Abstract
Background
No randomised clinical trials (RCTs) have simultaneously compared the safety of open (OA), transperitoneal laparoscopic (TLA), posterior retroperitoneal (PRA), and robotic adrenalectomy (RA) for resecting adrenal tumours.
Aim
To evaluate outcomes for OA, TLA, PRA, and RA from RCTs.
Methods
A NMA was performed according to PRISMA-NMA guidelines. Analysis was performed using R packages and Shiny.
Results
Eight RCTs with 488 patients were included (mean age: 48.9 years). Overall, 44.5% of patients underwent TLA (217/488), 37.3% underwent PRA (182/488), 16.4% underwent RA (80/488), and just 1.8% patients underwent OA (9/488). The mean tumour size was 35 mm in largest diameter with mean sizes of 44.3 mm for RA, 40.9 mm for OA, 35.5 mm for TLA, and 34.4 mm for PRA (P < 0.001). TLA had the lowest blood loss (mean: 50.6 ml), complication rates (12.4%, 14/113), and conversion to open rates (1.3%, 2/157), while PRA had the shortest intra-operative duration (mean: 94 min), length of hospital stay (mean: 3.7 days), lowest visual analogue scale pain scores post-operatively (mean: 3.7), and was most cost-effective (mean: 1728 euros per case). At NMA, there was a significant increase in blood loss for OA (mean difference (MD): 117.00 ml (95% confidence interval (CI): 1.41–230.00)) with similar blood loss observed for PRA (MD: − 10.50 (95% CI: − 83.40–65.90)) compared to TLA.
Conclusion
LTA and PRA are important contemporary options in achieving favourable outcomes following adrenalectomy. The next generation of RCTs may be more insightful for comparison surgical outcomes following RA, as this approach is likely to play a future role in minimally invasive adrenalectomy.
PROSPERO registration
CRD42022301005.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While tumours of the adrenal glands were traditionally resected through open adrenalectomy (OA) [1], the contemporary approach to adrenal lesions has evolved to minimally invasive techniques (both transperitoneal laparoscopic and more recently retroperitoneoscopic), replacing traditional open resections [2, 3]. In recent times, the surgical approach has further evolved with the adoption of robotic technology as the next iteration of minimally invasive surgery (MIS). MIS was originally pioneered in colorectal surgery and the evolution of its use has extended to endocrine surgery, such that minimally invasive adrenalectomy is now considered the gold standard for resecting most lesions of the adrenal gland [4,5,6,7,8]. Laparoscopic adrenalectomy was first described by Gagner et al. [9] and Higashihara et al. [10] in 1992, which involved a transperitoneal laparoscopic approach to adrenalectomy (TLA), before Walz et al. described a posterior retroperitoneal approach to resecting the adrenal gland (PRA) [11]. While the European Society of Endocrine Surgeons (ESES) continues to recommend OA for the resection of adrenocortical carcinoma (ACC) and cancers of 8 cm or greater in size [12], performing laparoscopic adrenalectomy is considered advantageous over OA if possible, due to a reported reduction in post-operative pain, major morbidity, length of hospital stay (LOS), surgical site infection, and faster recovery time [13]. Notwithstanding, performing laparoscopic adrenalectomy does confer unavoidable limitations: the operating surgeon has limited instrument movement/dexterity compared to OA and the natural physiological hand tremor becomes amplified at laparoscopy. Furthermore, the two-dimensional projection of images through the camera limits the view of the surgical field in its entirety [14, 15]. In addition, laparoscopic approaches become challenging in complex patients, including those with large tumours, with phaeochromocytomas, and in those with increased body habitus. In such complex cases, conversion from laparoscopic to OA typically occurs in approximately 3–5% of cases [16, 17]. As described, the ESES guidelines further reflect the importance of OA in specific circumstances, as this approach remains the gold standard for resections of ACC and large tumours (8 cm in size or greater) [12].
Robotic surgery first made its debut as a technique for performing adrenalectomy in 2002 [18]. Robotic technology is an attractive addition to the surgeon’s armamentarium with theoretical advantages over conventional laparoscopic techniques such as improved dexterity (including more flexible and intuitive instrument control), a wristed instrument to eliminate physiological tremor, and a three-dimensional visual field which is non-inferior to laparoscopy [19, 20]. Shortcomings of robotic adrenalectomy (RA) are the longer operative time, increased expenses associated with purchasing and maintaining equipment and training operators, a steep learning curve, and poorer cost-effectiveness in low-volume centres [21,22,23,24].
Previous meta-analyses have addressed the oncological and surgical safety of RA compared to laparoscopic adrenalectomy [25,26,27], while others have evaluated the utility of both TLA and PRA over OA in achieving safe and effective resection of lesions of the adrenal glands [13, 28,29,30]. While these meta-analyses compare the outcomes for two approaches to adrenalectomy using studies of retrospective design, there are no previous meta-analyses performed evaluating the safety of RCTs comparing the safety of all four approaches to adrenalectomy. Therefore, applying network meta-analysis (NMA) methodology is advantageous if employed here as it facilitates simultaneous comparison of OA, TLA, PRA, and RA [31, 32]. Accordingly, the aim of the current systematic review and network meta-analysis of randomised clinical trials (RCTs) was to evaluate the post-operative surgical and oncological outcomes of OA, TLA, PRA, and RA.
Methods
A systematic review was performed in accordance with the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (or PRISMA) extension statement for reporting of systematic reviews incorporating network meta-analyses of healthcare interventions [33]. Local institutional ethical approval was not required as all data used in this analysis was obtained from a previously published resource. This study was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO): CRD42022301005.
Study eligibility
For inclusion in this analysis, studies had to meet the following inclusion criteria: (1) prospective randomised trials (i.e. RCTs) which compared any peri-operative implications and complication rates following different approaches to adrenalectomy (i.e. any post-operative complications; intra-operative blood loss; duration of the operation; conversion to open adrenalectomy; post-operative pain at 12 h post-operatively (D0), 24 h post-operatively (D1), and 48 h post-operatively (D2); cost of procedure; and length of stay (LOS)), irrespective of clinical, radiological, or oncological indication for surgery, (2) studies had to provide full-text manuscripts, and (3) be published in the past 20 years (2001–2021). Included studies were expected to report patient demographics and to report on the primary outcomes of interest. Studies failing to meet these strict eligibility criteria were not considered for inclusion. Conference abstracts and studies not published in the English language were excluded.
Population, Intervention, Comparison, Outcomes (PICO)
Using the PICO framework [34], the aspects the authors wished to address were:
-
Population — Patients aged 18 years or older who were due to undergo adrenalectomy for any indication.
-
Intervention — Any patient eligible for and then randomised to undergo a minimally invasive approach to adrenalectomy (i.e. TLA or PRA) for resection of pathologies of the adrenal gland.
-
Comparison — Any patient who are eligible and randomised to undergo any of the other approaches (including other minimally invasive/laparoscopic approaches) to adrenalectomy for resection of the same pathologies of the adrenal gland.
-
Outcomes
-
The primary outcomes of interest were:
-
Rates of specific complications experienced post-operatively including surgical site infections (SSIs), pneumothoraces, and haematoma.
-
Timing/duration of operation, defined as the time taken in minutes from opening skin to skin closure.
-
Intra-operative blood loss, reported in millilitres.
-
Rates of conversion to open adrenalectomy following initial attempt to perform the other approaches to adrenalectomy.
-
The secondary outcomes of interest were:
-
Post-operative pain reported using visual analogue scales (VAS) at 12 h post-operatively (D0), 24 h post-operatively (D2), and 48 h post-operatively (D2).
-
Cost of each approach to adrenalectomy (in euros). In cases where cost was provided in another currency, local conversion rates were applied for comparability.
-
LOS post-operatively reported in days.
-
Recurrence following adrenalectomy — this included oncological, biochemical, or physiological recurrences
Search strategy
A formal systematic search was performed on the 23rd of December 2021 of the PUBMED, EMBASE, and Cochrane Central Register of Controlled Trials (CENTRAL) electronic databases. Each database was initially searched for relevant titles. This search was performed by two independent reviewers, using a predetermined search strategy that was designed by the senior authors. This search included the following search term: (Adrenalectomy[MeSH Terms]. Boolean operators were not deployed for this search. Manual cross-referencing of reference lists from previous systematic reviews, meta-analyses, and included trials was undertaken. As described, studies were limited to those published in the period 2001–2021.
Manual removal of duplicate studies was performed before all titles were screened. Thereafter, RCTs considered to be appropriate had their abstracts and/or full text reviewed. Retrieved studies were reviewed to ensure inclusion criteria were met for the primary outcome at a minimum, with discordances in opinion resolved through consultation with the third author (NED). Data extraction was also performed by two independent reviewers (MGD & ÉJR), with study details, basic patient clinicopathological characteristics, and surgical data all recorded. The final search was performed in January 2022.
Data management and analysis
Descriptive statistics were used to outline and report characteristics of included trials. Rates of complications and conversion to open adrenalectomy rates were expressed as dichotomous or binary outcomes, reported as odds ratios (ORs) expressed with 95% confidence intervals (CIs). ORs were calculated, using crude event RCT data, to compare interventions using per-protocol data, where applicable. Comparative operation times, intra-operative blood loss, VAS pain, etc. were calculated using mean values, standard deviations (SD), and pooled mean variance. The mean difference (MD) between approaches to adrenalectomy was then calculated at NMA. The principal comparator varied in several of these analyses based on the approaches to adrenalectomy compared for each primary outcome measure. Cost analyses of each approach to adrenalectomy were performed for the adrenalectomy operation and not for entire length of hospital stay. Analyses were performed to facilitate US Dollars (USD) conversion to euros at a rate of 1.00 USD = 0.88 euro [35] and one-way analysis of variance analyses (or ANOVA, †) were performed to compare mean costs of each procedure. All surgical costs are reported in euro. Disease recurrence was defined as ‘invasive disease recurrence of the primary adrenal malignancy for which the patient underwent the surgical resection with adrenalectomy (which subsequently was evaluated in an RCT)’.
Bayesian network meta-analyses were conducted using Netameta and Shiny packages for R [23]. Effect sizes were described with a 95% CI. Results were considered statistically significant at the P < 0.050 level if the 95% CI did not include the value of one. Estimates of mean and SDs were calculated using standard statistical methods, where applicable [36, 37]. Rank probabilities were plotted against the possible ranks for all competing treatments. The deviance from unrelated mean effect inconsistency models was used to establish the inconsistency of each analysis performed. Rankings were illustrated using Litmus rank-o-gram surface under the cumulative ranking curve (SUCRA) analyses, with directionality imposed upon outcome measures by author to provide clinical relevance to results. The confidence in estimates of the outcome was assessed using ‘Confidence in Network Meta-Analysis’ (CINeMA) [38]. Methodological assessment of included studies was undertaken using the Cochrane Risk of Bias assessment tool [39]. Quality assessment of included studies was conducted assessed using the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) assessment [40].
Results
Literature search and study characteristics
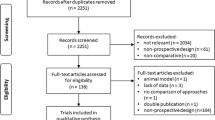
The systematic search strategy identified a total of 17,017 studies, of which 1877 duplicate studies were manually removed. The remaining 15,140 studies had their titles and/or abstracts screened for relevance, before 15 full texts were reviewed. In total, 8 RCTs fulfilled our inclusion criteria and were included in this systematic review and network meta-analysis [41,42,43,44,45,46,47,48] (Fig. 1). Publication dates ranged from 2004 to 2019 (Table 1). The mean follow up was 33.6 months.
Clinicopathological and surgical data
In total, there was data included from 488 patients with mean age at diagnosis of 48.9 years (range 19–84 years — 8 studies) [41,42,43,44,45,46,47,48]. Overall, 55.9% of patients were female (273/488 — 8 studies) [41,42,43,44,45,46,47,48]. The mean body mass index of included patients was 26.1 (range: 19–35 — 7 studies) [41,42,43,44,45,46,47]. In total, 46.1% of patients underwent resection of phaeochromocytomas (225/488), 26.2% underwent resection of a non-functioning adrenal tumour (128/488), 16.8% underwent resection of an aldosteronoma (82/488), 9.6% underwent resection of a glucocorticoid secreting adrenal adenoma (47/488), and just 6 patients underwent resection of an isolated metastatic deposit or other tumours (including 3 cases of ACC) (1.2%).
Overall, 44.5% of patients underwent TLA (217/488), 37.3% underwent PRA (182/488), 16.4% underwent RA (80/488), and 1.8% patients underwent OA (9/488) (Table 1). More patients underwent left sided adrenalectomy than right sided adrenalectomy (left: 59.8%, 262/458 vs. right: 40.2%, 196/458 — 8 RCTs) [41,42,43,44,45,46,47,48].
The mean size of resected tumours was 35 mm in largest diameter (range: 8–65 mm — 8 studies) [41,42,43,44,45,46,47,48], which was significantly greater for RA compared to laparoscopic approaches (i.e. TLA and PRA): The mean tumour size resected was 44.3 mm for RA, 40.9 mm for OA, 35.5 mm for TLA, and 34.4 mm for PRA (P < 0.001, †). Clinical data and indications for adrenalectomy from the 8 included RCTs are provided in detail in Table 2.
Duration of operation
All 8 RCTs reported on the operative duration of adrenalectomy [41,42,43,44,45,46,47,48]. The shortest operation mean duration for adrenalectomy was for PRA (93.7 min, range: 30–180 min). Conversely, the longest operation duration was OA with a mean of 180.0 min (range: 120–230 min) (Supplementary Material S1). At network meta-analysis, there was no significant difference in operative time reported for OA (MD: − 21.50 (95% CI: − 22.60–66.10)) or PRA (MD: 7.82 (95% CI: − 21.20–36.70)) compared to TLA (2 RCTs) (Supplementary Material 2A). The associated ranking tables for these approaches to adrenalectomy and operative duration are outlined in Table 3A.
Intra-operative blood loss
In total, 7 RCTs reported on intra-operative blood loss during adrenalectomy [41,42,43,44,45, 47, 48]. Patients undergoing OA had the largest intra-operative blood loss at surgery (mean: 164 ml), while those undergoing TLA had the smallest intra-operative blood loss (mean: 50.6 ml, range: 25–200mls) (Supplementary Material S1). At network meta-analysis, there was a significant increase in intra-operative blood loss for those undergoing OA (MD: 117.00 (95% CI: 1.41–230.00)) with similar blood loss observed for those undergoing PRA (MD: − 10.50 (95% CI: − 83.40–65.90)) compared to TLA (3 RCTs) (Supplementary Material 2B). The associated ranking tables for these approaches to adrenalectomy and blood loss are outlined in Table 3B.
Overall complications
The overall complication rate following adrenalectomy was 12.9% (38/294) from the 4 RCTs included which reported complication rates [43, 44, 46, 47]. RA had the highest complication rates (13.8%, 11/80) and TLA had the lowest complication rates (12.4%, 14/113) (Supplementary Material S3). Unfortunately, specific complications reported by the RCTs included in this study were incompatible with independent NMA.
At NMA for overall complications, there was no significant difference reported for RA (OR: 1.130 (95% CI: 0.404–3.000)) or PRA (OR: 0.657 (95% CI: 0.195–2.200)) compared to TLA (4 RCTs) (Supplementary Material 2C). The associated ranking tables for these approaches to adrenalectomy and post-operative complications are outlined in Table 3C.
Of note, post-operative pneumonia (n = 8) and requiring blood transfusions (n = 6) were the commonest complications reported post-adrenalectomy, with no studies reporting data on incisional hernia. The breakdown of the reported complications is outlined in Supplementary Material S4.
Conversion to open
In total, 6 RCTs reported on converting to open during adrenalectomy [41, 43,44,45,46,47]. The overall conversion rate was 2.3% (9/383). RA had the highest conversion to open rates (5.0%, 4/80), compared to PRA (2.1%, 3/146) and TLA (1.3%, 2/157) (Supplementary Material S3). At network meta-analysis, there was no significant difference observed for RA (OR: 7.91 (95% CI: 0.167–396.000)) or PRA (OR: 3.92 (95% CI: 0.231–126.000)) compared to TLA (4 RCTs) (Supplementary Material 2D). Indications for converting to open included right adrenal vein haemorrhage [42] and failure to progress during MIS approach [45, 47]. Ranking tables for minimally invasive approaches to adrenalectomy and conversion to open are outlined in Table 3D.
Post-operative pain
Overall, 4 RCTs reported post-operative VAS pain scores [41,42,43, 45] and just RCT reported post-operative pain complicating the procedure as a dichotomous outcome (Supplementary Material S4) [43]. TLA was higher than PRA at D0 post-operatively (mean VAS: 4.4 vs. 3.7), D1 post-operatively (mean VAS: 3.0 vs. 2.1), and D2 post-operatively (mean VAS: 2.5 vs. 1.7) (Supplementary Material S5). At network meta-analysis, there was no significant difference in pain at D0 post-operatively reported for PRA (MD: − 0.423 (95% CI: − 1.350–0.580)) compared to TLA (2 RCTs) (Supplementary Material 2E). Ranking tables for these approaches to adrenalectomy and post-operative pain are outlined in Table 3E.
Length of hospital stay
Overall, 7 RCTs reported LOS following adrenalectomy [41,42,43,44,45,46, 48]. OA had the longest LOS (mean: 8.0 days), compared to RA (mean: 4.4 days), TLA (mean: 3.6 days), and PRA (mean: 2.1 days) (Supplementary Material S5). At network meta-analysis, there was no significant reduction observed for LOS following PRA (MD: − 0.178 (95% CI: − 0.476–0.149)) compared to TLA (2 RCTs) (Supplementary Material 2F). Ranking tables for these approaches to adrenalectomy and length of hospital stay are outlined in Table 3F. Ranking figures illustrating the most favourable approach for relevant outcome measures are illustrated in Fig. 2. Network plots illustrating the number of RCTs included for the meta-analysis performed for the previous 6 outcome measures are outlined in Supplementary Material S6.
Disease recurrence
In total, 4 RCTs reported disease recurrence following adrenalectomy [42, 43, 47, 48] and there was just 1 recurrence observed in the patients included (0.4%, 1/239). This recurrence occurred in patient undergoing PRA in the trial performed by Rubenstein et al. (0.8%, 1/117) [47]. Details surrounding this recurrence are not provided in this study (i.e. oncological, biochemical, or physiological recurrence). No patients who underwent OA (0.0%, 0/9) or TLA (0.0%, 0/113) suffered disease recurrence (Supplementary Material S3).
Cost of adrenalectomy
Overall, 3 RCTs reported cost relating to approach to adrenalectomy [41, 44, 46]. Of these, Ma et al. report cost for full hospitalisation for adrenalectomy [44], which was not included in our analysis. Morino et al. and Barczynski et al. report costs of performing an adrenalectomy and were included in this analysis [41, 46]. The overall mean cost of performing an adrenalectomy was 2729.50 euros. Overall, RA was the most expensive approach to adrenalectomy (RA: 3050 euros vs. TLA: 2362 euros vs. PRA: 1728 euros, P < 0.001, †) (Supplementary Material S5).
Risk of bias assessment
The majority of included RCTs had low-to-moderate risk of bias: Overall, 2 of the included RCTs had low-risk of bias (25.0%) [41, 47], 4 of the RCTs included some concerns for bias (50.0%) [42,43,44, 48], while 2 RCTs were considered high-risk of bias (25.0%) [45, 46]. Risk of bias assessment is summarised in Table 1. Quality assessment of included studies was conducted assessed using the GRADE assessments (Supplementary Material S7). Deviance from unrelated mean effect inconsistency models is outlined in Supplementary Material S8. Rankings illustrated using Litmus rank-o-gram surface under the cumulative ranking curve (SUCRA) analyses are depicted in Supplementary Material S9.
Discussion
This study is the first systematic review and NMA to integrate data from prospective, randomised clinical trials to evaluate post-operative surgical outcomes following different approaches to adrenalectomy for adrenal lesions suitable for a minimally invasive approach. In total, eight RCTs were included and the raw data demonstrated that there were favourable intra-operative and post-operative outcomes reported for those who underwent TLA and PRA approaches compared to those undergoing OA and RA, despite the indications being similar irrespective of approach used. At NMA, most analyses failed to illustrate significant differences between approaches to adrenalectomy, except for the data illustrating increased blood loss following OA relative to other approaches. Importantly, the size of the tumours resected in each of the included studies was similar for those undergoing OA and other approaches, with none of the adrenalectomies be performed for large, locally advanced, or ACC (except for 3 ACCs resected in the study by Rubenstein — 2/25 from the TLA group and 1/32 from the PRA group). In addition, just Ma et al. and Rubenstein et al. compared approaches for resecting both benign and invasive cancers of the adrenal glands, with just 10.5% (6/57) of cases included by Rubenstein et al. being for malignant pathologies, with no differentiation among pathologies being reported by Ma et al. Therefore, the results of this study highlight the significance of adopting minimally invasive techniques for small, non-ACC-related lesions of the adrenal gland where feasible, when surgical resection is indicated.
In this analysis, TLA and PRA exhibited favourable outcomes with respect to intra-operative duration, blood loss, and post-operative complications compared to patients undergoing OA or RA, while demonstrating lower conversion to open rates for these MIS approaches compared to RA. The most informative results are derived from the crude values reported for each approach to adrenalectomy at systematic review, as the majority of these analyses failed to demonstrate statistical significance at meta-analysis. A plausible explanation for these finding is that NMA calculations may be underpowered due to a lack of data availability for certain outcome measures (e.g. all 8 RCTs report intra-operative duration, yet just 2 of these provide data for integration into meta-analysis). While the NMA element to this study may be scrutinised for being performed prematurely, the systematic review component of this study provides insightful ‘real-world’ data in relation to intra- and post-operative surgical outcomes following adrenalectomy.
Unsurprisingly, patients undergoing OA experienced significantly more intra-operative blood loss compared to their counterparts who underwent minimally invasive adrenalectomy. This is a predictable finding, and one that supports the use of MIS techniques when resecting non-malignant adrenal cancer pathologies, as recommended by the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines [49]. In addition to the data highlighting reduced blood loss associated with minimally invasive adrenalectomy techniques, MIS is perceived to be advantageous as patients are subject to less physiological stress, immunologic burden, faster recovery times, lower complication rates, and less use of healthcare resources [50,51,52]. Accordingly, this study further emphasises and validates the current paradigm shift towards adopting MIS techniques where clinically appropriate and possible, reserving OA for larger, locally advanced cases and ACCs, where laparoscopic or robotic surgery may prove futile in achieving a complete R0 resection [12, 53]. Notwithstanding, acknowledgement must be made for the likelihood that this indication for OA may confound the results implying that OA has longer operative time and blood loss relative to minimally invasive approaches to the adrenal gland.
Overall, TLA had the lowest intra-operative blood loss (mean: 51 millilitres per operation), conversion to open rates (1.3%, 14/113), and complication rates (12.4%, 14/113) when compared to other approaches to adrenalectomy. TLA is advantageous as it facilitates the surgeon to work with typically familiar intra-bdominal anatomy and in a wider working space than PRA [54], while making use of what the majority of surgeons would consider more familiar instrumentation than robotic instruments [55]. In addition, TLA is associated with reduced complication rates than is observed in patients who have undergone OA [28, 56]. When considering these factors, this RCT data illustrating the benefit of TLA approach may be unsurprising; however, several of these outcomes are comparable for PRA: We observed a minimal difference in intra-operative blood loss for TLA and PRA (mean: 51 ml vs. 55 millilitres per operation), which is unlikely to be clinically relevant and PRA had the shortest intra-operative duration, length of hospital stay, and lowest post-operative pain. As such, when MIS is indicated, PRA may be considered once surgical and institutional expertise allows, as previously demonstrated by Nigri et al. in their meta-analysis [29, 57]. Thus, this study supports the use of minimally invasive laparoscopic/retroperitoneoscopic approaches to adrenalectomy where indicated, with reservation of the OA approach for cases where minimally invasive approaches are deemed be unlikely to effectively resect the tumour to establish oncological control, for example, for large (> 8 cm), locally advanced tumours, those extending into major venous structures, or those of ACC pathology [22, 53].
While there are several potential advantages of adopting the RA approach compared to other minimally invasive approaches (TLA/RPA) [14, 15, 58], the results of the current meta-analysis do not support the adoption of RA as routine at present. There are several reasons for such results: In this analysis, two RCTs compared RA and minimally invasive techniques [44, 46]: Morino et al. conducted the first RCT comparing RA and MIS techniques, which provided very disappointing results, with 40.0% of the RA group requiring conversion to open surgery to successfully resect the adrenal gland [46]. Subsequently, Ma et al. performed a second RCT with more promising results regarding the use of RA (less patients converted to open (0/70 vs. 1/70 for LA) and reduced mean intra-operative time (92.5 min vs. 122.5 min for LA) [44], which has been supported by several recent observational studies [59, 60]. Furthermore, there were only 80 patients who underwent RA in this analysis which may bring into question the robustness of these results. At the time of writing, these early RCTs are approaching 20 years since publication, and it is likely that robotic techniques have become optimised as the learning curve is negated in recent years. Therefore, once this steep learning curve effect associated with RA is overcome [61], the timing may be appropriate to conduct large, prospective multicentre RCTs which may prove insightful as to whether RA or the other minimally invasive approaches (TLA/PRA) best serve patients by improving surgical outcomes following adrenalectomy. In particular, surgeons would be likely have to developed a certain degree of familiarity with the static camera vision, motion scaling, and tremor elimination offered by robotic surgery [62], while allowing time for the reported disadvantages such as increased costs, longer operative times, and loss of haptic feedback [63, 64] to be offset as the learning curve is surmounted [65].
As previously described, there are no previous reports of prospective, randomised trials comparing the safety of all four approaches to adrenalectomy. Thus, the authors deployed NMA methodology to evaluate the previously published RCTs to establish the surgical and oncological safety profiles of each of approach to adrenalectomy. Heger et al. previously performed a NMA of both randomised and non-randomised clinical trials evaluating outcomes following open and MIS approaches to adrenalectomy [29]. Results from the current study are congruent with the work of Heger et al., illustrating the advantages of MIS in reducing intra-operative blood loss, post-operative complications, and LOS following adrenalectomy. Conversely, Heger et al. report OA as the fastest technique, directly contradicting the results of the current analysis. It is of interest to note that there have been several previous meta-analyses demonstrating comparable outcomes for RA and other minimally invasive approaches: Brandao et al. performed a meta-analysis of observational studies including 600 patients which demonstrated comparable surgical outcomes for RA and minimally invasive adrenalectomy [27]. Similarly, Economopoulos et al. illustrated the safety of RA relative to laparoscopic adrenalectomy in their extensive meta-analysis performed involving 1162 patients from 27 studies [26]. As techniques in robotic endocrine surgery become more commonly used, these previous meta-analyses support robust adoption of RA where feasible, yet the current study successfully challenges this work from these previous authors using RCT data. As previously outlined, the modest outcomes observed in our study in relation to RA suggest there remains a steep learning curve for RA adoption as ‘gold standard’ [61]. Additionally, there are several meta-analyses which compare surgical outcomes for OA and minimally invasive techniques [13, 28, 30, 66]: Sgourakis et al. previously reported similar surgical and post-operative outcomes for those undergoing OA and MIS for stage I/II adrenocortical carcinoma, with poorer 5-year survival outcomes observed for those undergoing minimally invasive techniques [30]. In their recent meta-analysis of 14 studies and 743 patients, Li et al. outlined minimally invasive adrenalectomy as a more feasible and safer treatment option to OA, with reduced post-operative morbidity and improved recovery outcomes observed following MIS in those undergoing resection of phaeochromocytoma [28]. Similarly, Fu et al. confirmed the efficacy of MIS for phaeochromocytoma surgery in their recent meta-analysis [13]. While this study focuses on studies of the highest level of evidence to definitively establish the optimal approach to adrenalectomy, Perivoliotis et al. performed a previous analysis of 2997 patients (from 21 studies of moderate-to-high quality evidence — 1 RCT and 20 non-randomised studies) which ultimately favoured RA as the optimal approach to adrenalectomy [66].
Limitations
Despite several strengths, the current study is subject to several inherent limitations. Firstly, as previously outlined, several outcome measures used in our NMA may be underpowered relative to the robust availability of crude data reported at systematic review, limiting the robustness of NMA results. Secondly, the year of publication of RCTs was intentionally limited to those published in the past 20 years (2001–2021) to ensure the modern adrenal surgery paradigm was within the data used for this analysis. Although this was performed pragmatically by the authors, it is possible remains that some RCTs may have not been captured in this search. Thirdly, with just 9 patients undergoing OA in the current analysis, it is obvious that this analysis is not powered to provide many meaningful comparisons between OA and other approaches to adrenalectomy. Therefore, caution must be taken when interpreting results described in relation to this method of adrenalectomy. Finally, in the wake of the era of robotic endocrine surgery, we must re-emphasise the steep learning curve associated with RA. As robotic surgical techniques become optimised, future RCTs will likely provide more insightful and exciting results in relation to robotic approaches to the adrenal gland, as we strive towards an era of minimally invasive, personalised oncological care.
In conclusion, the current systematic review and NMA of RCTs highlights the value of adopting laparoscopic approaches in achieving favourable surgical and oncological outcomes following adrenalectomy. While outcomes post-OA are inferior relative to minimally invasive adrenalectomy, judicious case selection is warranted to determine which cases would benefit from open approaches in the era of minimally invasive surgery. While the results of this study fail to support RA as routine, the learning curve associated with RA may have impacted the results and this approach is likely to play a role in future MIS of the adrenal gland. Therefore, contemporary RA warrants robust investigation in well-designed designed RCTs to determine its position in the multimodal management paradigm of pathologies of the adrenal gland.
References
Harris DA, Wheeler MH (2005) History of adrenal surgery. In: Linos D, van Heerden JA (eds) Adrenal glands: diagnostic aspects and surgical therapy. Springer, Berlin Heidelberg p, Berlin, Heidelberg, pp 1–6
Matsuda T (2017) Laparoscopic adrenalectomy: the ‘gold standard’ when performed appropriately. BJU Int 119(1):2–3
Carr AA, Wang TS (2016) Minimally invasive adrenalectomy. Surg Oncol Clin N Am 25(1):139–152
Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059. https://doi.org/10.1056/NEJMoa032651
Buunen M et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10(1):44–52
Bessoff KE et al (2021) Evidence-based surgery for laparoscopic appendectomy: a stepwise systematic review. Surg Open Sci 6:29–39
Klarenbeek BR et al (2009) Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma Trial. Ann Surg 249(1):39–44
Gervaz P et al (2010) A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg 252(1):3–8
Gagner M, Lacroix A, Bolté E (1992) Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N Engl J Med 327(14):1033
Higashihara E et al (1992) A case report of laparoscopic adrenalectomy. Nihon Hinyokika Gakkai Zasshi 83(7):1130–1133
Walz MK et al (1995) Dorsal retroperitoneoscopic adrenalectomy–a new surgical technique. Zentralbl Chir 120(1):53–58
Gaujoux S et al (2017) European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg 104(4):358–376
Fu S-Q et al (2020) Laparoscopic versus open surgery for pheochromocytoma: a meta-analysis. BMC Surg 20(1):167–167
Agrusa A et al (2016) Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: a case-control study. Int J Surg 28(Suppl 1):S114–S117
Agrusa A et al (2018) 3D laparoscopic surgery: a prospective clinical trial. Oncotarget 9(25):17325–17333
Shen WT et al (2004) Reasons for conversion from laparoscopic to open or hand-assisted adrenalectomy: review of 261 laparoscopic adrenalectomies from 1993 to 2003. World J Surg 28(11):1176–1179
Shen ZJ et al (2007) Predictive factors for open conversion of laparoscopic adrenalectomy: a 13-year review of 456 cases. J Endourol 21(11):1333–1337
Desai MM et al (2002) Robotic-assisted laparoscopic adrenalectomy. Urology 60(6):1104–1107
Woo Y et al (2011) Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg 146(9):1086–1092
Van Koughnett JA et al (2009) Are there advantages to robotic-assisted surgery over laparoscopy from the surgeon’s perspective? J Robot Surg 3(2):79–82
Nomine-Criqui C et al (2017) Robot-assisted adrenalectomy: indications and drawbacks. Updates Surg 69(2):127–133
Pineda-Solís K, Medina-Franco H, Heslin MJ (2013) Robotic versus laparoscopic adrenalectomy: a comparative study in a high-volume center. Surg Endosc 27(2):599–602
Owen RK et al (2019) MetaInsight: an interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res Synth Methods 10(4):569–581
Hyams ES et al (2013) Impact of robotic technique and surgical volume on the cost of radical prostatectomy. J Endourol 27(3):298–303
Tang K et al (2015) Robot-assisted versus laparoscopic adrenalectomy: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 25(3):187–195
Economopoulos KP et al (2017) Laparoscopic versus robotic adrenalectomy: a comprehensive meta-analysis. Int J Surg 38:95–104
Brandao LF et al (2014) Robotic versus laparoscopic adrenalectomy: a systematic review and meta-analysis. Eur Urol 65(6):1154–1161
Li J et al (2020) Laparoscopic adrenalectomy (LA) vs open adrenalectomy (OA) for pheochromocytoma (PHEO): a systematic review and meta-analysis. Eur J Surg Oncol 46(6):991–998
Heger P et al (2017) Evaluation of open and minimally invasive adrenalectomy: a systematic review and network meta-analysis. World J Surg 41(11):2746–2757
Sgourakis G et al (2015) Laparoscopic versus open adrenalectomy for stage I/II adrenocortical carcinoma: meta-analysis of outcomes. J Invest Surg 28(3):145–152
Jansen JP, Naci H (2013) Is network meta-analysis as valid as standard pairwise meta-analysis? It all depends on the distribution of effect modifiers. BMC Med 11(1):159
Mills EJ, Thorlund K, Ioannidis JP (2013) Demystifying trial networks and network meta-analysis. BMJ 346:f2914
Hutton B et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Armstrong EC (1999) The well-built clinical question: the key to finding the best evidence efficiently. WMJ 98(2):25–28
USD-EUR X-RATE (2021) Cited 2021 28th December 2021. Available from: https://www.bloomberg.com/quote/USDEUR:CUR
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Luo D et al (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805
Wan X et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135
Higgins JPT et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Yepes-Nuñez JJ et al (2019) Development of the summary of findings table for network meta-analysis. J Clin Epidemiol 115:1–13
Barczyński M, Konturek A, Nowak W (2014) Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg 260(5):740–7 (discussion 747-8)
Chai YJ et al (2019) Lateral transperitoneal adrenalectomy versus posterior retroperitoneoscopic adrenalectomy for benign adrenal gland disease: randomized controlled trial at a single tertiary medical center. Ann Surg 269(5):842–848
Kozłowski T et al (2019) Laparoscopic adrenalectomy: lateral transperitoneal versus posterior retroperitoneal approach - prospective randomized trial. Wideochir Inne Tech Maloinwazyjne. 14(2):160–169
Ma W et al (2020) Surgical outcomes of a randomized controlled trial compared robotic versus laparoscopic adrenalectomy for pheochromocytoma. Eur J Surg Oncol 46(10 Pt A):1843–1847
Mohammadi-Fallah MR et al (2013) Comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy in a prospective randomized study. J Laparoendosc Adv Surg Tech A 23(4):362–366
Morino M et al (2004) Robot-assisted vs laparoscopic adrenalectomy: a prospective randomized controlled trial. Surg Endosc 18(12):1742–1746
Rubinstein M et al (2005) Prospective, randomized comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy. J Urol 174(2):442–5 (discussion 445)
Tiberio GA et al (2008) Prospective randomized comparison of laparoscopic versus open adrenalectomy for sporadic pheochromocytoma. Surg Endosc 22(6):1435–1439
Stefanidis D et al (2013) SAGES guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc 27(11):3960–3980
Cooper MA et al (2014) Hospital level under-utilization of minimally invasive surgery in the United States: retrospective review. BMJ 349:g4198
da Luz Moreira A et al (2010) Laparoscopic versus open colectomy for patients with American Society of Anesthesiology (ASA) classifications 3 and 4: the minimally invasive approach is associated with significantly quicker recovery and reduced costs. Surg Endosc 24(6):1280–1286
Novitsky YW, Litwin DE, Callery MP (2004) The net immunologic advantage of laparoscopic surgery. Surg Endosc 18(10):1411–1419
Mihai R (2019) Open adrenalectomy. Gland Surg 8(Suppl 1):S28-s35
Shiraishi K et al (2019) Transperitoneal versus retroperitoneal laparoscopic adrenalectomy for large pheochromocytoma: comparative outcomes. Int J Urol 26(2):212–216
Grogan RH (2020) Current status of robotic adrenalectomy in the United States. Gland Surg 9(3):840–843
Fan CJ et al (2018) Minimally invasive versus open surgery in the Medicare population: a comparison of post-operative and economic outcomes. Surg Endosc 32(9):3874–3880
Nigri G et al (2013) Meta-analysis of trials comparing laparoscopic transperitoneal and retroperitoneal adrenalectomy. Surgery 153(1):111–119
Dickson PV et al (2013) Robotic-assisted retroperitoneoscopic adrenalectomy: making a good procedure even better. Am Surg 79(1):84–89
Mishra K et al (2019) Comparative efficacy of laparoscopic versus robotic adrenalectomy for adrenal malignancy. Urology 123:146–150
Hue JJ et al (2021) A comparison of robotic and laparoscopic minimally invasive adrenalectomy for adrenal malignancies. Surg Endosc 36(7):5374–5381
Mazzon G et al (2017) Learning curves for robotic surgery: a review of the recent literature. Curr Urol Rep 18(11):89
Orosco RK et al (2021) Compensatory motion scaling for time-delayed robotic surgery. Surg Endosc 35(6):2613–2618
Okamura AM (2009) Haptic feedback in robot-assisted minimally invasive surgery. Curr Opin Urol 19(1):102–107
Ahmadi N, Mor I, Warner R (2022) Comparison of outcome and costs of robotic and laparoscopic right hemicolectomies. J Robot Surg 16(2):429–436
Soomro NA et al (2020) Systematic review of learning curves in robot-assisted surgery. BJS Open 4(1):27–44
Perivoliotis K et al (2020) Comparing the efficacy and safety of laparoscopic and robotic adrenalectomy: a meta-analysis and trial sequential analysis. Langenbeck’s Arch Surg 405(2):125–135
Funding
Open Access funding provided by the IReL Consortium M.G.D received funding from the National Breast Cancer Research Institute, Ireland.
Author information
Authors and Affiliations
Contributions
M.G.D., E.J.R, and N.E.D. conceived the presented idea. A.J.L and M.J.K developed the theory and performed the computations. M.G.D and E.J.R performed the systemic search and M.R.B arbitrated discrepancies in opinion. M.G.D and E.J.R performed data extraction which was subsequently checked by M.A. and N.E.D. M.G.D. and E.J.R. performed statistical analyses and M.A. and O.K.R. verified these analytical methods. M.G.D. drafted the original manuscript which was supervised by A.J.L and M.J.K. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Manuscript category: Original Research — This manuscript is not based on a communication to a society or meeting.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Davey, M.G., Ryan, É.J., Donlon, N.E. et al. Comparing surgical outcomes of approaches to adrenalectomy — a systematic review and network meta-analysis of randomised clinical trials. Langenbecks Arch Surg 408, 180 (2023). https://doi.org/10.1007/s00423-023-02911-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02911-7