Abstract
Chemosensory processes are integral to the physiology of most organisms. This function is typically performed by specialized cells that are able to detect input signals and to convert them to an output dedicated to a particular group of target cells. Tuft cells are cholinergic chemosensory epithelial cells capable of producing immunologically relevant effector molecules. They are scattered throughout endoderm-derived hollow organs and function as sensors of luminal stimuli, which has been best studied in mucosal barrier epithelia. Given their epithelial origin and broad distribution, and based on their interplay with immune pathways, tuft cells can be considered a prototypical example of how complex multicellular organisms engage innate immune mechanisms to modulate and optimize organ physiology. In this review, I provide a concise overview of tuft cells and discuss how these cells influence organ adaptation to dynamic luminal conditions.
Similar content being viewed by others
Introduction
Most organs in the body rely on chemosensory processes in order to respond appropriately to their environment. This is often enabled by specialized chemosensory cells that are capable of both detecting environmental cues and converting these inputs into usable signals that surrounding non-chemosensory cells can respond to. Over the past several decades, research by physiologists has identified tuft cells as important players in the chemosensation signal transduction pathway. Tuft cells, which are also known as brush cells, microvillous cells, caveolated cells, or solitary chemosensory cells, are relatively rare cholinergic chemosensory epithelial cells that are found in multiple different organs and that play a role in signal transduction across barrier epithelia. Tuft cells have been found to engage in innate immune responses to various microbial stimuli, a finding that has captured the attention of immunologists. Despite the recent interest in these fascinating epithelial chemosensory cells, the biology of tuft cells still remains relatively enigmatic. In this review, I provide an overview of tuft cell biology and summarize evidence for tuft cells contributing to both aversive reflexes and barrier tissue adaptation in response to changing environmental conditions.
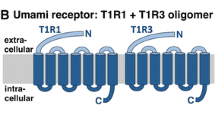
Historically, tuft cells were identified in epithelia of hollow organs by their apical microvillus-rich tuft with dense actin filaments and deep-reaching rootlets. These structures can be visualized by phalloidin, and morphologically distinguish tuft cells from other surrounding epithelial cells [1, 2]. In addition, tuft cells are enriched for a number of markers that are structural proteins or associated with structural proteins. Such markers include villin [3], advillin [4], and β-tubulin [5], which are all enriched in the apical tuft, as well as cytokeratin-18 [6] and the microtubule-associated serine/threonine-protein kinase DCLK1 (doublecortin-like and CAM kinase-like 1) [7]. A seminal finding by Höfer, Püschel, and Drenckhahn demonstrated that tuft cells in the intestine also express α-gustducin (guanine nucleotide-binding protein G(t) subunit α3; GNAT3) [8]. GNAT3 is a protein critically involved in the canonical taste transduction cascade employed by type II taste cells in the oral cavity, which detect sweet, bitter, and umami tastants. This surprising finding sparked subsequent studies by many groups, revealing that tuft cells across various organs express signaling components of the canonical taste transduction cascade (reviewed in [9]). In addition to GNAT3, these tuft cell-expressed signaling components include phospholipase Cβ2 (PLCβ2), the ER membrane calcium channel inositol-1,4,5-trisphosphate receptor (InsP3R), and the depolarizing calcium-activated cation channel TRPM5. Recent studies found that this expression program is relatively conserved in humans, including in tuft cells from the intestine [10,11,12].
Despite being able to identify tuft cells by both morphology and key protein markers, the developmental pathway associated with the tuft cell lineage is not well characterized. Aside from tuft cells’ strict reliance on the lineage-defining transcription factor POU2F3—another characteristic shared with type II taste cells—very little is known about the process of tuft cell lineage commitment. Interestingly, a number of additional transcription factors were found to be enriched in tuft cells relative to other epithelial cells, including Gfi-1b, SOX-9, and SPI-B. Their function, however, remains unclear. It is possible that these transcription factors are part of the machinery that regulates the differentiation from epithelial progenitors and the subsequent expression of the core tuft cell transcriptional program, a program which is overall strongly conserved in most tissues [13]. The striking similarities in gene expression among different organ-specific tuft cells suggest a shared core function. All tuft cells seem capable of detecting luminal (microbial) stimuli and relaying signals via taste signaling components, resulting in the release of appropriate effector molecules to not only neighboring epithelial cells but also to subepithelial immune and non-immune cells. While the core signaling pathways are highly conserved on a transcriptional level [13], there appears to be more diversity in the nature of the upstream stimuli that are detected, as well as the downstream effector modules. A brief summary of currently known physiological ligand-receptor pairs for tuft cells in different organs is provided in Table 1. It should be noted, however, that one has to be careful with this type of generalized conclusion regarding tuft cell biology, especially since most studies focused only on one particular organ.
A number of recent comprehensive reviews illuminated diverse aspects of tuft cell biology [26,27,28,29]. In the following sections, I will focus on currently known roles of tuft cells in aversive and adaptive responses in tissues. A summary of some of these interaction modules is provided in Fig. 1.
Summary of tuft cell interaction modules. Stimulation of tuft cells with luminal agonists triggers the release of one or multiple tuft cell effector molecules in a process that remains incompletely characterized. Known effector molecules include acetylcholine (various tissues), ATP (type II taste cells), IL-25 (small intestine), cysteinyl leukotrienes (CysLTs) (small intestine, airways), and prostaglandin D2 (PGD2) (small intestine, pancreas). Acetylcholine has a relatively broad action profile and is primarily associated with acute aversive responses in multiple organs via effects on ciliated cells and afferent nerve fibers (see text). ATP functions as a critical second messenger for the signaling of gustatory information from type II taste cells to afferent fibers in the oral taste buds [30]. IL-25 and CysLTs cooperatively stimulate the production of IL-13 and other type 2 cytokines in group 2 innate lymphoid cells (ILC2s) of the small intestine lamina propria (see text). Recent studies revealed roles of PGD2 in injury-associated pancreatic tumorigenesis [31] and small intestinal type 2 responses [32] through effects on incompletely defined immune and epithelial cell populations. IL-25 and tuft cell-derived eicosanoids appear to be predominantly involved in the regulation of epithelial remodeling
Tuft cells in acute aversive responses
The responses that tuft cells elicit in their interaction partners are suggested to be qualitatively analogous to those of taste cells stimulated with bitter tastants. This is supported by similarities in pathways engaged by tuft cells and type II taste cells, and the expression of certain bitter taste receptors (Tas2Rs) by some tuft cells. The physiological response to substances with a strong bitter taste is rejection, and such aversive behavior is thought to have evolved to protect the organism from potentially toxic molecules [33]. Taste perception, especially detection of a broad range of structurally diverse bitter substances through a large set of Tas2Rs, might be particularly important for omnivorous species. Omnivores diversified their food sources, and in doing so, were faced with both an increased risk of intoxication and a need to identify high caloric (sweet) food [34]. Advanced taste perception and an aversion to bitter tastants provided omnivores with an exquisite hazard-warning system. It would thus not surprise that the same physiology may have been adapted to other organs in an effort to induce similar physiological consequences in response to adverse stimuli. Tuft cells may possibly be an example of this adaptation, as there are many reports of stimulus-provoking agents being rejected based on signaling mediated by tuft cells.
Tuft cell chemosensation appears to be important in protecting the respiratory system. Tuft cells in the nasal epithelium responded to bacterial acyl-homoserine lactones by activating trigeminal afferents to evoke apnea and induce substance P release via cholinergic signaling, which also promoted mast cell degranulation and plasma leakage [14, 19, 20]. Certain bitter substances may be directly sensed by Tas2Rs expressed in ciliated cells of the human upper airways, as exposure to bitter substances resulted in nitric oxide-regulated increases in ciliary beat frequency [35]. In the lower airways, however, such regulation seems to occur on the level of tuft cells, as suggested by two recent studies in mice. Stimulation of tracheal tuft cells with Pseudomonas quinolones or formylated peptides engaged signaling via PLCβ2, InsP3R3, and TRPM5, and caused tuft cells to release acetylcholine, which promoted increased ciliary movement in surrounding ciliated cells [16, 17]. These studies reveal mechanistic insight into the involved signaling pathways and expand on prior reports, which demonstrated aversive respiratory responses following stimulation of mouse trachea epithelium with Tas2R agonists; specifically, the respiratory rate dropped and there was increased mucosal surface particle transport speed [18, 36]. Somewhat related, tuft cells at the entrance duct of the mouse vomeronasal organ regulated fluid access into this pheromone-sensing organ in order to protect the organ from harmful or irritating substances [37]. Interestingly, a tuft cell “hot-spot” can also be found in the stomach at the boundary between fundus and corpus, the so-called limiting ridge [38]. Multiple studies reported a decrease in gastric emptying following intragastric administration of bitter receptor agonists, and one study found this effect even more pronounced in Gnat3–/– mice [33, 39]. Further studies will help to identify the precise role of gastric tuft cells in regulating access or passage of luminal constituents to the corpus and further to the small intestine. Similarly, stimulation of urethral tuft cells with bitter and umami taste receptor ligands caused acetylcholine release, stimulation of sensory nerve fibers, and increased activity of the bladder detrusor muscle, which may be a protective reflex to flush out microbes and prevent ascending infections [40].
The gastrointestinal tract, in particular the small intestine, is another key location for tuft cell signaling. Several recent studies with a focus on tuft cells in the small intestine identified novel interaction modules with immune cells following detection of luminal parasites by tuft cells. Most notably, a feedforward circuit involving lamina propria-resident group 2 innate lymphoid cells (ILC2s) was shown to be enabled by tuft cell effector molecules such as IL-25 and leukotrienes [29]. Similar to their airway counterparts, small intestinal tuft cells required the canonical taste transduction components, GNAT3, PLCβ2, and TRPM5, for the response to the Tritrichomonas protist metabolite succinate downstream of the G protein-coupled receptor SUCNR1 [13, 23,24,25, 41]. However, SUCNR1 and GNAT3 were dispensable for the sensing of luminal worms which produce ligands and engage receptors of unknown nature [13]. While the tuft cell effector responses are critically involved in the expulsion of helminth model organisms from their intestinal niche, they differ considerably in kinetics when compared to the fast-acting protective and aversive reflexes that are mediated by tuft cells in the other tissues described above. In the Nippostrongylus brasiliensis helminth infection model, the peak of the tuft cell–ILC2 response and associated worm clearance is reached approximately 1 week after first exposure to the larvae in the small intestine [42, 43]. As in other tissues, tuft cell activation occurs instantly and secreted effector molecules can be detected a few minutes after stimulation in vitro [44, 45]. Release of preformed mediators from storage compartments could be involved, although evidence for this is currently lacking. It is more likely that some effector molecules may be generated on demand: tuft cells express an enzymatic machinery which enables the rapid synthesis of leukotrienes and other eicosanoid derivatives of arachidonic acid from membrane phospholipids following appropriate stimulation of competent cells [45]. This rapid synthesis is known to be regulated on multiple levels [46].
Il-25 is a key effector molecule for tuft cell function in response to helminth infection. IL-25 transcript, however, is expressed constitutively in tuft cells and remains unchanged upon helminth exposure [43, 45]. Tuft cell stimulation thus might control protein production on the posttranscriptional level, a process known to be used in the regulation of other cytokines [47]. Alternatively, secretion of stored IL-25 protein could be triggered upon tuft cell activation. IL-25 has a secretory signal peptide suggesting a conventional mode of secretion; an inhibitor of this pathway, Brefeldin A, was reported to block activation-induced IL-25 release [44]. Whether IL-25 is rerouted to storage vesicles or directly secreted following translation requires further study. Cleavage of IL-25 by matrix metalloproteinase 7 was reported to further enhance IL-25 activity in asthmatic airways [48]. Additional studies are needed to assess if proteolytic activation of IL-25 is a general mechanism of IL-25 regulation, specifically in the small intestine where functions of IL-25 are well understood.
Overall, tuft cells in the small intestine are capable of responding rapidly to stimuli, but the overall physiological response they invoke is delayed. The interaction module is rather slow between tuft cells that are constantly moving upwards within the epithelial “conveyor belt” along the intestinal crypt-villus axis, and the static ILC2s in the lamina propria. Soluble effectors from tuft cells have to first reach ILC2s, presumably through diffusion. ILC2s then have to induce their own transcriptional effector program that includes the canonical type 2 cytokines IL-5, IL-9, and IL-13, which are transcribed from readily accessible loci [49, 50]. Although studies using transcriptional reporter alleles have demonstrated that Il13 expression can be detected in ILC2s less than 24 h after oral gavage of helminths [45, 51], mounting a potent type 2 immune response appears to require continuous cross-talk between tuft cells, ILC2s, and the crypt epithelial progenitor compartment to alter epithelial composition (discussed in more detail below). While additional and more acute responses are conceivable, including communication with adjacent epithelial cells, stimulation of enteric neurons, and hypercontractility of smooth muscle, further study is warranted to establish a direct role of tuft cells in these processes.
When considering the tuft cell modules and defensive/aversive strategies of the gastrointestinal tract, interesting parallels with food allergy reactions emerge. Innocuous dietary antigens can elicit acute responses that have a strong type 2 immune component and involve players such as immunoglobulin E (IgE), mast cells, and basophils [52]. Physiological responses to these dietary antigens in the intestine include elevated mucus secretion, smooth muscle contractions, and acute diarrhea. It has been speculated that these are coordinated by a gastrointestinal food quality control system that can be trained to identify negative food value by associating adverse consequences of a harmful substance with a particular dietary constituent (antigen sensitization) [53]. Analogous to conditioned taste aversion (CTA), in which adverse consequences are associated with gustatory or olfactory cues in food [33], intestinal antigen sensitization (conditioning) and detection with high specificity upon subsequent re-exposure enables appropriate responses geared towards ridding the intestine of noxious chemicals. Such an alternative defensive strategy might provide another layer of protection and particularly benefit the organism when CTA is insufficient, perhaps due to absence of a strong taste or flavor or when such signals are outweighed in food with a very positive valence (e.g., a combination of high caloric food and an energy-deprived metabolic state). In exaggerated form and perhaps with hypersensitive predispositions, these physiological defense strategies can manifest as a food allergy [53]. More generally, it has been hypothesized that mechanisms of allergic (type 2 immune) responses have evolved as part of a complex physiological system that is particularly active at barrier sites and dedicated to aversion and expulsion of noxious substances, specifically environmental toxins [54]. This defensive system can cause undesired and pathological symptoms when unbalanced or targeted at a substance associated with common environmental antigens.
It will be interesting if and how tuft cell chemosensation and effector molecules are engaged in such responses at the intersection of gustatory and immune sensory mechanisms. A recent study provided some hints that there may be a role for tuft cells in these responses. Using a model of mechanical skin injury, the tuft cell–ILC2 circuit promoted mast cell expansion in the small intestine, which potentiated subsequent anaphylaxis to an oral antigen challenge [55]. Furthermore, data suggesting that activation of skin sensory neurons by leukotrienes can cause acute itch flares offers an opportunity for future studies into the largely unexplored area of intestinal tuft cell-neuron crosstalk via tuft cell-derived eicosanoids [56].
Tuft cells in tissue adaptation
Acute rejection in response to a stimulus is only one of the possible ways that tuft cells can respond to their environment. Depending on the localization, and perhaps the quality and/or quantity of the stimulus detected by tuft cells, the appropriate response may not be outright rejection of the stimulus, especially when expulsion is not an option. Indeed, an alternative strategy is the tolerization of a stimulus and the adaptation of the tissue to its presence. In humans, for example, there is a cultural history of developing an acquired taste for certain bitter food and drinks. Notably, experimental evidence suggests that a certain level of these “bitter” stimuli is not only tolerated but can have beneficial effects on organism physiology, specifically endocrine homeostasis (summarized in [57]). Integrating such a view into the role of tuft cells in barrier epithelia suggests that a possible favorable consequence of their stimulation with bitter ligands or other tuft cell agonists might be increased resilience to subsequent challenges with the same or related stimulus. This concept is supported by two aspects of tissue alterations often associated with tuft cell activation: an elevated anti-microbial state, and an expanding sensory (i.e., tuft cell) compartment. In most cases, however, the mechanisms that underlie these alterations are not well defined.
Tuft cells regulating an antimicrobial tissue state
Studies in multiple organs indicate that activated tuft cells are often associated with an elevated antimicrobial state of the local tissue. Stimulating bitter receptors on human sinonasal tuft cells can result in propagation of a calcium-dependent signal to surrounding epithelial cells, causing the release of broad-spectrum antimicrobial substances such as β-defensins 1 and 2 from adjacent epithelial cells [58]. Notably, such a mechanism was not found in cultures from human bronchial epithelium nor mouse nasal epithelium, which suggests possible regional and species-specific tuft cell signaling pathways. Tuft cells in mouse gingival junctional epithelium express several bitter Tas2Rs and their activation results in upregulated expression of β-defensin-3 in gingival tissue, which is abrogated in Gnat3–/– mice [59]. Physiological consequences of defective antimicrobial responses in these Gnat3–/– mice were found to be an altered oral microbiota and an accelerated alveolar bone loss under homeostatic conditions; pathologies were further exacerbated in a model of ligature-induced periodontitis. For both the gingival tissue and the alveolar bone, the relevant tuft cell effector molecule as well as its precise target cell population are unclear. Because gingival tuft cells lack detectable expression of choline acetyltransferase (ChAT), which can be found in tuft cells of most tissues, they might employ factors other than acetylcholine for communication with their neighboring cells [59].
In the small intestine, Paneth cells constitute an important constitutive source of antimicrobial peptides. Mice deficient in Paneth cell lysozyme display altered gut bacterial landscape, which is associated with increased tuft cell frequencies [60]. There is currently no data, however, that would suggest a direct cross-talk between tuft cells and Paneth cells. The prototypical immune regulators of intestinal antimicrobial proteins are IL-22 and IL-17, although a potential link between the bactericidal protein angiogenin 4 and IL-13 was reported for the colon [61]. Consequences of tuft cells activation in the small intestine are primarily associated with canonical antihelminthic responses [41,42,43]. These effects are thought to be mediated predominantly by promoting expression of type 2 cytokines in ILC2s, in particular IL-13, which drives goblet cell hyperplasia and the production of mucins and resistin-like molecule-β (RELMβ) [62]. An elevated type 2 immune tone in the small intestine was associated with increased resistance to helminth infection [25], though the individual contribution of different effector mechanisms were not definitively clarified. Similarly, pre-conditioning the intestine by treating mice with effector cytokines IL-25 and IL-4 before or at the time of helminth arrival in the small intestine lumen results in rapid worm clearance [63, 64]. Whether small intestinal tuft cells directly communicate with adjacent epithelial cells and neurons, as their counterparts do in other tissues, requires further study. Notably, a recent study reported that small intestinal tuft cells can directly act on epithelial progenitor cells and goblet cells through secretion of prostaglandin D2, which negatively regulates the epithelial response to type 2 cytokines during helminth infections [32].
Although these examples suggest a link between the antimicrobial state of an organ and tuft cell activation, further study is required to determine to which extent tuft cell signaling enables the host to regulate the composition of its eukaryotic and prokaryotic microbiota, and what the consequences are if tuft cell responsiveness is impaired. Increasing resolution of microbial metagenomic analysis and microbiota characterization will be helpful in gaining a deeper understanding of this biology.
The luminal microbial state regulates tuft cell abundance
Another interesting feature of tuft cell activation is that it can further expand the pool of tuft cells. This effect is most dramatic in the small intestine, where tuft cell-derived effector molecules stimulate IL-13 production by ILC2s, which directly promotes tuft cell (as well as goblet cell) fate in epithelial progenitors [41,42,43]. The mechanism for this fate specification, however, has yet to be defined. As a consequence of the high cellular turnover in the epithelium of the small intestine, the frequency of tuft cells can increase by more than tenfold within just a few days when luminal parasites are present. In helminth infections, this constitutes an essential feed-forward response circuit that elevates the number of cells that produce effector molecules (including tuft cells); these effector molecules then drive worm expulsion [42, 43]. The intestinal microbial colonization state also determines the abundance of tuft cells in the small intestine, which can reach a stable equilibrium. This equilibrium depends on the cross-talk between tuft cells and ILC2s [25, 41]. Chronic activation of the tuft cell–ILC2 circuit, while generally well tolerated, can significantly impact the small intestinal tissue and can promote an increase in overall small bowel length [25]. Notably, small intestine tuft cell populations can also increase due to perturbation of the bacterial microbiota. This effect was noted in mice treated with streptomycin or polyethylene glycol 3350, in mice with an abrogated secretory cell differentiation, which lack Paneth cells, and in mice deficient in Paneth cell lysozyme (Lyz1) [24, 60, 65]. While some of these studies identified increased bacterial succinate production as a driving force, similar to the findings with Tritrichomonas protists, the physiological consequences of this response remain unclear. Interestingly, fewer tuft cells were detected in samples from patients affected by inflammatory diseases of the small bowel relative to specimens from unaffected individuals [65, 66].
In comparison to the small intestine, alterations in tuft cell abundance in other tissues are more subtle and the mechanisms that underlie these epithelial remodeling events are less well understood. Mice deficient in TLR2, TLR4, or MyD88—key components in detection of microbial ligands—displayed a reduction in tuft cells in the urethra and trachea, whereas no difference was noted between germ-free and SPF wildtype mice [67]. Moderate expansion of airway tuft cells was found following fungal or mite aeroallergen exposure in mice [68]; a similar increase in abundance was reported for patients with chronic rhinosinusitis with nasal polyposis (CRSwNP) and allergic fungal rhinosinusitis [69, 70]. Further studies are required to determine whether tuft cell sensory function is a necessary upstream event in promoting their own expansion in tissues outside the gut. Notably, tuft cells can also emerge in tissues where they have not previously existed following remodeling associated with metaplasia and inflammation, a phenomenon that was observed in the pancreas and distal lung [71,72,73]. These findings suggest that diverse changes to the tissue state can promote tuft cell lineage commitment.
It is unclear why epithelial tissues adapt tuft cell abundance to a particular luminal state. One reason could be that it increases both the number of sensory cells and effector molecule sources, thereby lowering the threshold and increasing the amplitude of a response following exposure to the same or related stimulus. De novo differentiation of tuft cells may also provide a mechanism to alter the overall quality of tuft cells, which could be an additional way to finetune tissue responses. Heterogeneity in tuft cells has been reported for the trachea and small intestine, and, in the latter, the composition was shifted following helminth infection [74, 75]. Notably, diversity in small intestinal tuft cells appears to be in part driven by zonated transcriptional programs along the crypt-villus axis [76]. Luminal signals may therefore influence tuft cell heterogeneity at the level of their differentiation from epithelial progenitor cells and/or by directly or indirectly altering gene expression in mature tuft cells. Interestingly, elevated urinary catecholamine levels and increased energy expenditure were found in Pou2f3–/– mice which lack all tuft cells and type II taste cells [77]. These findings suggest that changes in certain tuft cell populations might have an impact on organismal energy homeostasis. However, additional work will be necessary to establish such a model.
Overall, these concepts are largely driven by a host-centric view and could be modified to fit a more complex host-parasite relationship. Perhaps, certain parasites deliberately stimulate tuft cells and induce aspects of the abovementioned adaptation to their own benefit, such that they can modify their nutrient accessibility or have a selective advantage over newly invading microbial competitors for the same niche. Interestingly, expulsion of evolutionarily adapted parasites, including some intestinal helminths, is often limited or, in the case of Tritrichomonas, even completely absent [41, 78]. Despite their limited expulsion, these organisms stimulate the tuft cell–ILC2 circuit and raise the overall type 2 tissue tone, suggesting a possible benefit of this environment for some parasites. There is, however, clear evidence for enhanced parasite fecundity in the absence of tuft cells or their critical effector molecule, IL-25, indicating an important and dominant host-centric immune function of tuft cells in defending against parasites [42, 79]. Long-term reproductive fitness and success of parasites, however, has not been compared under natural conditions with variable food composition and with many different species competing for similar luminal niches. Under these conditions, stimulation of the tuft cell-ILC2 circuit may suddenly become a beneficial trait for particular parasite species.
Conclusions and future directions
Studies by many groups over the past few years have established a number of tuft cell agonists, primarily of microbial origin, and a limited repertoire of secreted effector molecules through which tuft cells interact with other cells, including neurons, epithelial cells, and immune cells. While this research identified diverse roles of tuft cells in shaping aversive and adaptive responses to luminal stimuli in different tissues, there is still much more to learn about these cells. In complex organisms, processes in different organs are often cross-regulated and these interactions can induce a state of preparedness prior to exposure to a stimulus that shifts the system away from baseline activity. Hormonal and neuronal pathways are often engaged to promote such anticipatory responses. A classic example is the cephalic phase of digestion when sensory inputs prepare the gastrointestinal tract for the upcoming food processing and nutrient absorption by regulating a significant fraction of the overall secretory activity in organs such as stomach and pancreas before the arrival of food in the gut [80]. Notably, oral bitter taste stimulation can elicit nausea and influence food intake and intestinal motility through effects on a number of physiological pathways, which can be summarized as anticipatory responses in the intestine that confer a prophylactic aversive state [57, 81]. It will be interesting to investigate whether tuft cell activation in one tissue can have physiological consequences in spatially separated tissues. Also, it is unclear if the quality of a stimulus can determine the outcome, i.e., the type of effector molecule that is secreted following ligand detection, and if this is mediated by different types of tuft cells or one cell that is able to discriminate between different agonists. Moreover, the role of immune-related effectors, IL-25 and CysLTs, outside of the small intestine, and the function of acetylcholine produced by tuft cells in the small intestine remain largely unknown. In terms of cellular physiology, the relevance of various interesting morphologic features of tuft cells remains incompletely understood [2, 82]. On the translational side, one can imagine that certain tuft cell signaling pathways may be targetable to increase resilience in particular tissues or to prevent pathologies related to type 2 inflammation.
Over the past years, multiple studies illuminated various aspects of tuft cell biology in diverse tissues and contexts. With the increasing interest in tuft cells stimulating interactions between physiologist, immunologist, and epithelial biologists, we can expect to learn much more about these cells and their impact on organism health in the near future.
References
Gerbe F, van Es JH, Makrini L, Brulin B, Mellitzer G, Robine S, Romagnolo B, Shroyer NF, Bourgaux JF, Pignodel C, Clevers H, Jay P (2011) Distinct ATOH1 and Neurog3 requirements define tuft cells as a new secretory cell type in the intestinal epithelium. J Cell Biol 192:767–780. https://doi.org/10.1083/jcb.201010127
Sato A (2007) Tuft cells. Anat Sci Int 82:187–199. https://doi.org/10.1111/j.1447-073X.2007.00188.x
Hofer D, Drenckhahn D (1992) Identification of brush cells in the alimentary and respiratory system by antibodies to villin and fimbrin. Histochem 98:237–242. https://doi.org/10.1007/BF00271037
Ruppert AL, Keshavarz M, Winterberg S, Oberwinkler J, Kummer W, Schutz B (2020) Advillin is a tuft cell marker in the mouse alimentary tract. J Mol Histol 51:421–435. https://doi.org/10.1007/s10735-020-09893-6
Hofer D, Drenckhahn D (1996) Cytoskeletal markers allowing discrimination between brush cells and other epithelial cells of the gut including enteroendocrine cells. Histochem Cell Biol 105:405–412. https://doi.org/10.1007/BF01463662
Kasper M, Hofer D, Woodcock-Mitchell J, Migheli A, Attanasio A, Rudolf T, Muller M, Drenckhahn D (1994) Colocalization of cytokeratin 18 and villin in type III alveolar cells (brush cells) of the rat lung. Histochem 101:57–62. https://doi.org/10.1007/BF00315832
Gerbe F, Brulin B, Makrini L, Legraverend C, Jay P (2009) DCAMKL-1 expression identifies Tuft cells rather than stem cells in the adult mouse intestinal epithelium. Gastroenterology 137:2179-2180; author reply 2180-2171. https://doi.org/10.1053/j.gastro.2009.06.072
Hofer D, Puschel B, Drenckhahn D (1996) Taste receptor-like cells in the rat gut identified by expression of alpha-gustducin. Proc Natl Acad Sci U S A 93:6631–6634. https://doi.org/10.1073/pnas.93.13.6631
O’Leary CE, Schneider C, Locksley RM (2019) Tuft cells-systemically dispersed sensory epithelia integrating immune and neural circuitry. In: Yokoyama WM (ed) Annual Review of Immunology, Vol 37, 2019, vol 37. Annual Review of Immunology. pp 47-72. https://doi.org/10.1146/annurev-immunol-042718-041505
Elmentaite R, Kumasaka N, Roberts K, Fleming A, Dann E, King HW, Kleshchevnikov V, Dabrowska M, Pritchard S, Bolt L, Vieira SF, Mamanova L, Huang N, Perrone F, Goh Kai’En I, Lisgo SN, Katan M, Leonard S, Oliver TRW, Hook CE, Nayak K, Campos LS, Dominguez Conde C, Stephenson E, Engelbert J, Botting RA, Polanski K, van Dongen S, Patel M, Morgan MD, Marioni JC, Bayraktar OA, Meyer KB, He X, Barker RA, Uhlig HH, Mahbubani KT, Saeb-Parsy K, Zilbauer M, Clatworthy MR, Haniffa M, James KR, Teichmann SA (2021) Cells of the human intestinal tract mapped across space and time. Nature 597:250–255. https://doi.org/10.1038/s41586-021-03852-1
Schutz B, Ruppert AL, Strobel O, Lazarus M, Urade Y, Buchler MW, Weihe E (2019) Distribution pattern and molecular signature of cholinergic tuft cells in human gastro-intestinal and pancreatic-biliary tract. Sci reports 9:17466. https://doi.org/10.1038/s41598-019-53997-3
Smillie CS, Biton M, Ordovas-Montanes J, Sullivan KM, Burgin G, Graham DB, Herbst RH, Rogel N, Slyper M, Waldman J, Sud M, Andrews E, Velonias G, Haber AL, Jagadeesh K, Vickovic S, Yao J, Stevens C, Dionne D, Nguyen LT, Villani AC, Hofree M, Creasey EA, Huang H, Rozenblatt-Rosen O, Garber JJ, Khalili H, Desch AN, Daly MJ, Ananthakrishnan AN, Shalek AK, Xavier RJ, Regev A (2019) Intra- and inter-cellular rewiring of the human colon during ulcerative colitis. Cell 178(714–730):e722. https://doi.org/10.1016/j.cell.2019.06.029
Nadjsombati MS, McGinty JW, Lyons-Cohen MR, Jaffe JB, DiPeso L, Schneider C, Miller CN, Pollack JL, Nagana Gowda GA, Fontana MF, Erle DJ, Anderson MS, Locksley RM, Raftery D, von Moltke J (2018) Detection of succinate by intestinal tuft cells triggers a type 2 innate immune circuit. Immun 49(33–41):e37. https://doi.org/10.1016/j.immuni.2018.06.016
Finger TE, Bottger B, Hansen A, Anderson KT, Alimohammadi H, Silver WL (2003) Solitary chemoreceptor cells in the nasal cavity serve as sentinels of respiration. Proc Natl Acad Sci U S A 100:8981–8986. https://doi.org/10.1073/pnas.1531172100
Gulbransen BD, Clapp TR, Finger TE, Kinnamon SC (2008) Nasal solitary chemoreceptor cell responses to bitter and trigeminal stimulants in vitro. J Neurophysiol 99:2929–2937. https://doi.org/10.1152/jn.00066.2008
Perniss A, Liu S, Boonen B, Keshavarz M, Ruppert AL, Timm T, Pfeil U, Soultanova A, Kusumakshi S, Delventhal L, Aydin O, Pyrski M, Deckmann K, Hain T, Schmidt N, Ewers C, Gunther A, Lochnit G, Chubanov V, Gudermann T, Oberwinkler J, Klein J, Mikoshiba K, Leinders-Zufall T, Offermanns S, Schutz B, Boehm U, Zufall F, Bufe B, Kummer W (2020) Chemosensory cell-derived acetylcholine drives tracheal mucociliary clearance in response to virulence-associated formyl peptides. Immunity 52(683–699):e611. https://doi.org/10.1016/j.immuni.2020.03.005
Hollenhorst MI, Jurastow I, Nandigama R, Appenzeller S, Li L, Vogel J, Wiederhold S, Althaus M, Empting M, Altmuller J, Hirsch AKH, Flockerzi V, Canning BJ, Saliba AE, Krasteva-Christ G (2020) Tracheal brush cells release acetylcholine in response to bitter tastants for paracrine and autocrine signaling. FASEB J 34:316–332. https://doi.org/10.1096/fj.201901314RR
Krasteva G, Canning BJ, Papadakis T, Kummer W (2012) Cholinergic brush cells in the trachea mediate respiratory responses to quorum sensing molecules. Life Sci 91:992–996. https://doi.org/10.1016/j.lfs.2012.06.014
Saunders CJ, Christensen M, Finger TE, Tizzano M (2014) Cholinergic neurotransmission links solitary chemosensory cells to nasal inflammation. Proc Natl Acad Sci U S A 111:6075–6080. https://doi.org/10.1073/pnas.1402251111
Tizzano M, Gulbransen BD, Vandenbeuch A, Clapp TR, Herman JP, Sibhatu HM, Churchill ME, Silver WL, Kinnamon SC, Finger TE (2010) Nasal chemosensory cells use bitter taste signaling to detect irritants and bacterial signals. Proc Natl Acad Sci U S A 107:3210–3215. https://doi.org/10.1073/pnas.0911934107
Fu Z, Ogura T, Luo W, Lin W (2018) ATP and odor mixture activate TRPM5-expressing microvillous cells and potentially induce acetylcholine release to enhance supporting cell endocytosis in mouse main olfactory epithelium. Front Cell Neurosci 12:71. https://doi.org/10.3389/fncel.2018.00071
Ualiyeva S, Hallen N, Kanaoka Y, Ledderose C, Matsumoto I, Junger WG, Barrett NA, Bankova LG (2020) Airway brush cells generate cysteinyl leukotrienes through the ATP sensor P2Y2. Sci Immunol 5. https://doi.org/10.1126/sciimmunol.aax7224
Howitt MR, Cao YG, Gologorsky MB, Li JA, Haber AL, Biton M, Lang J, Michaud M, Regev A, Garrett WS (2020) The taste receptor TAS1R3 regulates small intestinal tuft cell homeostasis. Immunohorizons 4:23–32. https://doi.org/10.4049/immunohorizons.1900099
Lei W, Ren W, Ohmoto M, Urban JF Jr, Matsumoto I, Margolskee RF, Jiang P (2018) Activation of intestinal tuft cell-expressed Sucnr1 triggers type 2 immunity in the mouse small intestine. Proc Natl Acad Sci U S A 115:5552–5557. https://doi.org/10.1073/pnas.1720758115
Schneider C, O’Leary CE, von Moltke J, Liang H-E, Ang QY, Turnbaugh PJ, Radhakrishnan S, Pellizzon M, Ma A, Locksley RM (2018) A metabolite-triggered tuft cell-ILC2 circuit drives small intestinal remodeling. Cell 174:271-+. https://doi.org/10.1016/j.cell.2018.05.014
Billipp TE, Nadjsombati MS, von Moltke J (2021) Tuning tuft cells: new ligands and effector functions reveal tissue-specific function. Curr Opinion Immunol 68:98–106. https://doi.org/10.1016/j.coi.2020.09.006
Nevo S, Kadouri N, Abramson J (2019) Tuft cells: from the mucosa to the thymus. Immunol Lett 210:1–9. https://doi.org/10.1016/j.imlet.2019.02.003
O’Leary CE, Schneider C, Locksley RM (2019) Tuft cells-systemically dispersed sensory epithelia integrating immune and neural circuitry. Annu Rev Immunol 37:47–72. https://doi.org/10.1146/annurev-immunol-042718-041505
Schneider C, O’Leary CE, Locksley RM (2019) Regulation of immune responses by tuft cells. Nat Rev Immunol 19:584–593. https://doi.org/10.1038/s41577-019-0176-x
Finger TE, Danilova V, Barrows J, Bartel DL, Vigers AJ, Stone L, Hellekant G, Kinnamon SC (2005) ATP signaling is crucial for communication from taste buds to gustatory nerves. Science (New York, NY) 310:1495–1499. https://doi.org/10.1126/science.1118435
DelGiorno KE, Chung CY, Vavinskaya V, Maurer HC, Novak SW, Lytle NK, Ma Z, Giraddi RR, Wang D, Fang L, Naeem RF, Andrade LR, Ali WH, Tseng H, Tsui C, Gubbala VB, Ridinger-Saison M, Ohmoto M, Erikson GA, O’Connor C, Shokhirev MN, Hah N, Urade Y, Matsumoto I, Kaech SM, Singh PK, Manor U, Olive KP, Wahl GM (2020) Tuft cells inhibit pancreatic tumorigenesis in mice by producing prostaglandin D2. Gastroenterol 159(1866–1881):e1868. https://doi.org/10.1053/j.gastro.2020.07.037
Oyesola OO, Shanahan MT, Kanke M, Mooney BM, Webb LM, Smita S, Matheson MK, Campioli P, Pham D, Fruh SP, McGinty JW, Churchill MJ, Cahoon JL, Sundaravaradan P, Flitter BA, Mouli K, Nadjsombati MS, Kamynina E, Peng SA, Cubitt RL, Gronert K, Lord JD, Rauch I, von Moltke J, Sethupathy P, Tait Wojno ED (2021) PGD2 and CRTH2 counteract type 2 cytokine-elicited intestinal epithelial responses during helminth infection. J Exp Med 218. https://doi.org/10.1084/jem.20202178
Schier LA, Spector AC (2019) The functional and neurobiological properties of bad taste. Physiol Rev 99:605–663. https://doi.org/10.1152/physrev.00044.2017
Breslin PA (2013) An evolutionary perspective on food and human taste. Curr Biol 23:R409-418. https://doi.org/10.1016/j.cub.2013.04.010
Lee RJ, Xiong G, Kofonow JM, Chen B, Lysenko A, Jiang P, Abraham V, Doghramji L, Adappa ND, Palmer JN, Kennedy DW, Beauchamp GK, Doulias PT, Ischiropoulos H, Kreindler JL, Reed DR, Cohen NA (2012) T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J Clin Investigation 122:4145–4159. https://doi.org/10.1172/JCI64240
Krasteva G, Canning BJ, Hartmann P, Veres TZ, Papadakis T, Muhlfeld C, Schliecker K, Tallini YN, Braun A, Hackstein H, Baal N, Weihe E, Schutz B, Kotlikoff M, Ibanez-Tallon I, Kummer W (2011) Cholinergic chemosensory cells in the trachea regulate breathing. Proc Natl Acad Sci U S A 108:9478–9483. https://doi.org/10.1073/pnas.1019418108
Ogura T, Krosnowski K, Zhang L, Bekkerman M, Lin W (2010) Chemoreception regulates chemical access to mouse vomeronasal organ: role of solitary chemosensory cells. PloS one 5:e11924. https://doi.org/10.1371/journal.pone.0011924
Hass N, Schwarzenbacher K, Breer H (2007) A cluster of gustducin-expressing cells in the mouse stomach associated with two distinct populations of enteroendocrine cells. Histochem Cell Biol 128:457–471. https://doi.org/10.1007/s00418-007-0325-3
Janssen S, Laermans J, Verhulst PJ, Thijs T, Tack J, Depoortere I (2011) Bitter taste receptors and alpha-gustducin regulate the secretion of ghrelin with functional effects on food intake and gastric emptying. Proc Natl Acad Sci U S A 108:2094–2099. https://doi.org/10.1073/pnas.1011508108
Deckmann K, Filipski K, Krasteva-Christ G, Fronius M, Althaus M, Rafiq A, Papadakis T, Renno L, Jurastow I, Wessels L, Wolff M, Schutz B, Weihe E, Chubanov V, Gudermann T, Klein J, Bschleipfer T, Kummer W (2014) Bitter triggers acetylcholine release from polymodal urethral chemosensory cells and bladder reflexes. Proc Natl Acad Sci U S A 111:8287–8292. https://doi.org/10.1073/pnas.1402436111
Howitt MR, Lavoie S, Michaud M, Blum AM, Tran SV, Weinstock JV, Gallini CA, Redding K, Margolskee RF, Osborne LC, Artis D, Garrett WS (2016) Tuft cells, taste-chemosensory cells, orchestrate parasite type 2 immunity in the gut. Sci (New York, NY) 351:1329–1333. https://doi.org/10.1126/science.aaf1648
Gerbe F, Sidot E, Smyth DJ, Ohmoto M, Matsumoto I, Dardalhon V, Cesses P, Garnier L, Pouzolles M, Brulin B, Bruschi M, Harcus Y, Zimmermann VS, Taylor N, Maizels RM, Jay P (2016) Intestinal epithelial tuft cells initiate type 2 mucosal immunity to helminth parasites. Nature 529:226–230. https://doi.org/10.1038/nature16527
von Moltke J, Ji M, Liang HE, Locksley RM (2016) Tuft-cell-derived IL-25 regulates an intestinal ILC2-epithelial response circuit. Nature 529:221–225. https://doi.org/10.1038/nature16161
Luo XC, Chen ZH, Xue JB, Zhao DX, Lu C, Li YH, Li SM, Du YW, Liu Q, Wang P, Liu M, Huang L (2019) Infection by the parasitic helminth Trichinella spiralis activates a Tas2r-mediated signaling pathway in intestinal tuft cells. Proc Natl Acad Sci U S A 116:5564–5569. https://doi.org/10.1073/pnas.1812901116
McGinty JW, Ting HA, Billipp TE, Nadjsombati MS, Khan DM, Barrett NA, Liang HE, Matsumoto I, von Moltke J (2020) Tuft-cell-derived leukotrienes drive rapid anti-helminth immunity in the small intestine but are dispensable for anti-protist immunity. Immun 52(528–541):e527. https://doi.org/10.1016/j.immuni.2020.02.005
Haeggstrom JZ, Funk CD (2011) Lipoxygenase and leukotriene pathways: biochemistry, biology, and roles in disease. Chem Rev 111:5866–5898. https://doi.org/10.1021/cr200246d
Salerno F, Turner M, Wolkers MC (2020) Dynamic post-transcriptional events governing CD8(+) T cell homeostasis and effector function. Trends Immunol 41:240–254. https://doi.org/10.1016/j.it.2020.01.001
Goswami S, Angkasekwinai P, Shan M, Greenlee KJ, Barranco WT, Polikepahad S, Seryshev A, Song LZ, Redding D, Singh B, Sur S, Woodruff P, Dong C, Corry DB, Kheradmand F (2009) Divergent functions for airway epithelial matrix metalloproteinase 7 and retinoic acid in experimental asthma. Nat Immunol 10:496–503. https://doi.org/10.1038/ni.1719
Shih HY, Sciume G, Mikami Y, Guo L, Sun HW, Brooks SR, Urban JF Jr, Davis FP, Kanno Y, O’Shea JJ (2016) Developmental acquisition of regulomes underlies innate lymphoid cell functionality. Cell 165:1120–1133. https://doi.org/10.1016/j.cell.2016.04.029
Van Dyken SJ, Nussbaum JC, Lee J, Molofsky AB, Liang HE, Pollack JL, Gate RE, Haliburton GE, Ye CJ, Marson A, Erle DJ, Locksley RM (2016) A tissue checkpoint regulates type 2 immunity. Nat Immunol 17:1381–1387. https://doi.org/10.1038/ni.3582
O’Leary CE, Feng X, Cortez VS, Locksley RM, Schneider C (2021) Interrogating the small intestine tuft cell-ILC2 circuit using in vivo manipulations. Curr Protoc 1:e77. https://doi.org/10.1002/cpz1.77
Renz H, Allen KJ, Sicherer SH, Sampson HA, Lack G, Beyer K, Oettgen HC (2018) Food allergy. Nat Rev Dis Primers 4:17098. https://doi.org/10.1038/nrdp.2017.98
Florsheim EB, Sullivan ZA, Khoury-Hanold W, Medzhitov R (2021) Food allergy as a biological food quality control system. Cell 184:1440–1454. https://doi.org/10.1016/j.cell.2020.12.007
Profet M (1991) The function of allergy: immunological defense against toxins. Q Rev Biol 66:23–62. https://doi.org/10.1086/417049
Leyva-Castillo JM, Galand C, Kam C, Burton O, Gurish M, Musser MA, Goldsmith JD, Hait E, Nurko S, Brombacher F, Dong C, Finkelman FD, Lee RT, Ziegler S, Chiu I, Austen KF, Geha RS (2019) Mechanical skin injury promotes food anaphylaxis by driving intestinal mast cell expansion. Immun 50(1262–1275):e1264. https://doi.org/10.1016/j.immuni.2019.03.023
Wang F, Trier AM, Li F, Kim S, Chen Z, Chai JN, Mack MR, Morrison SA, Hamilton JD, Baek J, Yang TB, Ver Heul AM, Xu AZ, Xie Z, Dong X, Kubo M, Hu H, Hsieh CS, Dong X, Liu Q, Margolis DJ, Ardeleanu M, Miller MJ, Kim BS (2021) A basophil-neuronal axis promotes itch. Cell 184(422–440):e417. https://doi.org/10.1016/j.cell.2020.12.033
Harmon CP, Deng D, Breslin PAS (2021) Bitter taste receptors (T2Rs) are sentinels that coordinate metabolic and immunological defense responses. Curr Opin Physiol 20:70–76. https://doi.org/10.1016/j.cophys.2021.01.006
Lee RJ, Kofonow JM, Rosen PL, Siebert AP, Chen B, Doghramji L, Xiong G, Adappa ND, Palmer JN, Kennedy DW, Kreindler JL, Margolskee RF, Cohen NA (2014) Bitter and sweet taste receptors regulate human upper respiratory innate immunity. J Clin Investigation 124:1393–1405. https://doi.org/10.1172/JCI72094
Zheng X, Tizzano M, Redding K, He J, Peng X, Jiang P, Xu X, Zhou X, Margolskee RF (2019) Gingival solitary chemosensory cells are immune sentinels for periodontitis. Nat Commun 10:4496. https://doi.org/10.1038/s41467-019-12505-x
Yu S, Balasubramanian I, Laubitz D, Tong K, Bandyopadhyay S, Lin X, Flores J, Singh R, Liu Y, Macazana C, Zhao Y, Beguet-Crespel F, Patil K, Midura-Kiela MT, Wang D, Yap GS, Ferraris RP, Wei Z, Bonder EM, Haggblom MM, Zhang L, Douard V, Verzi MP, Cadwell K, Kiela PR, Gao N (2020) Paneth cell-derived lysozyme defines the composition of mucolytic microbiota and the inflammatory tone of the intestine. Immunity 53(398–416):e398. https://doi.org/10.1016/j.immuni.2020.07.010
Steenwinckel V, Louahed J, Lemaire MM, Sommereyns C, Warnier G, McKenzie A, Brombacher F, Van Snick J, Renauld JC (2009) IL-9 promotes IL-13-dependent paneth cell hyperplasia and regulation of innate immunity mediators in intestinal mucosa. J Immunol (Baltimore, Md: 1950) 182:4737–4743. https://doi.org/10.4049/jimmunol.0801941
Sorobetea D, Svensson-Frej M, Grencis R (2018) Immunity to gastrointestinal nematode infections. Mucosal Immunol 11:304–315. https://doi.org/10.1038/mi.2017.113
Fallon PG, Ballantyne SJ, Mangan NE, Barlow JL, Dasvarma A, Hewett DR, McIlgorm A, Jolin HE, McKenzie AN (2006) Identification of an interleukin (IL)-25-dependent cell population that provides IL-4, IL-5, and IL-13 at the onset of helminth expulsion. J Exp Med 203:1105–1116. https://doi.org/10.1084/jem.20051615
Urban JF Jr, Maliszewski CR, Madden KB, Katona IM, Finkelman FD (1995) IL-4 treatment can cure established gastrointestinal nematode infections in immunocompetent and immunodeficient mice. J immunol (Baltimore Md: 1950) 154:4675–4684
Banerjee A, Herring CA, Chen B, Kim H, Simmons AJ, Southard-Smith AN, Allaman MM, White JR, Macedonia MC, McKinley ET, Ramirez-Solano MA, Scoville EA, Liu Q, Wilson KT, Coffey RJ, Washington MK, Goettel JA, Lau KS (2020) Succinate produced by intestinal microbes promotes specification of tuft cells to suppress ileal inflammation. Gastroenterol 159(2101–2115):e2105. https://doi.org/10.1053/j.gastro.2020.08.029
Huh WJ, Roland JT, Asai M, Kaji I (2020) Distribution of duodenal tuft cells is altered in pediatric patients with acute and chronic enteropathy. Biomed Res 41:113–118. https://doi.org/10.2220/biomedres.41.113
Perniss A, Schmidt P, Soultanova A, Papadakis T, Dahlke K, Voigt A, Schutz B, Kummer W, Deckmann K (2021) Development of epithelial cholinergic chemosensory cells of the urethra and trachea of mice. Cell and tissue research. https://doi.org/10.1007/s00441-021-03424-9
Bankova LG, Dwyer DF, Yoshimoto E, Ualiyeva S, McGinty JW, Raff H, von Moltke J, Kanaoka Y, Frank Austen K, Barrett NA (2018) The cysteinyl leukotriene 3 receptor regulates expansion of IL-25-producing airway brush cells leading to type 2 inflammation. Sci Immunol 3. https://doi.org/10.1126/sciimmunol.aat9453
Kohanski MA, Workman AD, Patel NN, Hung LY, Shtraks JP, Chen B, Blasetti M, Doghramji L, Kennedy DW, Adappa ND, Palmer JN, Herbert DR, Cohen NA (2018) Solitary chemosensory cells are a primary epithelial source of IL-25 in patients with chronic rhinosinusitis with nasal polyps. J allergy Clin Immunol 142(460–469):e467. https://doi.org/10.1016/j.jaci.2018.03.019
Patel NN, Triantafillou V, Maina IW, Workman AD, Tong CCL, Kuan EC, Papagiannopoulos P, Bosso JV, Adappa ND, Palmer JN, Kohanski MA, Herbert DR, Cohen NA (2019) Fungal extracts stimulate solitary chemosensory cell expansion in noninvasive fungal rhinosinusitis. Int Forum Allergy Rhinol 9:730–737. https://doi.org/10.1002/alr.22334
Bailey JM, Alsina J, Rasheed ZA, McAllister FM, Fu YY, Plentz R, Zhang H, Pasricha PJ, Bardeesy N, Matsui W, Maitra A, Leach SD (2014) DCLK1 marks a morphologically distinct subpopulation of cells with stem cell properties in preinvasive pancreatic cancer. Gastroenterol 146:245–256. https://doi.org/10.1053/j.gastro.2013.09.050
Delgiorno KE, Hall JC, Takeuchi KK, Pan FC, Halbrook CJ, Washington MK, Olive KP, Spence JR, Sipos B, Wright CV, Wells JM, Crawford HC (2014) Identification and manipulation of biliary metaplasia in pancreatic tumors. Gastroenterology 146(233–244):e235. https://doi.org/10.1053/j.gastro.2013.08.053
Rane CK, Jackson SR, Pastore CF, Zhao G, Weiner AI, Patel NN, Herbert DR, Cohen NA, Vaughan AE (2019) Development of solitary chemosensory cells in the distal lung after severe influenza injury. Am J Physiol Lung Cell Mol Physiol 316:L1141–L1149. https://doi.org/10.1152/ajplung.00032.2019
Haber AL, Biton M, Rogel N, Herbst RH, Shekhar K, Smillie C, Burgin G, Delorey TM, Howitt MR, Katz Y, Tirosh I, Beyaz S, Dionne D, Zhang M, Raychowdhury R, Garrett WS, Rozenblatt-Rosen O, Shi HN, Yilmaz O, Xavier RJ, Regev A (2017) A single-cell survey of the small intestinal epithelium. Nature 551:333–339. https://doi.org/10.1038/nature24489
Montoro DT, Haber AL, Biton M, Vinarsky V, Lin B, Birket SE, Yuan F, Chen S, Leung HM, Villoria J, Rogel N, Burgin G, Tsankov AM, Waghray A, Slyper M, Waldman J, Nguyen L, Dionne D, Rozenblatt-Rosen O, Tata PR, Mou H, Shivaraju M, Bihler H, Mense M, Tearney GJ, Rowe SM, Engelhardt JF, Regev A, Rajagopal J (2018) A revised airway epithelial hierarchy includes CFTR-expressing ionocytes. Nature 560:319–324. https://doi.org/10.1038/s41586-018-0393-7
Manco R, Averbukh I, Porat Z, Bahar Halpern K, Amit I, Itzkovitz S (2021) Clump sequencing exposes the spatial expression programs of intestinal secretory cells. Nat Commun 12:3074. https://doi.org/10.1038/s41467-021-23245-2
Ushiama S, Ishimaru Y, Narukawa M, Yoshioka M, Kozuka C, Watanabe N, Tsunoda M, Osakabe N, Asakura T, Masuzaki H, Abe K (2016) Catecholamines facilitate fuel expenditure and protect against obesity via a novel network of the gut-brain axis in transcription factor Skn-1-deficient mice. EBioMedicine 8:60–71. https://doi.org/10.1016/j.ebiom.2016.04.031
Maizels RM, Bundy DA, Selkirk ME, Smith DF, Anderson RM (1993) Immunological modulation and evasion by helminth parasites in human populations. Nature 365:797–805. https://doi.org/10.1038/365797a0
Pei C, Zhao C, Wang AJ, Fan AX, Grinchuk V, Smith A, Sun R, Xie Y, Lu N, Urban JF Jr, Shea-Donohue T, Zhao A, Yang Z (2016) Critical role for interleukin-25 in host protective Th2 memory response against Heligmosomoides polygyrus bakeri. Infect Immun 84:3328–3337. https://doi.org/10.1128/IAI.00180-16
Brand JG, Cagan RH, Naim M (1982) Chemical senses in the release of gastric and pancreatic secretions. Annu Rev Nutr 2:249–276. https://doi.org/10.1146/annurev.nu.02.070182.001341
Peyrot des Gachons C, Beauchamp GK, Stern RM, Koch KL, Breslin PA (2011) Bitter taste induces nausea. Curr Biol 21:R247-248. https://doi.org/10.1016/j.cub.2011.02.028
Hoover B, Baena V, Kaelberer MM, Getaneh F, Chinchilla S, Bohorquez DV (2017) The intestinal tuft cell nanostructure in 3D. Sci Rep 7:1652. https://doi.org/10.1038/s41598-017-01520-x
Funding
Open Access funding provided by Universität Zürich. C.S. is supported by the Peter Hans Hofschneider Professorship for Molecular Medicine, an Eccellenza grant from the Swiss National Science Foundation (194216), the Foundation for Research in Science and the Humanities at the University of Zurich (STWF-20-007), and the Olga Mayenfisch Stiftung.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schneider, C. Tuft cell integration of luminal states and interaction modules in tissues. Pflugers Arch - Eur J Physiol 473, 1713–1722 (2021). https://doi.org/10.1007/s00424-021-02630-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-021-02630-2