Abstract
Purpose
Even though minor, stoma-related complications significantly impact quality of life, they are often excluded from clinical analyses that compare short-term postoperative outcomes of loop ileostomy and loop colostomy. This study compares stoma-related complications between loop ileostomy and loop colostomy after rectal resection, including minor complications, and discusses the characteristics of diverting stoma types.
Methods
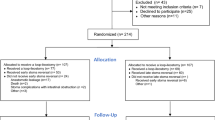
A retrospective review was conducted in patients who underwent diverting stoma construction after rectal resection. Data on patient background and postoperative short-term outcomes, including stoma-related complications and morbidity after stoma closure, were collected and compared between loop ileostomy and loop colostomy groups. Morbidities of all severity grades were targeted for analysis.
Results
A total of 47 patients (27 loop ileostomy, 20 loop colostomy) underwent diverting stoma construction following rectal resection. Overall stoma-related complications, incidence of skin irritation, high-output stoma, and outlet obstruction were significantly higher in the loop ileostomy group but high-output stoma and outlet obstruction were absent in the loop colostomy group. Regarding morbidity after stoma closure, operation times and surgical site infections were significantly higher in the loop colostomy group while anastomotic leakage after diverting stoma closure occurred (2 cases; 15%) in the loop colostomy group but not the loop ileostomy group.
Conclusion
Because stoma-related complications were significantly higher in the loop ileostomy group, and even these minor complications may impair QOL, early loop ileostomy closure is recommended. For loop colostomy, stoma-related morbidities are lower but post-closure leakage is a calculated risk.

Similar content being viewed by others
References
Kang CY et al (2013) Risk factors for anastomotic leakage after anterior resection for rectal cancer. JAMA Surg 148:65–71. https://doi.org/10.1001/2013.jamasurg.2
Eriksen MT et al (2005) Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis 7:51–57. https://doi.org/10.1111/j.1463-1318.2004.00700.x
Matthiessen P et al (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Colorectal Dis 6:462–469. https://doi.org/10.1111/j.1463-1318.2004.00657.x
Kruschewski M et al (2007) Risk factors for clinical anastomotic leakage and postoperative mortality in elective surgery for rectal cancer. Int J Colorectal Dis 22:919–927. https://doi.org/10.1007/s00384-006-0260-0
Matthiessen P et al (2007) Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer A randomized multicenter trial. Ann Surg 246:207–214. https://doi.org/10.1097/SLA.0b013e3180603024
Van der Pas MH et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218. https://doi.org/10.1016/S1470-2045(13)70016-0
Nugent KP et al (1999) Quality of life in stoma patients. Dis Colon Rectum 42:1569–1574. https://doi.org/10.1007/BF02236209
Danielsen AK et al (2017) Early Closure of a Temporary Ileostomy in Patients With Rectal Cancer A Multicenter Randomized Controlled Trial. Ann Surg 265:284–290. https://doi.org/10.1097/SLA.0000000000001829
Rui D et al (2021) Postoperative morbidity and mortality after anterior resection with preventive diverting loop ileostomy versus loop colostomy for rectal cancer: A updated systematic review and meta-analysis. Eur J Surg Oncol 47:1514–1525. https://doi.org/10.1016/j.ejso.2021.01.030
Tilney HS et al (2007) Comparison of Outcomes following ileostomy versus colostomy for defunctioning colorectal anastomosis. World J Surg 31:1142–1151. https://doi.org/10.1007/s00268-006-0218-y
Lyon C et al (2000) The spectrum of skin disorders in abdominal stoma patients. Br J Dermatol 143:1248–1260. https://doi.org/10.1046/j.1365-2133.2000.03896.x
Chudner A et al (2019) The influence of diverting loop ileostomy vs. colostomy on postoperative morbidity in restorative anterior resection for rectal cancer: a systematic review and meta-analysis. Langenbecks Arch Surg 404:129–139. https://doi.org/10.1007/s00423-019-01758-1
Rullier E et al (2001) Loop Ileostomy versus Loop Colostomy for Defunctioning Low Anastomoses during Rectal Cancer Surgery. World J Surg 25:274–278. https://doi.org/10.1007/s002680020091
Dimitrios P et al (2020) Loop ileostomy versus loop colostomy as temporary deviation after anterior resection for rectal cancer. Langenbecks Arch Surg 405:1147–1153. https://doi.org/10.1007/s00423-020-01940-w
American Society of Anesthesiologists (1963) New classification of physical status. Anesthesiology 24:111
Khoury GA et al (1986) Colostomy or ileostomy after colorectal anastomosis?: a randomized trial. Ann R Coll Surg Engl 68:5–7
Raimes SA, Mathew VV, Devlin HB et al (1984) Temporary loop ileostomy. J R Soc Med 77:738–741. https://doi.org/10.1177/014107688407700905
Alexander-Williams J et al (1974) Loop ileostomy and colostomy for faecal diversion. Ann R Coll Surg Engl 54:141–148
Rondelli F et al (2009) Loop ileostomy versus loop colostomy for fecal diversion after colorectal or colonal anastomosis: a meta- analysis. Int J Colorectal Dis 24:479–488. https://doi.org/10.1007/s00384-009-0662-x
Gooszen AW et al (2000) Quality of life with a temporary stoma: ileostomy vs colostomy. Dis Colon Rectum 43:650–655. https://doi.org/10.1007/BF02235581
Persson E et al (2010) Stoma-related complications and stoma size -a 2-year follow up. Colorectal Dis 12:971–976. https://doi.org/10.1111/j.1463-1318.2009.01941.x
Edwards DP et al (2001) Stoma-related complications are more frequent after transverse colostomy than loop ileostomy: a prospective randomized clinical trial. Br J Surg 88:360–363. https://doi.org/10.1046/j.1365-2168.2001.01727.x
Law WL et al (2002) Randomized clinical trial comparing loop ileostomy and loop transverse colostomy for faecal diversion following total mesorectal excision. Br J Surg 89:704–708. https://doi.org/10.1046/j.1365-2168.2002.02082.x
Baker ML et al (2010) Cause and management of a high-output stoma. Colorectal Dis 13:191–197. https://doi.org/10.1111/j.1463-1318.2009.02107.x
Enomoto H et al (2021) Risk of outlet obstruction associated with defunctioning loop ileostomy in rectal cancer surgery. Cancer Diagnosis & Prognosis 1:465–470. https://doi.org/10.21873/cdp.10062
Tamura K et al (2019) Defunctioning loop ileostomy for rectal anastomoses: predictors of stoma outlet obstruction. Int J Colorectal Dis 34:1141–1145. https://doi.org/10.1007/s00384-019-03308-z
Ohira G et al (2018) Incidence and risk factor of outlet obstruction after construction of ileostomy. J Anus Rectum Colon 2:25–30. https://doi.org/10.23922/jarc.2017-034
Hara Y et al (2020) Organ/space infection is a common cause of high output stoma and outlet obstruction in diverting ileostomy. BMC Surg 20(1):83. https://doi.org/10.1186/s12893-020-00734-7
Sasaki S et al (2021) Risk factors for outlet obstruction after laparoscopic surgery and diverting ileostomy for rectal cancer. Surg Today 51:366–373. https://doi.org/10.1007/s00595-020-02096-2
Acknowledgements
The authors extend their thanks to Dr. Bryan J. Mathis of the University of Tsukuba Hospital International Medical Center for language and logical proofing the paper.
Funding
This study was not funded by any source.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by Koichiro Kumano and Daichi Kitaguchi. Data collection was performed by Koichiro Kumano and Eiki Kinoshita. Yohei Owada, Shoko Moue, Kinji Furuya, Yusuke Ohara, Tsuyoshi Enomoto, and Tatsuya Oda commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study conforms to the provisions of the 1964 Declaration of Helsinki and 2013 Brazil revisions.
Consent to participate
This study was approved by the Institutional Review Board of the University of Tsukuba Hospital (registration number: R01-110), and informed consent was obtained from all participants in the form of an opt-out option following the Good Clinical Practice Guidelines of the Ministry of Health and Welfare of Japan.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kumano, K., Kitaguchi, D., Owada, Y. et al. A comparative study of stoma-related complications from diverting loop ileostomy or colostomy after colorectal surgery. Langenbecks Arch Surg 408, 139 (2023). https://doi.org/10.1007/s00423-023-02877-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02877-6