Abstract
Purpose
Laparoscopic ileal pouch-anal anastomosis (IPAA) surgery offers improved short-term outcomes over open surgery but can be technically challenging. Robotic surgery has been increasingly used for IPAA surgery, but there is limited evidence supporting its use. This study aims to compare the short-term outcomes of laparoscopic and robotic IPAA procedures.
Methods
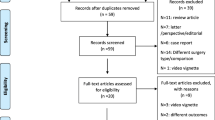
All consecutive patients receiving laparoscopic and robotic IPAA surgery at 3 centres, from 3 countries, between 2008 and 2019 were identified from prospectively collated databases. Robotic surgery patients were propensity score matched with laparoscopic patients for gender, previous abdominal surgery, ASA grade (I, II vs III, IV) and procedure performed (proctocolectomy vs completion proctectomy). Their short-term outcomes were examined.
Results
A total of 89 patients were identified (73 laparoscopic, 16 robotic). The 16 patients that received robotic surgery were matched with 15 laparoscopic patients. Baseline characteristics were similar between the two groups. There were no statistically significant differences in any of the investigated short-term outcomes. Length of stay trend was higher for laparoscopic surgery (9 vs 7 days, p = 0.072)
Conclusion
Robotic IPAA surgery is safe and feasible and offers similar short-term outcomes to laparoscopic surgery. Length of stay may be lower for robotic IPAA surgery, but further larger scale studies are required in order to demonstrate this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the main surgical treatment for patients with ulcerative colitis (UC) and familiar adenomatous polyposis (FAP), offering the benefit of avoiding a permanent stoma [1, 2]. However, there is a suggestion that in England the number of pouch procedures may be decreasing [3], possibly due to the associated problems of poor pouch function many patients experience.
Laparoscopic surgery has been increasingly utilised for pouch surgery [4] with a Cochrane review published in 2009 [5] and a randomised control trial in 2013 [6] supporting its feasibility and safety. Since then, there has been evidence demonstrating better cosmesis [6], improved fertility [7], lower blood loss [8], quicker recovery of bowel function [8] and faster recovery [9] with laparoscopic procedures when compared to open IPAA surgery. Nevertheless, the limitations of laparoscopic instruments make pelvic dissection and the proctectomy segment of the operation rather challenging. In England between 2012 and 2016, 60% of pouch surgery was still conducted through an open approach [3], and in the LapConPouch trial [6], a laparoscopic vs open pouch surgery trial, the conversion rate in the laparoscopic arm was 23.8%, possibly accounting for the reason why the number of pouch procedures in England has decreased. Alternative methods such as taTME have been described [10, 11], but the anatomy of performing the proctectomy from ‘back to front’ presents its own challenges. Robotic surgery addresses the limitations of laparoscopic instruments and is performed with the same anatomical approach as open and laparoscopic surgery. It is well established as an alternative method of operating for rectal cancer, with large multinational case series published in the literature [12, 13]. However, there are only a handful of small-scale studies for robotic vs laparoscopic IPAA surgery [14,15,16,17,18]. These studies are summarised in two recently published systematic reviews [19, 20], which conclude that more data is required.
This study aims to add to the current body of evidence comparing laparoscopic and robotic IPAA surgery and support its safety and feasibility.
Materials and methods
A retrospective analysis of prospectively maintained databases was conducted for this study. Consecutive patients from 3 centres, for 3 different countries (England, Portugal and Qatar), who received elective minimally invasive proctocolectomies or completion proctectomies with IPAA reconstruction between 2008 and 2019 were identified and included in this study. The common denominator is that all cases were performed or supervised by a single surgeon with extensive experience in both laparoscopic and robotic colorectal surgery. The robotic cases were propensity score matched to laparoscopic cases to obtain comparable cohorts.
Patients were prepared for surgery according to each regional institutions policy. Patients with UC, FAP and confirmed colorectal adenocarcinoma (either on a background of UC or FAP) were included. The decision as to whether to perform the procedure laparoscopically or robotically depended on availability of the robotic platform, which was the preferred approach when available. Surgical dissection was similar for both laparoscopic and robotic procedures with a standardised fully robotic technique applied for all robotic surgeries as taught in the European Academy of Robotic Colorectal Surgery (EARCS) programme [12]. A fully robotic approach was applied in both the proctocolectomies and completion proctectomies. Dissection was completed by means of minimally invasive surgery, with an extraction site used for specimen delivery and pouch formation. The requirements for anonymisation of personal dataset by the Data Protection Act 1998 were satisfied. According to the Health Research Authority (HRA), this study did not require their approval due to its status as a clinical audit.
Surgical procedure
Robot-assisted IPAA
Two stage proctocolectomy and ileoanal pouch
All procedures were performed using 4th generation da Vinci Xi platform by Intuitive Surgical™. Three 8 mm and one 12 mm robotic ports were used for the surgery. Additional two assistant ports were also used to complete the procedure (Fig. 1). Extraction site for retrieval of specimen was made with 5 cm supra pubic incision. After creation of ileoanal stapled J pouch, protective loop ileostomy was created at the right iliac fossa.
Following insertion of ports and creation of pneumo-peritoneum, dissection starts at the sacral promontory with isolation, ligation and division of inferior mesenteric artery (IMA) and inferior mesenteric vein (IMV). Rectal mobilisation is performed in the TME plane protecting the hypogastric nerve plexus. The rectal tube is divided just above the anal canal at 4–5 cm from the anal verge using da Vinci 45 or 60 mm green load stapler.
Dissection continues with the mobilisation of the splenic flexure and left transverse colon. At this stage, robotic boom is rotated to perform right colonic mobilisation; the ileocolic artery and vein, right colonic vessels and middle colic artery branches are isolated, ligated and divided to complete the mobilisation of right and transverse colon. The specimen is delivered with 4–5 cm incision at the supra pubic area using Alexis wound protector.
Following the delivery of the whole specimen, a standard 18–20 cm stapled ileoanal J pouch is fashioned extracorporeally. Ileoanal anastomosis is performed using a 28-mm CEA circular stapler under the view. Flexible endoscopy is performed to check for leak test and integrity of the pouch. RIF protective ileostomy is performed at the previously marked right iliac fossa site.
The temporary ileostomy was closed if water soluble contrast enema performed at 2 months did not show anastomotic leakage or stenosis. Through incision in the right iliac fossa, side to side anastomosis was performed using a linear stapler [Covidien or Ethicon Inc., NJ, USA]. The wound was partially closed according to purse-string closure or simple closure according to the surgeon preferences.
Ileoanal pouch formation in patients with previous subtotal colectomy
Robotic port placement is standardised for the performance of proctectomy and ileoanal pouch formation in patients who had undergone previous emergency subtotal colectomy.
Following the creation of pneumo-peritoneum, the rectal stump is identified and mobilised in the TME planes down to the pelvic floor. Care is taken to identify and protect the hypogastric nerve plexus. The rectal tube is divided just above the sphincters using 45–60-mm green load da Vinci stapler. Specimen is extracted through the suprapubic 5 cm incision using Alexis wound protector.
Previously created ileostomy is mobilised, and standard 18–20 cm stapled J pouch is fashioned extracorporeally. Ileoanal pouch anastomosis is performed using a 28-mm circular stapler with protective loop ileostomy created at the same site of the right iliac fossa.
Data collection and outcome assessment
The baseline characteristics and short-term surgical outcomes of patients receiving elective laparoscopic and robotic IPAA surgery were analysed. Baseline characteristics analysed included diagnosis, age, BMI, gender, American Society of Anaesthesiologist (ASA) grade, operation performed and previous abdominal surgery. Perioperative data included operative time, estimated blood loss (EBL) and conversion to open (defined as any incision needed to either mobilise the colon or rectum or ligate the vessels). Post-operative clinical data examined included length of stay (LOS), 30-day readmission, 30-day reoperation, Clavien-Dindo complication ≥ 3 and 30-day mortality.
Statistical analysis
Once collated, cleaned and checked, the data was analysed using IBM SPSS version 26 (SPSS Inc., Chicago, IL, USA). The robotic cases were propensity score matched (PSM) to laparoscopic cases. The variables used to calculate the propensity score matching (PSM) were as follows: gender, previous abdominal surgery, ASA grade (I, II vs III, IV) and procedure performed (proctocolectomy vs completion proctectomy). PSM variable selection was based on what the authors believed to be of most clinical significance. Propensity scores were calculated via logistic regression analysis by applying the Propensity Score Matching function on SPSS version 26 with the match tolerance set to 0.
Non-parametric data was expressed as median with interquartile range and parametric data as mean with standard deviation. Baseline and clinical characteristics were compared using χ2 test or Fisher’s exact test for categorical variables, Mann-Whitney U test for non-parametric continuous variables and t test for parametric continuous variables. P values of < 0.05 were considered statistically significant.
Finally, univariate binary logistic regression analysis was performed on all patients receiving elective minimally invasive IPAA surgery to assess whether surgical approach (robotic or laparoscopic) affected morbidity (defined as the presence of any of the following outcomes: 30-day reoperation, Clavien-Dindo complication ≥ 3, 30-day readmission, LOS > 14 days). Following this, a multivariate model was applied where surgical approach was adjusted for all clinically relevant variables including age, gender, BMI, ASA grade (I–II vs III–IV), previous abdominal surgery and procedure performed. The constant was included in the analysis model and data is presented as odds ratio, 95% confidence interval and p value.
Results
A total of 89 patients were identified (73 laparoscopic, 16 robotic) whose data was included in this study. The 16 robotic cases were propensity score matched with 15 laparoscopic cases to reduce the effect of confounding factors.
Baseline characteristics
There were no differences in any of the baseline characteristics between the two groups as demonstrated in Table 1. PSM produced near perfect matches for gender, previous abdominal surgery, ASA grade and procedure performed. Proctocolectomies accounted for 5 (33.3%) and 5 (31.3%) of the laparoscopic and robotic IPAA procedures respectively, while UC was the primary diagnosis for the majority of cases in both groups (lap: 13 (86.7%), rob: 14 (87.5%)).
Short-term outcomes
The short-term outcomes of the two groups are summarised in Table 2. There was only one conversion and this was in the laparoscopic group (p = 0.484). There was no 30-day mortality in either group. The short-term outcomes were largely similar and there was no statistically significant difference in any of the investigated short-term outcomes between the two cohorts. Length of stay trend was lower in the robotic group but did not reach statistical significance (7 vs 9 days, p = 0.072).
There was one reoperation in the laparoscopic group, which was a laparoscopic washout due to a collection. There were four readmissions in the laparoscopic group and three in the robotic group. All readmissions were due to either high stoma output or abdominal pain, with one patient having a wound infection. The only Clavien-Dindo complication ≥ 3 was the reoperation discussed.
Logistic regression analysis
Univariate logistic regression analysis of all 89 cases showed that surgical approach did not affect morbidity for the participants in this study. This was still the case in multivariate analysis when other clinically relevant factors were adjusted for (age, gender, BMI, ASA grade (I–II vs III–IV), previous abdominal surgery and procedure performed). Table 3 summarises the described findings.
Discussion
In contrast to robotic surgery for colorectal cancer, there is very limited evidence investigating the clinical outcomes of robotic pouch surgery. In our study, we demonstrate that robotic IPAA surgery is safe and feasible with comparable short-term clinical outcomes to that of laparoscopic surgery. In addition, in the examined cohort, there was a trend towards a reduced length of stay in the robotic group, which is in agreement with other previous studies comparing robotic to laparoscopic IPAA surgery [17, 18].
The robotic platform offers a stable 3-D high-definition camera and wristed instruments with 7 degrees of freedom. The proctectomy part of pouch surgery can be technically challenging, and the adjuncts of robotic surgery are ideally suited for it. Its application in rectal cancer surgery is spreading in accelerated pace [12], and a handful of small volume studies have been published comparing robotic vs laparoscopic pouch surgery [14,15,16,17,18], summarised in a systematic review by Flynn et al. [19]. The number of robotic pouch procedures in these studies ranges between 16 and 74 cases. Our series is equally low in volume but offers the advantage of a comparison between equally matched cohorts as well as performing a logistic regression analysis of all available data to investigate the effect of robotic procedures on morbidity. As discussed by Flynn et al. [19], the main limitations of the available literature are the heterogeneity of the data and quality of the reported studies. Two of the five studies have only been published as conference abstracts [16, 18], offering only limited information on the study design. Some of the studies included cases where a completion proctectomy and end ileostomy was performed rather than an IPAA, and in other studies, there are significant differences between the two cohorts in terms of diagnosis (UC vs FAP) and procedures (proctocolectomy vs completion proctectomy) performed [19]. These differences potentially skew the outcomes of the reported studies. Moreover, in the reported literature, there is considerable variation on how the colectomy segment of the robotic proctocolectomies was performed, which could have been performed laparoscopically (hybrid approach), lap assisted or robotically (total robotic) [19]. In our study, all robotic cases were totally robotic, and no hybrid cases were done; this approach reduces cost since it avoids opening two sets of instruments and utilises the benefits of the robotic platform for the whole procedure.
In our study population, operation time was similar in the two groups. This is contrast to other studies that have shown larger operation times for the robotic cohort [14,15,16,17,18]. We speculate that this is because all procedures were performed or supervised by a surgeon with vast experience in robotic surgery that has fully overcome his learning curve [21]. Even though it was initially accepted that operation times were longer with robotic when compared to laparoscopic colorectal surgery, more recent studies have demonstrated similar operation times between robotic and laparoscopic rectal surgery [22,23,24,25], and some have even shown shorter operation times in the robotic cohorts [26,27,28,29]. This is potentially due to the improvements of the latest robotic systems (X and Xi), which limit arm clashing and reduce docking time [30]. Additionally, as surgeons overcome their learning curve in robotic surgery, they become faster and in difficult cases can even reduce their operative time when compared to laparoscopy by utilising the advantages the robotic platform has to offer [31]. Furthermore, the presented studies LOS is comparable to that of the literature (rob vs lap: 7 vs 9 days), with Rencuzogullari et al. [15] and Marino et al. [16] demonstrating similar LOS in both cohorts (rob vs lap: 7.8 vs 9 [15]; 8.7 vs 9.2 [16] days).
In our study, median LOS was shorter in the robotic cohort, although it was not statistically significant (7 vs 9 days, p = 0.072). Considering the small sample size, there is a realistic chance that there is a type 2 error and that robotic pouch surgery can indeed help reduce LOS. This is supported by Lightner et al. [17] and Elias et al. [18], with both studies reporting improved LOS in their robotic arms [17, 18]. The reason behind this might be that robotic surgery can enable more precise surgery in the pelvis, resulting in less tissue trauma, fewer complications and consequently a lower LOS.
Conversion rate, 30-day readmission, 30-day reoperation, Clavien-Dindo ≥ 3 complications and EBL were similar in the two cohorts. Furthermore, univariate and multivariate logistic regression showed that surgical approach (robotic or laparoscopic) was not found to affect morbidity. This is similar to the previous studies that also did not report any major differences in these outcomes between the two approaches [19].
The main strengths of our study lie on the standardisation of operative approach between all robotic and laparoscopic cases [12] and the fact that data was collected from multiple centres from different countries therefore increasing its external validity. Furthermore, due to the PSM, the two cohorts were evenly matched in terms of baseline characteristics, limiting the effect of cofounding factors.
Acknowledging its limitations, our study is a retrospective analysis, it is of small sample size and almost all of the laparoscopic procedures pre-dated the robotic ones. The fact that all laparoscopic studies pre-dated the robotic cases can act as a potential cofounder. However, it should be noted that this could confound the results either way. Although theoretically any improvements in the robotic cohort could be attributed to the increasing experience of the lead surgeon or improvements in the unit, the robotic cohort is much smaller and therefore it could be argued these are cases early on the learning curve. Another point worth mentioning is the fact that all cases were done or closely supervised by a very experienced in both laparoscopic and robotic surgery colorectal surgeon offers the advantage of standardisation of treatment but can reduce the external validity of the results. Furthermore, the small sample size of the study increases the chance of type 2 error, although, with the exception of operation time, the results are very similar. One way to reduce the risk of type 2 error would be to perform 1:2 or 1:3 propensity score matching. However, considering the number of laparoscopic cases to choose from is also relatively low (n = 73), this would compromise the matching process and result in less evenly balanced cohorts. The main drawback of this study is the lack of functional data (urological, sexual and pouch function), lack of patient reported outcomes, lack of fertility data and lack of long-term pouch data such as pouch failure rates or pouchitis. Additionally, estimated blood loss was not compared as it is generally poorly recorded and hence a poor indicator for assessing quality of surgery. It could be that the technical advantages the robotic system has to offer are more likely to lead in differences on those outcomes rather the short-term outcomes examined in this study. This is because the precision in dissection offered in robotic surgery could lead to better preservation of the pelvic nerves (leading to improved functional outcomes) and reduce trauma in the pelvis, thus reducing sub-clinical leaks or pelvic sepsis that, even though do not necessarily affect short-term outcomes, can have a detrimental effect on long-term pouch outcomes.
In summary, our study supports the feasibility and safety of robotic pouch surgery and contributes to the current body of evidence comparing robotic and laparoscopic IPAA surgery. Further larger scale studies are required comparing those two techniques in order to be able to produce more meaningful meta-analyses. Finally, it is important to collect functional, fertility and long-term pouch function data since these outcomes are important to patients and the robotic platform is more likely to make a difference in these outcomes.
References
Parks AG, Nicholls RJ (1978) Proctocolectomy without ileostomy for ulcerative colitis. Br Med J 2:85–88. https://doi.org/10.1136/bmj.2.6130.85
Fazio VW, Ziv Y, Church JM et al (1995) Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 222:120–127. https://doi.org/10.1097/00000658-199508000-00003
Fearnhead NS, Lee MJ, Acheson AG et al (2018) Variation in practice of pouch surgery in England - using SWORD data to cut to the chase and justify centralization. Color Dis Off J Assoc Coloproctology Gt Britain Irel 20:597–605. https://doi.org/10.1111/codi.14036
Germain A, de Buck van Overstraeten A, Wolthuis A et al (2018) Outcome of restorative proctocolectomy with an ileo-anal pouch for ulcerative colitis: effect of changes in clinical practice. Color Dis Off J Assoc Coloproctology Gt Britain Irel 20:O30–O38. https://doi.org/10.1111/codi.13948
Ahmed Ali U, Keus F, Heikens JT et al (2009) Open versus laparoscopic (assisted) ileo pouch anal anastomosis for ulcerative colitis and familial adenomatous polyposis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006267.pub2
Schiessling S, Leowardi C, Kienle P et al (2013) Laparoscopic versus conventional ileoanal pouch procedure in patients undergoing elective restorative proctocolectomy (LapConPouch Trial)-a randomized controlled trial. Langenbeck’s Arch Surg 398:807–816. https://doi.org/10.1007/s00423-013-1088-z
Bartels SAL, DʼHoore A, Cuesta MA et al (2012) Significantly increased pregnancy rates after laparoscopic restorative proctocolectomy: a cross-sectional study. Ann Surg 256:1045–1048. https://doi.org/10.1097/SLA.0b013e318250caa9
Nozawa H, Hata K, Sasaki K et al (2022) Laparoscopic vs open restorative proctectomy after total abdominal colectomy for ulcerative colitis or familial adenomatous polyposis. Langenbeck’s Arch Surg 407(4):1605. https://doi.org/10.1007/s00423-022-02492-x
Singh P, Bhangu A, Nicholls RJ, Tekkis P (2013) A systematic review and meta-analysis of laparoscopic vs open restorative proctocolectomy. Color Dis Off J Assoc Coloproctology Gt Britain Irel 15:e340–e351. https://doi.org/10.1111/codi.12231
Coffey JC, Dillon MF, O’Driscoll JS, Faul E (2016) Transanal total mesocolic excision (taTME) as part of ileoanal pouch formation in ulcerative colitis--first report of a case. Int J Colorectal Dis 31:735–736. https://doi.org/10.1007/s00384-015-2236-4
Leo CA, Samaranayake S, Perry-Woodford ZL et al (2016) Initial experience of restorative proctocolectomy for ulcerative colitis by transanal total mesorectal rectal excision and single-incision abdominal laparoscopic surgery. Color Dis Off J Assoc Coloproctology Gt Britain Irel 18:1162–1166. https://doi.org/10.1111/codi.13359
Panteleimonitis S, Miskovic D, Bissett-Amess R et al (2020) Short-term clinical outcomes of a European training programme for robotic colorectal surgery. Surg Endosc 35:6796. https://doi.org/10.1007/s00464-020-08184-1
Feng Q, Yuan W, Li T et al (2022) Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): short-term outcomes of a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol 7(11):991. https://doi.org/10.1016/S2468-1253(22)00248-5
Miller AT, Berian JR, Rubin M et al (2012) Robotic-assisted proctectomy for inflammatory bowel disease: a case-matched comparison of laparoscopic and robotic technique. J Gastrointest Surg 16:587–594. https://doi.org/10.1007/s11605-011-1692-6
Rencuzogullari A, Gorgun E, Costedio M et al (2016) Case-matched comparison of robotic versus laparoscopic proctectomy for inflammatory bowel disease. Surg Laparosc Endosc Percutan Tech 26:e37–e40. https://doi.org/10.1097/SLE.0000000000000269
Marino MV, Glagoleva A (2018) Robotic-assisted vs. laparoscopic proctectomy for inflammatory bowel disease: results of the case-match comparison in single institution. J Crohns Colitis 12:S322–S322
Lightner AL, Grass F, McKenna NP et al (2019) Short-term postoperative outcomes following robotic versus laparoscopic ileal pouch-anal anastomosis are equivalent. Tech Coloproctol 23:259–266. https://doi.org/10.1007/s10151-019-01953-8
Elias AW, Landmann RG (2019) Tu1676–chasing zero cuff: robotic distal dissection superior to laparoscopy in ileal pouch anal anastomosis. Gastroenterology 156:1496
Flynn J, Larach JT, Kong JCH et al (2021) Robotic versus laparoscopic ileal pouch-anal anastomosis (IPAA): a systematic review and meta-analysis. Int J Colorectal Dis 36:1345–1356. https://doi.org/10.1007/s00384-021-03868-z
Khawaja Z, Jamal Z, Zafar N et al (2022) Role of robotic approach in ileal pouch-anal anastomosis (IPAA): a systematic review of the literature. J Robot Surg 16:1–7. https://doi.org/10.1007/s11701-022-01490-x
Odermatt M, Ahmed J, Panteleimonitis S et al (2017) Prior experience in laparoscopic rectal surgery can minimise the learning curve for robotic rectal resections: a cumulative sum analysis. Surg Endosc 31:4067. https://doi.org/10.1007/s00464-017-5453-9
Xiong B, Ma L, Huang W et al (2015) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a meta-analysis of eight studies. J Gastrointest Surg 19:516–526. https://doi.org/10.1007/s11605-014-2697-8
Trastulli S, Farinella E, Cirocchi R et al (2012) Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Color Dis 14:e134–e156. https://doi.org/10.1111/j.1463-1318.2011.02907.x
D’Annibale A, Pernazza G, Monsellato I et al (2013) Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc 27:1887–1895. https://doi.org/10.1007/s00464-012-2731-4
Park EJ, Cho MS, Baek SJ et al (2015) Long-term oncologic outcomes of robotic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg 261:129–137. https://doi.org/10.1097/SLA.0000000000000613
Baek J-H, Pastor C, Pigazzi A (2011) Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc 25:521–525. https://doi.org/10.1007/s00464-010-1204-x
Kwak JM, Kim SH (2016) Robotic surgery for rectal cancer: an update in 2015. Cancer Res Treat 48:427–435. https://doi.org/10.4143/crt.2015.478
Allemann P, Duvoisin C, Di Mare L et al (2016) Robotic-assisted surgery improves the quality of total mesorectal excision for rectal cancer compared to laparoscopy: results of a case-controlled analysis. World J Surg 40:1010–1016. https://doi.org/10.1007/s00268-015-3303-2
Levic K, Donatsky AM, Bulut O, Rosenberg J (2015) A comparative study of single-port laparoscopic surgery versus robotic-assisted laparoscopic surgery for rectal cancer. Surg Innov 22:368–375. https://doi.org/10.1177/1553350614556367
Panteleimonitis S, Pickering O, Ahmad M et al (2019) Robotic rectal cancer surgery: results from a European multicentre case series of 240 resections and comparative analysis between cases performed with the da Vinci Si and Xi systems. Laparosc Endosc Robot Surg 3(1):6–11. https://doi.org/10.1016/J.LERS.2019.12.002
Ahmed J, Cao H, Panteleimonitis S et al (2017) Robotic versus laparoscopic rectal surgery in high-risk patients. Colorectal Dis 19(12):1092. https://doi.org/10.1111/codi.13783
Funding
Open Access funding provided by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
Sofoklis Panteleimonitis: analysis and interpretation of data, drafting of manuscript. Mahmood Al-Dhaheri: acquisition of data, drafting of manuscript. Mick Harper: critical revision of manuscript. Ibrahim Amer: acquisition of data. Ayman Abdul Hafiz: critical revision of manuscript. Mohamed Abu Nada: critical revision of manuscript. Amjad Parvaiz: study conception and design, critical revision of manuscript
Corresponding author
Ethics declarations
Informed consent
Informed verbal consent was obtained from all individual participants included in the study.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Competing interests
Sofoklis Panteleimonitis, Mahmood Al-Dhaheri, Mick Harper, Ibrahim Amer, Ayman Abdul Hafiz, Mohamed Abu Nada and Amjad Parvaiz declare no competing interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Panteleimonitis, S., Al-Dhaheri, M., Harper, M. et al. Short-term outcomes in robotic vs laparoscopic ileal pouch-anal anastomosis surgery: a propensity score match study. Langenbecks Arch Surg 408, 175 (2023). https://doi.org/10.1007/s00423-023-02898-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02898-1