Abstract
Background and aim
Prognostic Nutritional Index (PNI) is a useful tool to predict short-term results in patients undergoing surgery for gastrointestinal cancer. Few studies have addressed this issue in colorectal cancer or specifically in rectal cancer. We evaluated the prognostic relevance of preoperative PNI on morbidity of patients undergoing laparoscopic curative resection for rectal cancer (LCRRC).
Methods
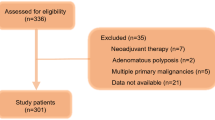
PNI data and clinico-pathological characteristics of LCRRC patients (June 2005–December 2020) were evaluated. Patients with metastatic disease were excluded. Postoperative complications were evaluated using the Clavien–Dindo classification.
Results
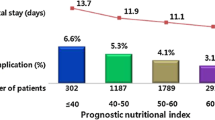
A total of 182 patients were included in the analysis. Median preoperative PNI was 36.5 (IQR 32.8–41.2). Lower PNI was associated with females (p=0.02), older patients (p=0.0002), comorbidity status (p<0.0001), and those who did not receive neoadjuvant treatment (p=0.01). Post-operative complications occurred in 53 patients (29.1%), by the Clavien–Dindo classification: 40 grades I–II and 13 grades III–V. Median preoperative PNI was 35.0 (31.8–40.0) in complicated patients and 37.0 (33.0–41.5) in uncomplicated patients (p=0.09). PNI showed poor discriminative performance regarding postoperative morbidity (AUC 0.57) and was not associated with postoperative morbidity (OR 0.97) at multivariable analysis.
Conclusions
Preoperative PNI was not associated with postoperative morbidity after LCRRC. Further research should focus on different nutritional indicators or hematological/immunological biomarkers.

Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71:209–249
Araghi M, Soerjomataram I, Jenkins M, Brierley J, Morris E, Bray F, Arnold M (2019) Global trends in colorectal cancer mortality: projections to the year 2035. Int J Cancer 144:2992–3000
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 69:613–616
Slaney G (1971) Results of treatment for carcinoma of the colon and rectum. Mod Trends Surg 3:69–89
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, Leer JW, van de Velde CJ (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646
Law WL, Choi HK, Lee YM (2007) Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11:8–15
Aritinian A, Orcutt TS, Anaya AD et al (2015) Infectious post-operative complications decrease long term survival in patients undergoing curative surgery for colorectal cancer. A study of 12,075 patients. Ann Surg 261:497–505
Filip B, Scarpa M, Cavallin F, Cagol M, Alfieri R, Saadeh L, Ancona E, Castoro C (2015) Postoperative outcome after oesophagectomy for cancer: nutritional index score is the missing ring in the current prognostic scores. Eur J Surg Oncol 41:787–794
Watanabe M, Iwatsuki M, Iwagami S, Ishimoto T, Baba Y, Baba H (2012) Prognostic Nutritional Index predicts outcomes of gastrectomy in the elderly. World J Surg 36:1632–1639
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A (2011) Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg 98:268–274
Pinato DJ, North BV, Sharma R (2012) A novel externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the Prognostic Nutritional Index (PNI). Br J Cancer 106:1439–1144
Tokunaga R, Sakamoto Y, Nakagawa S, Miyamoto Y, Yoshida N, Oki E, Watanabe M, Baba H (2015) Prognostic Nutritional Index predicts complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum 58:1048–1057
Jian-Hui C, Iskandar EA, Cai S, Chen C, Wu H, Xu J, He Y (2016) Significance of Onodera’s Prognostic Nutritional Index in patients with colorectal cancer: a large cohort study in a single Chinese institution. Tumor Biol 37:3277–3283
Mohri Y, Inohue Y, Tanaka K, Hiro J, Uchida K, Kusunoki M (2013) Prognostic Nutritional Index predicts postoperative outcome in colorectal cancer. World J Surg 37:2688–2692
Yang Y, Gao P, Chen X, Song Y, Shi J, Zhao J, Sun J, Xu Y, Wang Z (2016) Prognostic significance of preoperative Prognostic Nutritional Index in colorectal cancer: results from a retrospective cohort study and a meta-analysis. Oncotarget 7:58543–58552
Onodera T, Goseki N, Kosaki G (1984) Prognostic Nutritional Index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005
Miyakita H, Sadahiro S, Saito G, Okada K, Tanaka A, Suzuki T (2017) Risk scores as useful predictors of perioperative complications in patients with rectal cancer who received radical surgery. Int J Clin Oncol 22:324–331
Xia LJ, Li W, Zhai JC, Yan CW, Chen JB, Yang H (2020) Significance of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio and Prognostic Nutritional Index for predicting clinical outcomes in T1-2 rectal cancer. BMC Cancer 20:208
Al-Homoud S, Purkayastha S, Aziz O, Smith JJ, Thompson MD, Darzi AW, Stamatakis JD, Tekkis PP (2004) Evaluating operative risk in colorectal cancer surgery: ASA and POSSUM-based predictive models. Surg Oncol 13:83–92
Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
R Core Team (2022) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/. Accessed 31 Jan 2023
https://www.registrotumoriveneto.it/it/dati/dati-per-sede (accessed September 30, 2022)
Subwongcharoen S, Areesawangvong P, Chompoosaeng T (2019) Impact of nutritional status on surgical patients. Clin Nutr ESPEN 32:135–139
Li D, Jensen CC (2019) Patient satisfaction and quality of life with enhanced recovery protocols. Clin Colon Rectal Surg 32:138–144
Portale G, Spolverato Y, Bartolotta P, Gregori D, MAzzeo A, Rettore C, Cancian L, Fiscon V, (2023) Skeletal muscle mass and surgical morbidity after laparoscopic rectal cancer resection. J Laparoendosc Adv Surg Tech A 33(6):570–578. https://doi.org/10.1089/lap.2023.0068
Jochum SB, Kistner M, Wood EH et al (2019) Is sarcopenia a better predictor of complications than body mass index? Sarcopenia and surgical outcomes in patients with rectal cancer. Colorectal Dis 21:1372–1378
Uehara H, Yamazaki T, Kaneyama H et al (2022) Is radiological psoas muscle area measurement a predictor of postoperative complications after rectal resection for cancer? A retrospective study. Surg Today 52:306–315
Takeda Y, Akiyoshi T, Matsueda K et al (2018) Skeletal muscle loss is an independent negative prognostic factor in patients with advanced lower rectal cancer treated with neoadjuvant chemoradiotherapy. PLoS One 21:1372–1378
Chen XY, Yin SY, Shen YT, Zhang XC, Chen KK, Zhou CJ, Zheng CG (2022) The geriatric nutritional risk index is an effective tool to detect GLIM-defined malnutrition in rectal cancer patients. Front Nutr 15(9):1061944
Bausys A, Kryzauskas M, Abeciunas V, Degutyte AE, Bausys R, Strupas K, Poskus T (2022) Prehabilitation in modern colorectal cancer surgery: a comprehensive review. Cancers 13(14):5017
Franssen RF, Bongers BC, Vongelaar FJ, Janssen-Heijnen ML (2022) Feasibility of a tele-prehabilitation program in high-risk patients with colon or rectal cancer undergoing elective surgery: a feasibility study. Perioper Med 26(11):28
Author information
Authors and Affiliations
Contributions
Giuseppe Portale, Matteo Zuin, and Diletta Di Miceli conceptualized the study and prepared the first draft of the manuscript. Ylenia Spolverato and Chiara Cipollari retrieved the data. Francesco Cavallin performed the data analysis. Alberto Morabito, Teodoro Sava, and Valentino Fiscon participated in the analysis and contributed to editing the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOC 39 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Portale, G., Cavallin, F., Cipollari, C. et al. Preoperative Prognostic Nutritional Index was not predictive of short-term complications after laparoscopic resection for rectal cancer. Langenbecks Arch Surg 408, 263 (2023). https://doi.org/10.1007/s00423-023-02962-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02962-w