Abstract
Purpose
Endometriosis involving the colon and/or rectum (CRE) is operatively managed using various methods. We aimed to determine if a more limited excision is associated with 30-day complications, symptom improvement, and/or recurrence.
Methods
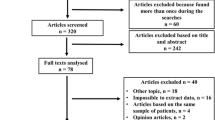
This is a retrospective review of consecutive cases of patients who underwent surgical management of CRE between 2010 and 2018. Primary outcomes were the associations between risk factors and symptom improvement, 30-day complications, and time to recurrence. Multivariable logistic regression assessed the independent risk factors.
Results
Of 2681 endometriosis cases, 142 [5.3% of total, mean age 35.4 (31.0; 39.0) years, 73.9% stage IV] underwent CRE excision (superficial partial = 66.9%, segmental = 27.5%, full thickness = 1.41%). Minor complications (14.8%) were associated with blood loss [150 (112; 288) vs. 100 (50.0; 200) mls, p = 0.046], Sigmoid involvement [45.5% vs. 12.2%, HR 5.89 (1.4; 22.5), p = 0.01], stoma formation [52.6% vs. 8.9%, HR 10.9 (3.65; 34.1), p < 0.001], and segmental resection [38.5% vs. 5.8%, HR 9.75 (3.54; 30.4), p < 0.001]. Superficial, partial-thickness resections were associated with decreased risk [(4.2% vs. 36.2%), HR 0.08 (0.02; 0.24), p < 0.001]. Factors associated with major complications (8.5%) were blood loss [250 (100; 400) vs. 100 (50.0; 200) mls, p = 0.03], open surgery [31.6% vs. 4.9%, HR 8.74 (2.36; 32.9), p = 0.001], stoma formation [42% vs. 3.3%, HR 20.3 (5.41; 90.0), p < 0.001], and segmental colectomy [28.2% vs. 0.9%, HR 34.6 (6.25; 876), p < 0.001]. Partial-thickness resection was associated with decreased risk ([.05% vs. 23.4%, HR 8.74 (2.36; 32.9), p < 0.001]. 19.1% experienced recurrence. Open surgery [5.2% vs. 21.3%, HR 0.14 (0.02; 1.05), p = 0.027] and superficial partial thickness excision [23.4% vs. 10.6%, HR 2.86 (1.08; 7.59), p = 0.027] were associated. Segmental resection was associated with decreased recurrence risk [7.6% vs. 23.5%, HR 0.27 (0.08; 0.91), p = 0.024].
Conclusion
Limiting resection to partial-thickness or full-thickness disc excision compared to bowel resection may improve complications but increase recurrence risk.


Similar content being viewed by others
References
Bong JW, Yu CS, Lee JL et al (2019) Intestinal endometriosis: diagnostic ambiguities and surgical outcomes. World J Clin Cases 7(4):441–451
Abrão MS, Petraglia F, Falcone T, Keckstein J, Osuga Y, Chapron C (2015) Deep endometriosis infiltrating the recto-sigmoid: critical factors to consider before management. Hum Reprod Update 21(3):329–339
Lincango EP, Connelly TM, Cheong JY, Kessler H (2022) An incidental infiltrating colonic lesion found during colonoscopy in a woman in her 30s [published online ahead of print, 2022 Oct 14]. ANZ J Surg. https://doi.org/10.1111/ans.18093
De Cicco C, Corona R, Schonman R, Mailova K, Ussia A, Koninckx P (2011) Bowel resection for deep endometriosis: a systematic review. BJOG. 118(3):285–291
Renner SP, Kessler H, Topal N et al (2017) Major and minor complications after anterior rectal resection for deeply infiltrating endometriosis. Arch Gynecol Obstet 295(5):1277–1285
Nezhat C, Li A, Falik R et al (2018) Bowel endometriosis: diagnosis and management. Am J Obstet Gynecol 218(6):549–562
Vermeulen N, Abrao MS, Einarsson JI et al (2021) Endometriosis classification, staging and reporting systems: a review on the road to a universally accepted endometriosis classification. J Minim Invasive Gynecol 28(11):1822–1848
Strasberg SM, Linehan DC, Hawkins WG (2009) The accordion severity grading system of surgical complications. Ann Surg 250(2):177–186
Messaris E, Sehgal R, Deiling S et al (2012 Feb) Dehydration is the most common indication for readmission after diverting ileostomy creation. Dis Colon Rectum 55(2):175–180
Roman H, Huet E, Bridoux V, Khalil H, Hennetier C, Bubenheim M, Braund S, Tuech JJ (2022 Jun) Long-term outcomes following surgical management of rectal endometriosis: seven-year follow-up of patients enrolled in a randomized trial. J Minim Invasive Gynecol 29(6):767–775
O'Brien L, Morarasu S, Morarasu BC et al (2023 Feb) Conservative surgery versus colorectal resection for endometriosis with rectal involvement: a systematic review and meta-analysis of surgical and long-term outcomes. Int J Color Dis 38(1):55
Mehedintu C, Frincu F, Brinduse LA et al (2021) Postoperative assessment of the quality of life in patients with colorectal endometriosis. J Clin Med 10(21)
Namazov A, Kathurusinghe S, Mehdi E et al (2022) Evolution of bowel complaints after laparoscopic endometriosis surgery: a 1497 women comparative study. J Minim Invasive Gynecol 29(4):499–506
Farella M, Tuech JJ, Bridoux V et al (2021) Surgical management by disk excision or rectal resection of low rectal endometriosis and risk of low anterior resection syndrome: a retrospective comparative study. J Minim Invasive Gynecol 28(12):2013–2024
Spagnolo E, Zannoni L, Raimondo D, Ferrini G, Mabrouk M, Benfenati A, Villa G, Bertoldo V, Seracchioli R (2014 Nov-Dec) Urodynamic evaluation and anorectal manometry pre- and post-operative bowel shaving surgical procedure for posterior deep infiltrating endometriosis: a pilot study. J Minim Invasive Gynecol 21(6):1080–1085
Author information
Authors and Affiliations
Contributions
All authors are responsible for the conceptualization, funding acquisition, investigation, methodology, project administration, supervision, validation, writing—original draft, and writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval
This project was granted ethical approval from the Cleveland Clinic IRB board.
Consent to participate
Due to the anonymized nature of patient data, consent was waived.
Conflict of interest
The authors declare no competing interests.
Additional information
An abstract from this manuscript was presented at the 2023 Annual Scientific Meeting ASCRS in Seattle, WA June 4, 2023.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The first two authors Abigail Christiansen and Tara M. Connelly are joint first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christiansen, A., Connelly, T.M., Lincango, E.P. et al. Endometriosis with colonic and rectal involvement: surgical approach and outcomes in 142 patients. Langenbecks Arch Surg 408, 385 (2023). https://doi.org/10.1007/s00423-023-03095-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03095-w