multiplication, inducing an interstitial ammonia concentration gradient that increases from the cortex to the outer medulla and then again to the inner medulla [91, 106].
Finally, ammonia is secreted by the adjacent collecting duct to reach final urinary t-ammonia excretion rate [102]. Production, transport, and final excretion of t-ammonia along the nephron increase in metabolic acidosis in the rat kidney (Fig. 1) [100, 102].
Urinary t-ammonia generation and transport in the nephron. NH3/NH4+ (t-ammonia) is produced essentially from glutamine metabolism into the proximal tubular (PT) cells. T-ammonia is secreted into the luminal fluid at the level of PT. In the loop of Henle, and more predominantly, in the medullary thick ascending limb (TAP), t-ammonia is reabsorbed and concentrated by counter-current multiplication which induces an interstitial ammonia concentration gradient that increases from cortex to outer medulla to inner medulla. There, sulfatides (S) accumulate in kidney interstitium where they can reversibly bind NH4+. Finally, ammonia (NH3) is secreted by the adjacent collecting duct, to reach final urinary t-ammonia excretion rate. Created with BioRender.com
Ammonia metabolism and reabsorption in the proximal part of the nephron
Renal glutamine transport and ammonia production
Ammonia is a highly toxic compound, particularly for central nervous system cells. Concentration in plasma is low, in the micromolar range (https://www.merckmanuals.com/professional/resources/normal-laboratory-values/normal-laboratory-values). Unlike other urine constituents, most of the t-ammonia found in urine does not stem from plasma content filtered by the glomerulus but is rather produced within the nephrons by the proximal tubular cell. The rate of ammoniagenesis is highly dependent on acid–base status. In the context of a Western diet, the absence or deficiency of one of the protagonists of ammonia production, metabolism, and transport in the proximal tubule can lead to the retention of non-volatile acids in the body and the development of metabolic acidosis.
NH4+ is generated mainly by the metabolism of amino acids such as glutamine, which results in the equimolar formation of bicarbonate transported in the blood while ammonium is secreted in the pro-urine (Fig. 2). Glutamine, which is a small molecule, is entirely filtered by the glomerulus and taken up by the proximal tubule [100]. In the proximal tubule, glutamine is transported into epithelial cells at least in part by the amino acid cotransporters B°AT1 (SLC6A19) and SNAT3 (SLC38A3) at the apical and basolateral poles of the cell, respectively [27, 84]. Glutamine is then taken up by the mitochondria via yet unknown transporters. In mitochondria, glutamine is converted into one α-ketoglutarate and 2 NH4+ molecules by the action of phosphate-dependent glutaminase (PDG) and glutamate dehydrogenase (GDH). α-Ketoglutarate is metabolized as part of the tricarboxylic acid (TCA) cycle, generating malate which is metabolized to form phosphoenolpyruvate (PEP) by the mitochondrial phosphoenolpyruvate carboxykinase (m-PEPCK or PCK2) or secreted into the cell cytoplasm through the mitochondrial membrane. In the cytoplasm, malate metabolism leads to the production of a bicarbonate molecule after the action of malate dehydrogenase and cytoplasmic phosphoenolpyruvate carboxykinase (c-PEPCK or PCK-1) to form PEP ([109], for review [56, 123]). The importance and rate-limiting effect of PCK1 has been highlighted recently by the study of PCK1 knockout mice. Even though PCK1 acts in the cytoplasm of proximal tubular cells, its disruption leads to severe dysfunction of the mitochondria, an inability of the mice to fight against an acid load and the development of metabolic acidosis due to a decrease of ammoniagenesis [109]. PCK1 has also been associated with diabetic nephropathy in humans [126]. PEP can then be metabolized to form pyruvate and undergo the TCA cycle again or be used by the proximal cell for gluconeogenesis [123]. T-ammonia formed during the metabolism of glutamine leaves the mitochondria for the cell cytoplasm. A member of aquaporin family, AQP8, has been first localized in the mitochondrial membrane of rat kidney and suggested as NH3 channel involved in ammonia diffusion from the mitochondria to the cytoplasm of proximal tubular cells [33, 83]. Indeed, in addition to its ability to transport H2O, mouse, rat, or human AQP8 when heterologously expressed in cell lines has been shown to allow NH3 diffusion [58, 77, 96]. In the human renal proximal cell line, HK-2, which expresses AQP8 in its inner mitochondrial membrane, the knockdown of AQP8 decreased ammonia secretion by these cells. The authors also demonstrated that mitochondrial AQP8 expression increased in acid-loaded rats during chronic metabolic acidosis, supporting a role of AQP8 in the kidney’s response to an acid challenge [83]. These data support a role for AQP8 in native proximal tubule mitochondrial T-ammonia transport. However, the physiological relevance of AQP8 role in ammonia handling by the proximal tubule is still questioned by the mild phenotype of AQP8 knockout mice [128]. Indeed, AQP8 knockout mice, which had no defect under baseline conditions, showed increased renal ammonia excretion during experimental metabolic acidosis created by chronic NH4Cl challenge, and no change in blood pH and blood pCO2 compared with wild-type mice [128]. Further research is therefore needed to resolve these contradictions and assess a possible compensatory effect of other aquaporins/transporters in t-ammonia export out of the proximal cell mitochondria [82, 83].
T-ammonia generation and transport in the proximal tubule (PT) cells. Glutamine is carried into the PT epithelial cells by the amino acid cotransporters B°AT1 and SNAT3. In the PT cells, glutamine is taken up by the mitochondria and processed to one α-ketoglutarate and 2 NH4+ molecules by the action of phosphate-dependent glutaminase (PDG) and glutamate dehydrogenase (GDH). α-Ketoglutarate metabolized in the tricarboxylic acid (TCA) cycle results in the generation of malate which is secreted into the cell cytoplasm through the mitochondrial membrane. In the cytoplasm, malate metabolism results in the generation of one bicarbonate molecule after the action of malate dehydrogenase and cytoplasmic phosphoenolpyruvate carboxykinase (c-PEPCK or PCK-1) to form phosphoenolpyruvate (PEP). PEP can then be metabolized to form pyruvate and undergo again TCA cycle or used by the proximal cell for gluconeogenesis. The newly formed NH4+ is leaving the mitochondria via the aquaporin isoform 8 (AQP8). The t-ammonia (NH3/NH4+) formed in PT cells is secreted into the tubular lumen by diffusion across the apical membrane and by active transport, mainly via the Na/H exchanger NHE3 by proton substitution or via a barium-sensitive K channel. The bicarbonate (HCO3−) formed is transported across the basolateral plasma membrane by the Na-bicarbonate/carbonate (HCO3c−/CO32−) cotransporter NBCe1 and transferred to the bloodstream. The activity of the Kir4.2 potassium channel hyperpolarizes the plasma membrane to enable activation of carbonate transport by the NBCe1 transporter. This process lowers the intracellular pH required for the proper functioning of ammoniagenic enzymes and ammonium transporters. Created with BioRender.com
Ammonia transport in the proximal tubule
Ammonium formed in proximal tubular cells is secreted into the tubular lumen by diffusion across the apical membrane and by active transport mainly through the Na/H exchanger NHE3 (SLC9A3) by protons substitution, or through a barium-sensitive K+ channel [48]. NH4+ and K+ ions have almost identical biophysical characteristics, which allows NH4+ ions to be transported by theoretically all K+ transporters in epithelial cells [43, 121]. In parallel, the bicarbonate formed during malate metabolism is transported across the basolateral plasma membrane mainly by the Na-bicarbonate/carbonate (HCO3−) cotransporter NBCe1 (SLC4A4) and transferred into the bloodstream with a stoichiometry of 1 Na+ for 3HCO3− [10, 72]. Recently, it has been reported by Lee and colleagues in a mechanistic study that NBCe1 transports the main blood H+ buffer under its CO32− form [72]. So far, no other technical approach, such as structural studies, has been able to assess this crucial question. The recent crystal structure of NBCe1 at 3.9 Å could not determine with precision the exact substrate for NBCe1 coupled to Na+ [60]. Further research is needed to determine the stoichiometry of this transport, as the 1:3 stoichiometry cannot be maintained with the CO32− form [60, 69, 72]. The picture of ammonia handling by the proximal tubule has recently been better extended by the demonstration of the role of the potassium channel Kir4.2 as a powerful determinant of ammoniagenesis as well as of ammonia and bicarbonate transport by the proximal tubule [4]. In male mice, deletion of Kir4.2 causes metabolic acidosis via depolarization of the basolateral plasma membrane and impairment of bicarbonate handling by the NBCe1 transporter. This process increases intracellular pH and, consequently, alters the expression of ammoniagenic enzymes and ammonium transporters (Fig. 2) [4].
Transport in the thick ascending limb and concentration in renal medulla
The next site where significant transport of t-ammonia takes place is the loop of Henle and where most t-ammonia is reabsorbed in the thick ascending limb (TAL). Part of the reabsorbed t-ammonia is passively secreted into the thin descending limb [36], a phenomenon that plays a role in countercurrent multiplication and creates a cortico-papillary concentration gradient of NH3/NH4+ (Fig. 1) that allows NH3/NH4+ capture and secretion into the adjacent collecting duct (Fig. 3) [13, 43]. The magnitude of the concentration gradient increases with acidosis and water deprivation and drastically decreases during alkali load and furosemide infusion [91, 93]. The inability to create or maintain a cortico-papillary gradient of NH3/NH4+ can presumably be responsible for the progressive decrease in ammonium excretion that characterizes chronic kidney disease [18]. However in conditions where this gradient is disrupted, the body can still compensate for the lack of ammonia reabsorption in the TAL by increasing the urine output and thus ammonium supply to collecting duct cells, as has been observed in NHE4 and NBCn1 knockout mice [16, 89].
T-ammonia reabsorption in the thick ascending limb (TAL) cells and secretion in the collecting duct cells work in concert to facilitate NH4+ excretion in the urine. In the TAL, NH4+ is reabsorbed essentially by the Na+-K+-2Cl− cotransporter isoform 2, NKCC2 and to a lesser extent, a barium sensitive K+ channel. Intracellular t-ammonia leaves the cell at the basolateral side via a direct NH4+ transport, the Na+/(H+/NH4+) exchanger NHE4, and an indirect process of NH3 transport by bicarbonate buffering involving the electroneutral cotransporter Na+-HCO3− NBCn1. In, the type A IC, t-ammonia is taken up as NH4+ by the Na+/(K+/NH4+)-ATPase or the cotransporter Na+-K+-2Cl− isoform 1 NKCC1 or NH3 by the Rhesus (Rh) glycoproteins Rh C glycoprotein (Rhcg) or Rh B glycoprotein (Rhbg) thanks to the cortico-papillary gradient of NH3/NH4+. Within the cell cytoplasm, carbonic anhydrase II (CAII) facilitates the basolateral efflux of HCO3− by activating the Cl−/HCO3− exchangers AE1 and SLC26A7 which allows the generation of H+ in the cytosol and enable parallel H+ and NH3 secretions across the apical plasma membrane by, respectively, Rhcg and primarily, the multimeric protein H+-ATPase or the electroneutral H+,K+-ATPase. Created with BioRender.com
Luminal uptake
In the TAL, most of NH4+ reabsorption occurs transcellularly. The main transporter enabling apical uptake of ammonia from the tubular lumen is the Na+-K+-2Cl− cotransporter isoform 2, NKCC2 (SLC12A1). Inhibition of NKCC2 by furosemide suppresses NH4+ reabsorption in the ex vivo microperfused rat medullary TAL [45]. The NH4+ ion enters the cells by substituting for K+ (Fig. 3) [39, 43, 66]. As the NH4+ and the K+ ions compete at the same protein site, modulations of luminal K+ concentration also modify TAL NH4+ reabsorption. Thus, a lower extracellular potassium concentration increases ammonia reabsorption, and a higher potassium concentration reduces it [40, 41]. NKCC2 protein activity is modulated mainly by phosphorylation and trafficking [42, 86]. However, detailed knowledge of its role in the TAL response to ammonia handling remains incomplete. In addition to NKCC2, the activity of a luminal barium sensitive K+ channel has been documented in the ex vivo microperfused TAL [120]. The physiological importance of this channel in ammonia transport appears to be limited as the pharmacological inhibition of NKCC2 by furosemide almost abolishes ammonia reabsorption in the ex vivo microperfused TAL.
Basolateral exit
To complete ammonia reabsorption, intracellular ammonia must be transported across the basolateral membrane of TAL cells. Ex vivo microperfusion studies on TAL have demonstrated that 1 mM amiloride or 50 µM EIPA, an amiloride analogue, in the peritubular fluid drastically reduced ammonia reabsorption [44]. More than a decade later, two different transporters, the electroneutral Na+-HCO3− cotransporter NBCn1(SLC4A7) and the Na+/H+ exchanger NHE4 (SLC9A4) operating as a Na+/NH4+ exchanger, were shown to be involved in this final step of ammonia transport across the TAL (for review [59]).
NBCn1, first cloned from the rat smooth muscle cell [28], has been functionally identified in the basolateral membrane of the rat medullary thick ascending limb cells and localized in the rat and mouse TAL and mouse medullary collecting duct cells [8, 15, 111]. Being electroneutral, NBCn1 acts as a base loader, drawing sodium and bicarbonate into the cell. There, bicarbonate buffers a hydrogen ion from NH4+, releasing NH3 that then diffuses across the basolateral membrane [89]. The abundance of NBCn1 protein in the kidney and its activity in the ex vivo microperfused medullary TAL cells increase significantly during chronic metabolic acidosis induced by NH4Cl loading in rats and mice [71, 88, 89]. However, although its expression is controlled by acid–base status, the role of NBCn1 in ammonium reabsorption by the TAL and ammonium excretion in urine has been unclear until the recent phenotyping of NBCn1 knockout mice [89]. When exposed to NH4Cl in drinking water, NBCn1 knockout mice showed an abnormal adaptation to the acid load compared to wild-type mice. In TAL cells, net ammonia reabsorption was significantly reduced in NBCn1 knockout mice loaded with acid for 1 day [89]. Basolateral Na/H activity was maximally elevated under control and plateaued under acid loading compared with wild-type TAL [89]. The basolateral membrane of the medullary TAL cells expresses two distinct Na+/H+ exchangers: the ubiquitous NHE1 isoform and the TAL-specific NHE4 isoform [26]. NHE4 is highly resistant to amiloride derivatives: in purified basolateral vesicles, the IC50 value for ethyl isopropyl amiloride (EIPA) has been calculated to be 2.5 µM, contrasting with the high sensitivity of NHE1 (IC50 = 11 nM) [26]. Furthermore, in PS120 fibroblasts transfected with NHE4 isoform, 1 mM amiloride inhibits by 80% the NHE4-dependent Na/H activity [9]. Of note, when Olsen et al. used 1 mM amiloride to inhibit the basolateral Na/H activities, they were unable to distinguish between NHE1 and NHE4 activities [9, 16, 24]. NHE1 and NHE4 also differ in their respective sensitivity to intracellular pH (pHi), NHE4 being active at a lower pHi than NHE1 (pK values 6.21 and 6.75, respectively) [26, 90]. Medullary TAL cells have an intracellular pH around 6.9–7 when studied in the absence of extracellular ammonium, and NHE4 is probably almost inactive. When medullary TAL cells absorb ammonium, their intracellular pH reduces to about 6.5–6.6 [120], which is expected to activate NHE4.
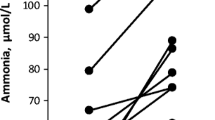
NHE4 mRNA expression and protein activity are increased during metabolic acidosis in mice and rats, respectively [16]. The direct demonstration that NHE4 is important for the basolateral exit of NH4+ has been provided by the study of the phenotype of NHE4 knockout mice [16]. On a control diet, NHE4 knockout mice exhibit a compensated, hyperchloremic metabolic acidosis with elevated excretion of ammonium in the urine compared to their littermate wild type [16]. However, the renal net acid excretion is not different from that of normal mice, revealing an inability to excrete more acid as expected during metabolic acidosis. It is noteworthy that the urinary pH of NHE4 knockout mice was lower than that of wild-type mice, suggesting that (1) the absence of NHE4 does not impair hydrogen ion secretion in the collecting duct and (2) the NHE4 knockout mice may have developed a compensatory increase in diffusion gradient of NH3 by the adjacent collecting duct to support final t-ammonia excretion, likely caused by an increased activity of NH3 channels such as Rhcg or Rhbg and the multimeric protein H-ATPase of the A-IC. In addition, the lower urinary pH could facilitate ammonia diffusion across the collecting duct epithelium. However, these hypotheses have not been investigated in NHE4 knockout mice. When subjected to chronic dietary acid loading, NHE4 knockout mice show worsening metabolic acidosis, whereas wild-type mice recover from acidosis [16]. The most striking difference between wild-type and NHE4 knockout mice is the latter’s inability to properly increase urinary ammonium excretion (Fig. 3). Good et al. emphasized the importance of medullary ammonia accumulation, and hence ammonia uptake in the loop of Henle, as the main determinant of ammonia secretion in the internal medullary collecting duct in vivo [46]. In agreement, NHE4 knockout mice as NBCn1 knockout mice have an impaired ability to build their cortico-papillary concentration gradient of NH3/NH4+ (Fig. 3). This is probably because medullary TAL cells reabsorb much less ammonia in the absence of NHE4 than in its presence, although NBCn1 could partially compensate.
Renal interstitium: role of sulfatides in ammonium handling
Sulfatides are a subclass of anionic glycosphingolipids, which accumulate in mammalian kidney with a higher concentration in distal medullary nephron [78]. Disturbances in renal sulfatide content or metabolism have been associated with a large panel of kidney and metabolic diseases [80]. For instance, abnormalities in the glycosphingolipid sulfatide content and activity have been reported in a mouse model of polycystic kidney disease [30], a condition known to progress towards the development of metabolic acidosis in rats [21]. Using molecular genetics and cellular and physiological approaches in a mouse model of disrupted sulfatide synthesis in the kidney, Stettner et al. demonstrated that sulfatides are required for renal excretion of ammonia. When subjected to acidic loading, mice deficient in renal sulfatide synthesis has impaired ammonia excretion with lower ammonia accumulation in the papilla and develop chronic hyperchloremic metabolic acidosis. Sulfatides are highly charged anion glycosphingolipids that may reversibly bind NH4+ in the renal interstitium (Fig. 1) [105]. Sulfatides, probably through their ability to reversibly bind interstitial NH4+, are also a key player in renal ammonia handling, urinary acidification, and acid–base homeostasis. However, the precise mechanisms of the disruption of the cortico-papillary ammonia/ammonium gradient remain unknown and need further research to precisely decipher the role of sulfatides in this process.
Fine-tuning of acid excretion in the distal nephron and the collecting duct
The ultimate fine-tuning of renal acid excretion takes place in the distal part of the nephron
Intercalated cells, which are highly specialized in transepithelial acid and base transport, are present in the late distal convoluted tubule (DCT2), connecting tubule (CNT), and collecting duct (CD) from the cortex (CCD) to the inner medulla (IMCD) [65]. Roughly, 40% of the cells in CNT, CCD, and outer medulla (OMCD) are IC. IC gradually disappear from the proximal to the last part of IMCD to be virtually absent in the papilla [2]. At least, two intercalated cells subtypes, type A and non-type A, can be recognized and differ by lateralization of the multimeric plasma membrane H+-ATPase and expression of various proteins involved in acid and base transport [65]. Type A intercalated cells express the vacuolar H+-ATPase at the apical membrane and the Cl−/HCO3− exchanger AE1 at the basolateral membrane. They are typically involved in proton and ammonium secretion and are expressed from DCT2 to IMCD. The non-type A intercalated cells express the vacuolar ATPase either at the basolateral membrane (also called type B) or at both basolateral and apical membranes (also called non-type A non-type B), and the Cl−/HCO3− pendrin exchanger at the luminal membrane. Non-type A intercalated cells are mainly expressed in cortical segments, from DCT2 to CCD [65]. Initial studies on isolated and ex vivo microperfused rabbit and rat collecting ducts have shown that the transport of ammonium is predominant in OMCD and IMCD, where only type A intercalated cells are present, and this is tightly regulated by acid–base status (Fig. 3) [95]. In metabolic acidosis, a marked increase in ammonia secretion is also found in the CNT and CCD [67].
The molecular mechanisms of t-ammonia secretion were poorly understood until recent years. The importance of acid secretion in the collecting duct to overall systemic acid–base balance is highlighted by several rare inherited disorders affecting acid–base transport proteins from the collecting duct. Pathogenic variants in the B1 and a4 subunits of H+-ATPase (ATP6V1B1, ATP6V0A4) and in AE1 (SLC4A1) have been identified as the cause of distal renal tubular acidosis (dRTA) almost two decades ago [62]. More recently mutations of the transcription factor FoXI1 and of the scaffolding protein WDR72, which are also expressed in the collected duct, have been causally linked to dRTA in humans [34, 94].
Basolateral uptake
Na+,K+-ATPase was the first discovered plasma membrane protein complex that was directly involved in NH4+ uptake by the collecting duct cells [70]. NH4+ binds to the K+ site and enables active transport of Na+ and NH4+. In IMCD, basolateral NH4+ uptake mediated by the Na+,K+-ATPase is critical for ammonia and H+ secretion, particularly in chronic hypokalemia [115, 117, 119]. Indeed, during hypokalemia, the drop in interstitial K+ concentration allows increased NH4+ binding to the K+ site of the Na+,K+-ATPase, thereby increasing basolateral uptake of NH4+ [117].
Expression of the Na+-K+-2Cl− isoform 1 NKCC1 (SLC12A2) has also been observed at the basolateral membrane of A-IC [118]. As with NKCC2 in the TAL, NKCC1 in the ex vivo microperfused rat OMCD can transport NH4+ by substitution with K+. However, its contribution to H+ secretion appears to be limited [116]. This observation has been confirmed in Slc12a2 knockout mice which do not develop any defects in renal acid handling [68, 118].
Studies evaluating the contribution of Rhesus (Rh) glycoproteins as ammonia/ammonium channels have significantly altered our understanding of collecting duct ammonia transport (for review [56, 112, 113, 122, 123]). Two Rh glycoproteins, Rh C glycoprotein (Rhcg, SLC42A3) and Rh B glycoprotein (Rhbg, SLC42A2), have been identified in the renal collecting duct cells. In humans, RhCG appears to be the major ammonia channel, while in mice and rats, Rhbg has been also localized at the basolateral membrane of IC and principal cells [17, 65, 92]. In rodents, Rhcg is present in the apical and basolateral membrane in type A intercalated and principal cells in the distal nephron, including DCT, CNT, CCD, and OMCD. RhCG is detected in the apical plasma membrane of non-A, non-B intercalated cells, but is not present in type B intercalated cells [13, 32, 110]. Rhcg has been identified as a direct NH3 channel [7], whereas Rhbg may transport ammonia in the form of NH3 and NH4+ [23]. Rhcg plays a major role in the basolateral ammonia uptake as illustrated by the drastically reduced diffusion of ammonia across the basolateral membrane of ex vivo microperfused CCD from Rhcg knockout mice compared to wild type [13]. Both Rhcg and Rhbg expressions are upregulated during chronic metabolic acidosis in mice [98]. However, the importance of Rhbg in t-ammonia transport is more controversial than that of Rhcg [7, 13, 73, 74] as Rhbg knockout mice exhibit either no or a much milder phenotype [5, 6, 25]. Rhbg may have a specific function in the defense against acidosis during hypokalemia [5, 50].
Carbonic anhydrase and HCO3 − secretion
In addition to its primary role in bicarbonate production, the carbonic anhydrase II (CAII) also contributes to ammonia secretion in type A intercalated cells. Inhibiting carbonic anhydrase blocks ammonia secretion in isolated perfused OMCD [116]. It is likely that this is because CAII-dependent cytosolic H+ production is required to enable parallel H+ and NH3 across the apical plasma membrane. CAII also facilitates the basolateral efflux of HCO3− by activating the Cl−/HCO3 exchanger AE1 [104]. Ae1 R607H knockin mouse, which carries the most common dominant dRTA variant of human AE1, R589H, shows a reduced number of type A IC and a decreased expression of B1 subunit of the H+-ATPase. One explanation could be that a reduced basolateral anion-exchange activity in type A ICs compromises the traffic and activity of H+-ATPase and hence the luminal acid secretion [85]. Another Cl−/HCO3− exchanger, SLC26A7, also expressed with AE1 at the plasma membrane of type A IC in OMCD, has been involved in the function of type A IC in this segment. Slc26a7 knockout mice exhibit metabolic acidosis and excrete a more alkaline urine than their wild-type counterparts at baseline [127]. In transfected MDCK, the SLC26A7 abundance increases with medium osmolarity and decreases with extracellular acidic pH [108]. Both AE1 and SLC26A7 could be involved in HCO3− reabsorption by type A IC and in the regulation of H+ secreting cells in response to modulations in extracellular pH and osmolarity [108]. Their cooperation has not yet been directly demonstrated.
Luminal secretion
Several in vitro and ex vivo studies have demonstrated that Rhcg is an NH3 channel (for review [113]). We were able to show that transepithelial transport of ammonia was drastically reduced in the ex vivo microperfused CCD or OMCD from Rhcg knockout mice due to decreased NH3 uptake [7, 13]. A large body of evidence indicates that Rhcg plays a crucial role in ammonia transport with a primary involvement in luminal NH3 secretion by collecting duct cells [13]. The first demonstrations were carried out in various mouse models of global or kidney-specific deletion of Rhcg gene. In all studies, Rhcg knockout mice developed incomplete dRTA with a marked reduction in ammonium excretion in the final urine [7, 13, 74, 75]. Furthermore, Rhcg has been shown to have a crucial role in renal ammonia excretion under different physiological or pathophysiological conditions such as high-protein diet, hypokalemia, ischemia–reperfusion injury, cyclosporine-induced nephropathy, reduced renal mass, or in Cy/ + rats, a model of chronic kidney disease [11, 21, 49, 50, 64, 76]. Membrane expression of Rhcg depends on the amount trafficked to and retrieved from the membrane. Its localization at the plasma membrane is increased by chronic metabolic acidosis and aldosterone [31, 99].
Most ammonia excreted in the final urine comes from secretion from the collecting duct, which requires parallel secretion of NH3 and H+ to allow the final urine acidification. The multimeric apical plasma membrane H+-ATPase protein of the type A IC has been postulated to mediate the majority of H+ secretion across the apical plasma membrane of the type-A IC. Mice with a disrupted B1 H+-ATPase subunit (ATP6V1B1) develop incomplete dRTA [12, 14, 35, 63]. Comparison of the phenotypes of Rhcg and Atp6v1b1 knockout mice has shown that Rhcg knockout mice excrete alkaline urine and little ammonia, whereas Atp6v1b1 knockout mice have only a mild reduction of their ammonia excretion during a chronic acid load [12, 13]. Cellular studies have established that Rhcg and H+-ATPase co-immunoprecipitate in the rat kidney tissue, indicating a close interaction between the two proteins [14]. In CCD from Rhcg and Atp6v1b1 knockout mice, while NH3 and H+ transports are reduced in CCD from Rhcg knockout mice, only H+ transport is impaired in CCD from Atp6v1b1 knockout mice, indicating that Rhcg can modulate H+-ATPase activity in CCD cells [14]. This non-reciprocal modulation of the activity of H+-ATPase by Rhcg makes sense from a physiological point of view, since NH3 is the main buffer of protons in urine.
Electroneutral H+,K+-ATPase activity has also been reported from the CNT to the IMCD in rats and mice [38]. Under control diet, total H+,K+-ATPase activity increases during acidosis and potassium deficiency [87, 101]. The role of H+,K+-ATPase may therefore be more important in potassium deficiency as suggested by a case report of distal renal tubular acidosis with severe hypokalemia in a 21-month-old boy [103]. Two isoforms of the protein are present in the distal nephron: the HK1 or gastric form and the HK2 also known as the “nongastric” or “colonic” H–K-ATPase. Under control diet, both isoforms are contributing to H+ secretion in the CCD of mice [79]. Yet, the exact role of H+,K+-ATPases in ammonia handling is not understood; it has been shown that H+,K+-ATPases can directly transport NH4+ but also that their activities can be regulated by ammonia in the renal tissue [37, 107]. However, phenotypic studies of HK1 and HK2 knockout mice subjected to experimental acid loading are lacking to directly establish the role of the H+,K+-ATPase in the final excretion of ammonia by the kidney.
Other diffusive transporters for NH3 movement across the apical and basolateral membranes of the collecting duct may also contribute to ammonia secretion as suggested in cultured mIMCD-3 ([51, 52]). However, this transport is now considered marginal as the deletion of Rhcg in mice abolishes almost 80% of total and apical or basolateral membrane NH3 permeability through the CCD or OMCD [7, 13], establishing Rhcg as the main ammonia channel in the collecting duct (Fig. 3).
Sex differences in ammonia handling by the kidney
The sex difference in ammonia handling by the kidney is an ongoing research topic, which has been studied mainly in mice, so far [22, 81, 124]. A striking sex difference in mouse kidney lies in the structure of the kidney itself, seen both under baseline condition and during acid loading. Male mice have bigger proximal tubules than female mice, and, conversely, the collecting ducts represent a larger volume of the whole kidney in females [53, 54]. On a normal diet, female mice excrete twice as much urinary ammonium as males in urine [54] while having similar food intake and plasma bicarbonate concentration. In addition, female mice show a greater expression of PEPCK, glutamine synthetase, NKCC2, Rhbg, and Rhcg, but not of NBCe1, than male mice [54]. In males, orchidectomy increased urinary ammonium excretion and the expression of PEPCK and NKCC2, both effects being reversed under treatment by testosterone [55]. The authors conclude that the sex difference in proteins involved in ammonia metabolism and transport results in greater ammonia excretion in female than in male mice. We would like to consider an alternative explanation. On steady state in normal mice, a higher ammonia excretion in urine indicates a higher acid production within the body that seems to be androgen dependent. Then, the kidney has to adapt to the higher acid production by producing more ammonia in the proximal tubule and secreting more ammonia along the collecting duct: the different expression of proteins involved in ammonia production and transport could reflect an adaptation to a higher acid production, not being the primary cause of higher ammonia excretion in females.
When subjected to a 7-day HCl loading, both female and male mice were able to carry out a 10- to 15-fold increase in urinary ammonia excretion, indicating that the androgen-dependent difference in ammonia excretion seen on baseline can be eliminated by the need to increase tubular ammonia production and secretion [53]. After 7 days on acid load, no difference in PEPCK, SNAT3, NBCe1, NHE3, Rhbg, and a4 subunit of H+-ATPase protein expression could be seen between female and male mice [53, 54]. NKCC2 and Rhcg protein expression remained higher in females than in males [53, 54]. The structural differences between females and males seen on baseline regarding relative cortical proximal tubule and collecting duct volumes were maintained.
The sex difference in kidney structure, specific protein expression, and, likely, metabolic acid production does not prevent both female and male mice to maintain a normal acid–base status on baseline; both male and female mice are able to increase ammonium excretion adequately and similarly on large acid load. Obviously, the mechanisms involved in the sex difference of metabolic acid production, as well as those linking androgens to acid–base homeostasis deserve further investigation.
Open questions and new directions
Thanks to the development of new molecular and cellular tools and the study of knockout animal models, research carried out in recent years has considerably improved our understanding of ammonia handling in the kidney, its role for the maintenance of acid–base homeostasis, as well as compensatory mechanisms allowing to maintain acid excretion in the context of kidney disease. Nevertheless, gaps in our understanding persist, and new questions have been raised by recent discoveries.
Firstly, a molecular cause is not retrieved in all patients with inherited forms of renal tubular acidosis, either proximal or distal [114]. Full genome sequencing, combined with functional studies of the candidate genes listed in this review, mutated in humans or causing renal tubular acidosis in knockout animal models, such as Kir4.2, NHE4, NBCn1, and Rhcg, can be expected to resolve many of these cases and better explain the underlying mechanisms in the near future.
Secondly, the role of determinants of cell polarity, such as FOXI1, and of signaling or scaffolding, such as WDR72, both recently discovered thanks to gene sequencing in patients, is not yet fully understood. Similarly, the list of protagonists of ammonia metabolism and transport inside and outside the mitochondria of the proximal tubule is still incomplete; the precise role of sulfatides, the lack of which is associated with acidosis, is not understood. Further research is needed to decipher the role of these newly discovered protagonists in the process of acid excretion by the kidney.
Thirdly, the description of sex differences in renal physiology and pathophysiology is still in its infancy, and the understanding of these differences is far from complete.
Finally, although the role and impact of acidosis on the development and progression of CKD has long been known, the mechanisms involved in the adverse effects of acidosis during CKD progression remain incompletely deciphered. The injured kidney responds to the decline in urinary ammonium excretion by increasing t-ammonia production in the remaining functional nephrons. This phenomenon was observed, for example, in the remnant kidney of a CKD stage III rat model of reduced renal mass where an increase in the rate of ammonia production was observed in vitro from the rats fed a high-protein diet [97, 124, 125]. However, this compensatory response can lead to high local intrarenal ammonia concentrations which, in the long term, can trigger deleterious mechanisms in the remaining healthy renal tissue. Stimulation of the complement pathway, recruitment of inflammatory cells, and oxidative stress can be enhanced by high ammonium concentration in renal tissue and promote a cascade of events that may eventually lead to tubulointerstitial fibrosis [29]. A direct link between intrarenal ammonium accumulation and kidney fibrosis has yet to be established in humans. Acidosis also promotes systemic and renal production of endocrine factors such as aldosterone, angiotensin II, or endothelin 1 (ET1). ET1, whose two receptors, ETA and ETB are functional in the renal tissue, contributes to maintain normal bicarbonatemia and blood pH via its ETB receptor by activating transporters leading to bicarbonate reabsorption in the proximal tubule and protons excretion in the collecting duct. However, ET1 also promotes renal injury, proteinuria, inflammation, and kidney tissue fibrosis via its ETA receptor. The mechanisms involved in balancing these two antagonistic actions remain to be identified.
Conclusion
This review summarizes the state of knowledge on NH3/NH4+ production and transport by the kidney. Fundamental discoveries have altered our understanding of the molecular mechanisms of renal ammonia transport in recent decades. Future research in this field is needed to understand the fate of ammonia metabolism in pathophysiological states and to provide insight into the mechanisms of kidney disease.
Data availability
No datasets were generated or analyzed during the current study.
References
Arnett TR (2008) Extracellular pH regulates bone cell function. J Nutr 138:415S-418S. https://doi.org/10.1093/jn/138.2.415S
Bagnis C, Marshansky V, Breton S, Brown D (2001) Remodeling the cellular profile of collecting ducts by chronic carbonic anhydrase inhibition. Am J Physiol Renal Physiol 280:F437-448. https://doi.org/10.1152/ajprenal.2001.280.3.F437
Bailey JL (2005) Metabolic acidosis: an unrecognized cause of morbidity in the patient with chronic kidney disease. Kidney Int Suppl:S15–23. https://doi.org/10.1111/j.1523-1755.2005.00450.x
Bignon Y, Pinelli L, Frachon N, Lahuna O, Figueres L, Houillier P, Lourdel S, Teulon J, Paulais M (2020) Defective bicarbonate reabsorption in Kir4.2 potassium channel deficient mice impairs acid-base balance and ammonia excretion. Kidney Int 97:304–315. https://doi.org/10.1016/j.kint.2019.09.028
Bishop JM, Lee HW, Handlogten ME, Han KH, Verlander JW, Weiner ID (2013) Intercalated cell-specific Rh B glycoprotein deletion diminishes renal ammonia excretion response to hypokalemia. Am J Physiol Renal Physiol 304:F422-431. https://doi.org/10.1152/ajprenal.00301.2012
Bishop JM, Verlander JW, Lee HW, Nelson RD, Weiner AJ, Handlogten ME, Weiner ID (2010) Role of the Rhesus glycoprotein, Rh B glycoprotein, in renal ammonia excretion. Am J Physiol Renal Physiol 299:F1065-1077. https://doi.org/10.1152/ajprenal.00277.2010
Biver S, Belge H, Bourgeois S, Van Vooren P, Nowik M, Scohy S, Houillier P, Szpirer J, Szpirer C, Wagner CA, Devuyst O, Marini AM (2008) A role for Rhesus factor Rhcg in renal ammonium excretion and male fertility. Nature 456:339–343. https://doi.org/10.1038/nature07518
Boedtkjer E, Praetorius J, Fuchtbauer EM, Aalkjaer C (2008) Antibody-independent localization of the electroneutral Na+-HCO3- cotransporter NBCn1 (slc4a7) in mice. Am J Physiol Cell Physiol 294:C591-603. https://doi.org/10.1152/ajpcell.00281.2007
Bookstein C, Musch MW, DePaoli A, Xie Y, Rabenau K, Villereal M, Rao MC, Chang EB (1996) Characterization of the rat Na+/H+ exchanger isoform NHE4 and localization in rat hippocampus. Am J Physiol 271:C1629-1638. https://doi.org/10.1152/ajpcell.1996.271.5.C1629
Boron VF, Hediger MA, Boulpaep EL, Romero MF (1997) The renal electrogenic Na+:HCO-3 cotransporter. J Exp Biol 200:263–268. https://doi.org/10.1242/jeb.200.2.263
Bounoure L, Ruffoni D, Muller R, Kuhn GA, Bourgeois S, Devuyst O, Wagner CA (2014) The role of the renal ammonia transporter Rhcg in metabolic responses to dietary protein. J Am Soc Nephrol 25:2040–2052. https://doi.org/10.1681/ASN.2013050466
Bourgeois S, Bettoni C, Baron S, Wagner CA (2018) Haploinsufficiency of the mouse Atp6v1b1 gene leads to a mild acid-base disturbance with implications for kidney stone disease. Cell Physiol Biochem 47:1095–1107. https://doi.org/10.1159/000490186
Bourgeois S, Bounoure L, Christensen EI, Ramakrishnan SK, Houillier P, Devuyst O, Wagner CA (2013) Haploinsufficiency of the ammonia transporter Rhcg predisposes to chronic acidosis: Rhcg is critical for apical and basolateral ammonia transport in the mouse collecting duct. J Biol Chem 288:5518–5529. https://doi.org/10.1074/jbc.M112.441782
Bourgeois S, Bounoure L, Mouro-Chanteloup I, Colin Y, Brown D, Wagner CA (2018) The ammonia transporter RhCG modulates urinary acidification by interacting with the vacuolar proton-ATPases in renal intercalated cells. Kidney Int 93:390–402. https://doi.org/10.1016/j.kint.2017.07.027
Bourgeois S, Masse S, Paillard M, Houillier P (2002) Basolateral membrane Cl(-)-, Na(+)-, and K(+)-coupled base transport mechanisms in rat MTALH. Am J Physiol Renal Physiol 282:F655-668. https://doi.org/10.1152/ajprenal.00220.2000
Bourgeois S, Meer LV, Wootla B, Bloch-Faure M, Chambrey R, Shull GE, Gawenis LR, Houillier P (2010) NHE4 is critical for the renal handling of ammonia in rodents. J Clin Invest 120:1895–1904. https://doi.org/10.1172/JCI36581
Brown AC, Hallouane D, Mawby WJ, Karet FE, Saleem MA, Howie AJ, Toye AM (2009) RhCG is the major putative ammonia transporter expressed in the human kidney, and RhBG is not expressed at detectable levels. Am J Physiol Renal Physiol 296:F1279-1290. https://doi.org/10.1152/ajprenal.00013.2009
Buerkert J, Martin D (1983) Deep nephron and collecting duct function after unilateral reduction in renal mass. Miner Electrol Metab 9:137–146
Buerkert J, Martin D, Trigg D (1982) Ammonium handling by superficial and juxtamedullary nephrons in the rat. Evidence for an ammonia shunt between the loop of Henle and the collecting duct. J Clin Invest 70:1–12. https://doi.org/10.1172/jci110581
Buerkert J, Martin D, Trigg D (1983) Segmental analysis of the renal tubule in buffer production and net acid formation. Am J Physiol 244:F442-454. https://doi.org/10.1152/ajprenal.1983.244.4.F442
Burki R, Mohebbi N, Bettoni C, Wang X, Serra AL, Wagner CA (2015) Impaired expression of key molecules of ammoniagenesis underlies renal acidosis in a rat model of chronic kidney disease. Nephrol Dial Transplant 30:770–781. https://doi.org/10.1093/ndt/gfu384
Canales BK, Smith JA, Weiner ID, Ware EB, Zhao W, Kardia SLR, Curhan GC, Turner ST, Perinpam M, Lieske JC (2017) Polymorphisms in renal ammonia metabolism genes correlate with 24-hour urine pH. Kidney Int Rep 2:1111–1121. https://doi.org/10.1016/j.ekir.2017.06.009
Caner T, Abdulnour-Nakhoul S, Brown K, Islam MT, Hamm LL, Nakhoul NL (2015) Mechanisms of ammonia and ammonium transport by rhesus-associated glycoproteins. Am J Physiol Cell Physiol 309:C747-758. https://doi.org/10.1152/ajpcell.00085.2015
Chambrey R, Achard JM, St John PL, Abrahamson DR, Warnock DG (1997) Evidence for an amiloride-insensitive Na+/H+ exchanger in rat renal cortical tubules. Am J Physiol 273:C1064-1074. https://doi.org/10.1152/ajpcell.1997.273.3.C1064
Chambrey R, Goossens D, Bourgeois S, Picard N, Bloch-Faure M, Leviel F, Geoffroy V, Cambillau M, Colin Y, Paillard M, Houillier P, Cartron JP, Eladari D (2005) Genetic ablation of Rhbg in the mouse does not impair renal ammonium excretion. Am J Physiol Renal Physiol 289:F1281-1290. https://doi.org/10.1152/ajprenal.00172.2005
Chambrey R, St John PL, Eladari D, Quentin F, Warnock DG, Abrahamson DR, Podevin RA, Paillard M (2001) Localization and functional characterization of Na+/H+ exchanger isoform NHE4 in rat thick ascending limbs. Am J Physiol Renal Physiol 281:F707-717. https://doi.org/10.1152/ajprenal.2001.281.4.F707
Chan K, Busque SM, Sailer M, Stoeger C, Broer S, Daniel H, Rubio-Aliaga I, Wagner CA (2016) Loss of function mutation of the Slc38a3 glutamine transporter reveals its critical role for amino acid metabolism in the liver, brain, and kidney. Pflugers Arch 468:213–227. https://doi.org/10.1007/s00424-015-1742-0
Choi I, Aalkjaer C, Boulpaep EL, Boron WF (2000) An electroneutral sodium/bicarbonate cotransporter NBCn1 and associated sodium channel. Nature 405:571–575. https://doi.org/10.1038/35014615
Clark EC, Nath KA, Hostetter MK, Hostetter TH (1990) Role of ammonia in tubulointerstitial injury. Miner Electrolyte Metab 16:315–321
Deshmukh GD, Radin NS, Gattone VH 2nd, Shayman JA (1994) Abnormalities of glycosphingolipid, sulfatide, and ceramide in the polycystic (cpk/cpk) mouse. J Lipid Res 35:1611–1618
Eguchi K, Izumi Y, Yasuoka Y, Nakagawa T, Ono M, Maruyama K, Matsuo N, Hiramatsu A, Inoue H, Nakayama Y, Nonoguchi H, Lee HW, Weiner ID, Kakizoe Y, Kuwabara T, Mukoyama M (2021) Regulation of Rhcg, an ammonia transporter, by aldosterone in the kidney. J Endocrinol 249:95–112. https://doi.org/10.1530/JOE-20-0267
Eladari D, Cheval L, Quentin F, Bertrand O, Mouro I, Cherif-Zahar B, Cartron JP, Paillard M, Doucet A, Chambrey R (2002) Expression of RhCG, a new putative NH(3)/NH(4)(+) transporter, along the rat nephron. J Am Soc Nephrol 13:1999–2008. https://doi.org/10.1097/01.asn.0000025280.02386.9d
Elkjaer ML, Nejsum LN, Gresz V, Kwon TH, Jensen UB, Frokiaer J, Nielsen S (2001) Immunolocalization of aquaporin-8 in rat kidney, gastrointestinal tract, testis, and airways. Am J Physiol Renal Physiol 281:F1047-1057. https://doi.org/10.1152/ajprenal.0158.2001
Enerback S, Nilsson D, Edwards N, Heglind M, Alkanderi S, Ashton E, Deeb A, Kokash FEB, Bakhsh ARA, Van’t Hoff W, Walsh SB, D’Arco F, Daryadel A, Bourgeois S, Wagner CA, Kleta R, Bockenhauer D, Sayer JA (2018) Acidosis and deafness in patients with recessive mutations in FOXI1. J Am Soc Nephrol 29:1041–1048. https://doi.org/10.1681/ASN.2017080840
Finberg KE, Wagner CA, Bailey MA, Paunescu TG, Breton S, Brown D, Giebisch G, Geibel JP, Lifton RP (2005) The B1-subunit of the H(+) ATPase is required for maximal urinary acidification. Proc Natl Acad Sci USA 102:13616–13621. https://doi.org/10.1073/pnas.0506769102
Flessner MF, Mejia R, Knepper MA (1993) Ammonium and bicarbonate transport in isolated perfused rodent long-loop thin descending limbs. Am J Physiol 264:F388-396. https://doi.org/10.1152/ajprenal.1993.264.3.F388
Frank AE, Wingo CS, Weiner ID (2000) Effects of ammonia on bicarbonate transport in the cortical collecting duct. Am J Physiol-Renal 278:F219–F226. https://doi.org/10.1152/ajprenal.2000.278.2.F219
Garg LC (1991) Respective roles of H-ATPase and H-K-ATPase in ion transport in the kidney. J Am Soc Nephrol 2:949–960. https://doi.org/10.1681/ASN.V25949
Garvin JL, Burg MB, Knepper MA (1988) Active NH4+ absorption by the thick ascending limb. Am J Physiol 255:F57-65. https://doi.org/10.1152/ajprenal.1988.255.1.F57
Good DW (1987) Effects of potassium on ammonia transport by medullary thick ascending limb of the rat. J Clin Invest 80:1358–1365. https://doi.org/10.1172/JCI113213
Good DW (1988) Active absorption of NH4+ by rat medullary thick ascending limb: inhibition by potassium. Am J Physiol 255:F78-87. https://doi.org/10.1152/ajprenal.1988.255.1.F78
Good DW (1990) Inhibition of bicarbonate absorption by peptide hormones and cyclic adenosine monophosphate in rat medullary thick ascending limb. J Clin Invest 85:1006–1013. https://doi.org/10.1172/JCI114530
Good DW (1994) Ammonium transport by the thick ascending limb of Henle’s loop. Annu Rev Physiol 56:623–647. https://doi.org/10.1146/annurev.ph.56.030194.003203
Good DW (1995) Hyperosmolality inhibits bicarbonate absorption in rat medullary thick ascending limb via a protein-tyrosine kinase-dependent pathway. J Biol Chem 270:9883–9889. https://doi.org/10.1074/jbc.270.17.9883
Good DW, Burg MB (1984) Ammonia production by individual segments of the rat nephron. J Clin Invest 73:602–610. https://doi.org/10.1172/JCI111250
Good DW, Caflisch CR, DuBose TD Jr (1987) Transepithelial ammonia concentration gradients in inner medulla of the rat. Am J Physiol 252:F491-500. https://doi.org/10.1152/ajprenal.1987.252.3.F491
Good DW, DuBose TD Jr (1987) Ammonia transport by early and late proximal convoluted tubule of the rat. J Clin Invest 79:684–691. https://doi.org/10.1172/JCI112871
Good DW, George T, Wang DH (1999) Angiotensin II inhibits HCO-3 absorption via a cytochrome P-450-dependent pathway in MTAL. Am J Physiol 276:F726-736
Han KH, Kim HY, Croker BP, Reungjui S, Lee SY, Kim J, Handlogten ME, Adin CA, Weiner ID (2007) Effects of ischemia-reperfusion injury on renal ammonia metabolism and the collecting duct. Am J Physiol Renal Physiol 293:F1342-1354. https://doi.org/10.1152/ajprenal.00437.2006
Han KH, Lee HW, Handlogten ME, Bishop JM, Levi M, Kim J, Verlander JW, Weiner ID (2011) Effect of hypokalemia on renal expression of the ammonia transporter family members, Rh B Glycoprotein and Rh C Glycoprotein, in the rat kidney. Am J Physiol Renal Physiol 301:F823-832. https://doi.org/10.1152/ajprenal.00266.2011
Handlogten ME, Hong SP, Westhoff CM, Weiner ID (2004) Basolateral ammonium transport by the mouse inner medullary collecting duct cell (mIMCD-3). Am J Physiol Renal Physiol 287:F628-638. https://doi.org/10.1152/ajprenal.00363.2003
Handlogten ME, Hong SP, Westhoff CM, Weiner ID (2005) Apical ammonia transport by the mouse inner medullary collecting duct cell (mIMCD-3). Am J Physiol Renal Physiol 289:F347-358. https://doi.org/10.1152/ajprenal.00253.2004
Harris AN, Lee HW, Fang LJ, Verlander JW, Weiner ID (2019) Differences in acidosis-stimulated renal ammonia metabolism in the male and female kidney. Am J Physiol-Renal 317:F890–F905. https://doi.org/10.1152/ajprenal.00244.2019
Harris AN, Lee HW, Osis G, Fang L, Webster KL, Verlander JW, Weiner ID (2018) Differences in renal ammonia metabolism in male and female kidney. Am J Physiol Renal Physiol 315:F211–F222. https://doi.org/10.1152/ajprenal.00084.2018
Harris AN, Lee HW, Verlander JW, Weiner ID (2020) Testosterone modulates renal ammonia metabolism. Am J Physiol-Renal 318:F922–F935. https://doi.org/10.1152/ajprenal.00560.2019
Harris AN, Skankar M, Melanmed M, Batlle D (2023) An update on kidney ammonium transport along the nephron. Adv Kidney Dis Health 30:189–196. https://doi.org/10.1053/j.akdh.2022.12.005
Haussinger D, Lamers WH, Moorman AF (1992) Hepatocyte heterogeneity in the metabolism of amino acids and ammonia. Enzyme 46:72–93. https://doi.org/10.1159/000468779
Holm LM, Jahn TP, Moller AL, Schjoerring JK, Ferri D, Klaerke DA, Zeuthen T (2005) NH3 and NH4+ permeability in aquaporin-expressing Xenopus oocytes. Pflugers Arch 450:415–428. https://doi.org/10.1007/s00424-005-1399-1
Houillier P, Bourgeois S (2012) More actors in ammonia absorption by the thick ascending limb. Am J Physiol Renal Physiol 302:F293-297. https://doi.org/10.1152/ajprenal.00307.2011
Huynh KW, Jiang J, Abuladze N, Tsirulnikov K, Kao L, Shao X, Newman D, Azimov R, Pushkin A, Zhou ZH, Kurtz I (2018) CryoEM structure of the human SLC4A4 sodium-coupled acid-base transporter NBCe1. Nat Commun 9:900. https://doi.org/10.1038/s41467-018-03271-3
Jehle S, Zanetti A, Muser J, Hulter HN, Krapf R (2006) Partial neutralization of the acidogenic Western diet with potassium citrate increases bone mass in postmenopausal women with osteopenia. J Am Soc Nephrol 17:3213–3222. https://doi.org/10.1681/ASN.2006030233
Karet FE (2002) Inherited distal renal tubular acidosis. J Am Soc Nephrol 13:2178–2184. https://doi.org/10.1097/01.asn.0000023433.08833.88
Karet FE, Finberg KE, Nelson RD, Nayir A, Mocan H, Sanjad SA, Rodriguez-Soriano J, Santos F, Cremers CW, Di Pietro A, Hoffbrand BI, Winiarski J, Bakkaloglu A, Ozen S, Dusunsel R, Goodyer P, Hulton SA, Wu DK, Skvorak AB, Morton CC, Cunningham MJ, Jha V, Lifton RP (1999) Mutations in the gene encoding B1 subunit of H+-ATPase cause renal tubular acidosis with sensorineural deafness. Nat Genet 21:84–90. https://doi.org/10.1038/5022
Kim HY, Baylis C, Verlander JW, Han KH, Reungjui S, Handlogten ME, Weiner ID (2007) Effect of reduced renal mass on renal ammonia transporter family, Rh C glycoprotein and Rh B glycoprotein, expression. Am J Physiol Renal Physiol 293:F1238-1247. https://doi.org/10.1152/ajprenal.00151.2007
Kim J, Kim YH, Cha JH, Tisher CC, Madsen KM (1999) Intercalated cell subtypes in connecting tubule and cortical collecting duct of rat and mouse. J Am Soc Nephrol 10:1–12. https://doi.org/10.1681/ASN.V1011
Kinne R, Kinne-Saffran E, Schutz H, Scholermann B (1986) Ammonium transport in medullary thick ascending limb of rabbit kidney: involvement of the Na+, K+, Cl(-)-cotransporter. J Membr Biol 94:279–284. https://doi.org/10.1007/BF01869723
Knepper MA, Packer R, Good DW (1989) Ammonium transport in the kidney. Physiol Rev 69:179–249. https://doi.org/10.1152/physrev.1989.69.1.179
Koumangoye R, Bastarache L, Delpire E (2021) NKCC1: newly found as a human disease-causing ion transporter. Function (Oxf) 2:zqaa028. https://doi.org/10.1093/function/zqaa028
I Kurtz 2018 NBCe1 electrogenic Na+-coupled HCO3−(CO32−) transporter Encyclopedia of Signaling Molecules https://doi.org/10.1007/978-3-319-67199-4_101572
Kurtz I, Balaban RS (1986) Ammonium as a substrate for Na+-K+-ATPase in rabbit proximal tubules. Am J Physiol 250:F497-502. https://doi.org/10.1152/ajprenal.1986.250.3.F497
Kwon TH, Fulton C, Wang W, Kurtz I, Frokiaer J, Aalkjaer C, Nielsen S (2002) Chronic metabolic acidosis upregulates rat kidney Na-HCO cotransporters NBCn1 and NBC3 but not NBC1. Am J Physiol Renal Physiol 282:F341-351. https://doi.org/10.1152/ajprenal.00104.2001
Lee SK, Occhipinti R, Moss FJ, Parker MD, Grichtchenko II, Boron WF (2023) Distinguishing among HCO3-, CO3–, and H+ as substrates of proteins that appear to be “bicarbonate” transporters. J Am Soc Nephrol 34:40–54. https://doi.org/10.1681/Asn.2022030289
Lee HW, Verlander JW, Bishop JM, Igarashi P, Handlogten ME, Weiner ID (2009) Collecting duct-specific Rh C glycoprotein deletion alters basal and acidosis-stimulated renal ammonia excretion. Am J Physiol Renal Physiol 296:F1364-1375. https://doi.org/10.1152/ajprenal.90667.2008
Lee HW, Verlander JW, Bishop JM, Nelson RD, Handlogten ME, Weiner ID (2010) Effect of intercalated cell-specific Rh C glycoprotein deletion on basal and metabolic acidosis-stimulated renal ammonia excretion. Am J Physiol Renal Physiol 299:F369-379. https://doi.org/10.1152/ajprenal.00120.2010
Lee HW, Verlander JW, Handlogten ME, Han KH, Weiner ID (2014) Effect of collecting duct-specific deletion of both Rh B glycoprotein (Rhbg) and Rh C glycoprotein (Rhcg) on renal response to metabolic acidosis. Am J Physiol Renal Physiol 306:F389-400. https://doi.org/10.1152/ajprenal.00176.2013
Lim SW, Ahn KO, Kim WY, Han DH, Li C, Ghee JY, Han KH, Kim HY, Handlogten ME, Kim J, Yang CW, Weiner ID (2008) Expression of ammonia transporters, Rhbg and Rhcg, in chronic cyclosporine nephropathy in rats. Nephron Exp Nephrol 110:e49-58. https://doi.org/10.1159/000153245
Liu K, Nagase H, Huang CG, Calamita G, Agre P (2006) Purification and functional characterization of aquaporin-8. Biol Cell 98:153–161. https://doi.org/10.1042/BC20050026
Lullmann-Rauch R, Matzner U, Franken S, Hartmann D, Gieselmann V (2001) Lysosomal sulfoglycolipid storage in the kidneys of mice deficient for arylsulfatase A (ASA) and of double-knockout mice deficient for ASA and galactosylceramide synthase. Histochem Cell Biol 116:161–169. https://doi.org/10.1007/s004180100286
Lynch IJ, Rudin A, Xia SL, Stow LR, Shull GE, Weiner ID, Cain BD, Wingo CS (2008) Impaired acid secretion in cortical collecting duct intercalated cells from H-K-ATPase-deficient mice: role of HKalpha isoforms. Am J Physiol Renal Physiol 294:F621-627. https://doi.org/10.1152/ajprenal.00412.2007
Mallela SK, Merscher S, Fornoni A (2022) Implications of sphingolipid metabolites in kidney diseases. Int J Mol Sci 23. https://doi.org/10.3390/ijms23084244
McDonough AA, Harris AN, Xiong LY, Layton AT (2023) Sex differences in renal transporters: assessment and functional consequences. Nat Rev Nephrol. https://doi.org/10.1038/s41581-023-00757-2
Michalek K (2016) Aquaglyceroporins in the kidney: present state of knowledge and prospects. J Physiol Pharmacol 67:185–193
Molinas SM, Trumper L, Marinelli RA (2012) Mitochondrial aquaporin-8 in renal proximal tubule cells: evidence for a role in the response to metabolic acidosis. Am J Physiol Renal Physiol 303:F458-466. https://doi.org/10.1152/ajprenal.00226.2012
Moret C, Dave MH, Schulz N, Jiang JX, Verrey F, Wagner CA (2007) Regulation of renal amino acid transporters during metabolic acidosis. Am J Physiol Renal Physiol 292:F555-566. https://doi.org/10.1152/ajprenal.00113.2006
Mumtaz R, Trepiccione F, Hennings JC, Huebner AK, Serbin B, Picard N, Ullah A, Paunescu TG, Capen DE, Lashhab RM, Mouro-Chanteloup I, Alper SL, Wagner CA, Cordat E, Brown D, Eladari D, Hubner CA (2017) Intercalated cell depletion and vacuolar H+-ATPase mistargeting in an Ae1 R607H knockin model. J Am Soc Nephrol 28:1507–1520. https://doi.org/10.1681/ASN.2016020169
Mutig K (2017) Trafficking and regulation of the NKCC2 cotransporter in the thick ascending limb. Curr Opin Nephrol Hypertens 26:392–397. https://doi.org/10.1097/MNH.0000000000000351
Nakamura S, Amlal H, Galla JH, Soleimani M (1999) NH4+ secretion in inner medullary collecting duct in potassium deprivation: role of colonic H+-K+-ATPase. Kidney Int 56:2160–2167. https://doi.org/10.1046/j.1523-1755.1999.00780.x
Odgaard E, Jakobsen JK, Frische S, Praetorius J, Nielsen S, Aalkjaer C, Leipziger J (2004) Basolateral Na+-dependent HCO3- transporter NBCn1-mediated HCO3- influx in rat medullary thick ascending limb. J Physiol 555:205–218. https://doi.org/10.1113/jphysiol.2003.046474
Olsen JSM, Svendsen S, Berg P, Dam VS, Sorensen MV, Matchkov VV, Leipziger J, Boedtkjer E (2021) NBCn1 increases NH(4) (+) reabsorption across thick ascending limbs, the capacity for urinary NH(4) (+) excretion, and early recovery from metabolic acidosis. J Am Soc Nephrol 32:852–865. https://doi.org/10.1681/ASN.2019060613
Orlowski J (1993) Heterologous expression and functional properties of amiloride high affinity (NHE-1) and low affinity (NHE-3) isoforms of the rat Na/H exchanger. J Biol Chem 268:16369–16377
Packer RK, Desai SS, Hornbuckle K, Knepper MA (1991) Role of countercurrent multiplication in renal ammonium handling: regulation of medullary ammonium accumulation. J Am Soc Nephrol 2:77–83. https://doi.org/10.1681/ASN.V2177
Quentin F, Eladari D, Cheval L, Lopez C, Goossens D, Colin Y, Cartron JP, Paillard M, Chambrey R (2003) RhBG and RhCG, the putative ammonia transporters, are expressed in the same cells in the distal nephron. J Am Soc Nephrol 14:545–554. https://doi.org/10.1097/01.asn.0000050413.43662.55
Robinson RR, Owen EE (1965) Intrarenal distribution of ammonia during diuresis and antidiuresis. Am J Physiol 208:1129–1134. https://doi.org/10.1152/ajplegacy.1965.208.6.1129
Rungroj N, Nettuwakul C, Sawasdee N, Sangnual S, Deejai N, Misgar RA, Pasena A, Khositseth S, Kirdpon S, Sritippayawan S, Vasuvattakul S, Yenchitsomanus PT (2018) Distal renal tubular acidosis caused by tryptophan-aspartate repeat domain 72 (WDR72) mutations. Clin Genet 94:409–418. https://doi.org/10.1111/cge.13418
Sajo IM, Goldstein MB, Sonnenberg H, Stinebaugh BJ, Wilson DR, Halperin ML (1981) Sites of ammonia addition to tubular fluid in rats with chronic metabolic acidosis. Kidney Int 20:353–358. https://doi.org/10.1038/ki.1981.146
Saparov SM, Liu K, Agre P, Pohl P (2007) Fast and selective ammonia transport by aquaporin-8. J Biol Chem 282:5296–5301. https://doi.org/10.1074/jbc.M609343200
Schoolwerth AC, Sandler RS, Hoffman PM, Klahr S (1975) Effects of nephron reduction and dietary protein content on renal ammoniagenesis in the rat. Kidney Int 7:397–404. https://doi.org/10.1038/ki.1975.57
Seshadri RM, Klein JD, Kozlowski S, Sands JM, Kim YH, Han KH, Handlogten ME, Verlander JW, Weiner ID (2006) Renal expression of the ammonia transporters, Rhbg and Rhcg, in response to chronic metabolic acidosis. Am J Physiol Renal Physiol 290:F397-408. https://doi.org/10.1152/ajprenal.00162.2005
Seshadri RM, Klein JD, Smith T, Sands JM, Handlogten ME, Verlander JW, Weiner ID (2006) Changes in subcellular distribution of the ammonia transporter, Rhcg, in response to chronic metabolic acidosis. Am J Physiol Renal Physiol 290:F1443-1452. https://doi.org/10.1152/ajprenal.00459.2005
Silbernagl S (1980) Tubular reabsorption of L-glutamine studied by free-flow micropuncture and microperfusion of rat kidney. Int J Biochem 12:9–16. https://doi.org/10.1016/0020-711x(80)90034-8
Silver RB, Mennitt P, Satlin LM (1996) Stimulation of apical H-K-ATPase in intercalated cells of cortical collecting duct with chronic metabolic acidosis. Am J Physiol Renal Fluid Electrolyt Physiol 270:F539–F547. https://doi.org/10.1152/ajprenal.1996.270.3.F539
Simon E, Martin D, Buerkert J (1985) Contribution of individual superficial nephron segments to ammonium handling in chronic metabolic acidosis in the rat. Evidence for ammonia disequilibrium in the renal cortex. J Clin Invest 76:855–864. https://doi.org/10.1172/JCI112043
Simpson AM, Schwartz GJ (2001) Distal renal tubular acidosis with severe hypokalaemia, probably caused by colonic H(+)-K(+)-ATPase deficiency. Arch Dis Child 84:504–507. https://doi.org/10.1136/adc.84.6.504
Sterling D, Reithmeier RAF, Casey JR (2001) A transport metabolon. Functional interaction of carbonic anhydrase II and chloride/bicarbonate exchangers. J Biol Chem 276:47886–47894. https://doi.org/10.1074/jbc.M105959200
Stettner P, Bourgeois S, Marsching C, Traykova-Brauch M, Porubsky S, Nordstrom V, Hopf C, Koesters R, Sandhoff R, Wiegandt H, Wagner CA, Grone HJ, Jennemann R (2013) Sulfatides are required for renal adaptation to chronic metabolic acidosis. Proc Natl Acad Sci USA 110:9998–10003. https://doi.org/10.1073/pnas.1217775110
Sullivan LP (1965) Ammonium excretion during stopped flow - a hypothetical ammonium countercurrent system. Am J Physiol 209:273–0. https://doi.org/10.1152/ajplegacy.1965.209.2.273
Swarts HGP, Koenderink JB, Willems PHGM, De Pont JJHHM (2005) The non-gastric H, K-ATPase is oligomycin-sensitive and can function as an H, NH-ATPase. J Biol Chem 280:33115–33122. https://doi.org/10.1074/jbc.M504535200
Ullah A, Rumley AC, Peleh V, Fernandes D, Almomani EY, Berrini M, Lashhab R, Touret N, Alexander RT, Herrmann JM, Cordat E (2020) SLC26A7 protein is a chloride/bicarbonate exchanger and its abundance is osmolarity- and pH-dependent in renal epithelial cells. Biochim Biophys Acta Biomembr 1862:183238. https://doi.org/10.1016/j.bbamem.2020.183238
Verissimo T, Dalga D, Arnoux G, Sakhi I, Faivre A, Auwerx H, Bourgeois S, Paolucci D, Gex Q, Rutkowski JM, Legouis D, Wagner CA, Hall AM, de Seigneux S (2023) PCK1 is a key regulator of metabolic and mitochondrial functions in renal tubular cells. Am J Physiol Renal Physiol 324:F532–F543. https://doi.org/10.1152/ajprenal.00038.2023
Verlander JW, Miller RT, Frank AE, Royaux IE, Kim YH, Weiner ID (2003) Localization of the ammonium transporter proteins RhBG and RhCG in mouse kidney. Am J Physiol Renal Physiol 284:F323-337. https://doi.org/10.1152/ajprenal.00050.2002
Vorum H, Kwon TH, Fulton C, Simonsen B, Choi I, Boron W, Maunsbach AB, Nielsen S, Aalkjaer C (2000) Immunolocalization of electroneutral Na-HCO(3)(-) cotransporter in rat kidney. Am J Physiol Renal Physiol 279:F901-909. https://doi.org/10.1152/ajprenal.2000.279.5.F901
Wagner CA, Bourgeois S (2014) Two Rhesus protein ammonia transporters team up to eliminate ammonium into urine. Am J Physiol Renal Physiol 306:F721-723. https://doi.org/10.1152/ajprenal.00681.2013
Wagner CA, Devuyst O, Belge H, Bourgeois S, Houillier P (2011) The rhesus protein RhCG: a new perspective in ammonium transport and distal urinary acidification. Kidney Int 79:154–161. https://doi.org/10.1038/ki.2010.386
Wagner CA, Unwin R, Lopez-Garcia SC, Kleta R, Bockenhauer D, Walsh S (2023) The pathophysiology of distal renal tubular acidosis. Nat Rev Nephrol 19:384–400. https://doi.org/10.1038/s41581-023-00699-9
Wall SM, Davis BS, Hassell KA, Mehta P, Park SJ (1999) In rat tIMCD, NH4+ uptake by Na-K-ATPase is critical to net acid secretion during chronic hypokalemia. Am J Physiol-Renal 277:F866–F874. https://doi.org/10.1152/ajprenal.1999.277.6.F866
Wall SM, Fischer MP (2002) Contribution of the Na(+)-K(+)-2Cl(-) cotransporter (NKCC1) to transepithelial transport of H(+), NH(4)(+), K(+), and Na(+) in rat outer medullary collecting duct. J Am Soc Nephrol 13(4):827–835. https://doi.org/10.1681/ASN.V134827
Wall SM, Fischer MP, Kim GH, Nguyen BM, Hassell KA (2002) In rat inner medullary collecting duct, NH4+ uptake by the Na, K-ATPase is increased during hypokalemia. Am J Physiol-Renal 282:F91–F102. https://doi.org/10.1152/ajprenal.0141.2001
Wall SM, Knepper MA, Hassell KA, Fischer MP, Shodeinde A, Shin W, Pham TD, Meyer JW, Lorenz JN, Beierwaltes WH, Dietz JR, Shull GE, Kim YH (2006) Hypotension in NKCC1 null mice: role of the kidneys. Am J Physiol Renal Physiol 290:F409-416. https://doi.org/10.1152/ajprenal.00309.2005
Wall SM, Koger LM (1994) Nh4+ transport mediated by Na+-K+-Atpase in rat inner medullary collecting duct. Am J Physiol-Renal 267:F660–F670. https://doi.org/10.1152/ajprenal.1994.267.4.F660
Watts BA 3rd, Good DW (1994) Effects of ammonium on intracellular pH in rat medullary thick ascending limb: mechanisms of apical membrane NH4+ transport. J Gen Physiol 103:917–936. https://doi.org/10.1085/jgp.103.5.917
Weiner ID, Hamm LL (2007) Molecular mechanisms of renal ammonia transport. Annu Rev Physiol 69:317–340. https://doi.org/10.1146/annurev.physiol.69.040705.142215
Weiner ID, Verlander JW (2014) Ammonia transport in the kidney by Rhesus glycoproteins. Am J Physiol Renal Physiol 306:F1107-1120. https://doi.org/10.1152/ajprenal.00013.2014
Weiner ID, Verlander JW (2017) Ammonia transporters and their role in acid-base balance. Physiol Rev 97:465–494. https://doi.org/10.1152/physrev.00011.2016
Weiner ID, Verlander JW (2019) Emerging features of ammonia metabolism and transport in acid-base balance. Semin Nephrol 39:394–405. https://doi.org/10.1016/j.semnephrol.2019.04.008
Wesson DE, Buysse JM, Bushinsky DA (2020) Mechanisms of metabolic acidosis-induced kidney injury in chronic kidney disease. J Am Soc Nephrol 31:469–482. https://doi.org/10.1681/ASN.2019070677
Wilson PC, Wu H, Kirita Y, Uchimura K, Ledru N, Rennke HG, Welling PA, Waikar SS, Humphreys BD (2019) The single-cell transcriptomic landscape of early human diabetic nephropathy. Proc Natl Acad Sci USA 116:19619–19625. https://doi.org/10.1073/pnas.1908706116
Xu J, Song P, Nakamura S, Miller M, Barone S, Alper SL, Riederer B, Bonhagen J, Arend LJ, Amlal H, Seidler U, Soleimani M (2009) Deletion of the chloride transporter slc26a7 causes distal renal tubular acidosis and impairs gastric acid secretion. J Biol Chem 284:29470–29479. https://doi.org/10.1074/jbc.M109.044396
Yang B, Zhao D, Solenov E, Verkman AS (2006) Evidence from knockout mice against physiologically significant aquaporin 8-facilitated ammonia transport. Am J Physiol Cell Physiol 291:C417-423. https://doi.org/10.1152/ajpcell.00057.2006
Acknowledgements
The authors sincerely thank Diane de Zelicourt for her diligent proofreading.
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Contributions
S.B. wrote the main manuscript text and prepared figures. S.B. and P.H. reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on Physiology of systemic and cellular pH regulation in Pflügers Archiv—European Journal of Physiology.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bourgeois, S., Houillier, P. State of knowledge on ammonia handling by the kidney. Pflugers Arch - Eur J Physiol 476, 517–531 (2024). https://doi.org/10.1007/s00424-024-02940-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-024-02940-1