Abstract
Purpose
While both anterior and posterior component separation techniques aid the repair of large ventral hernias, their outcomes can be remarkably dissimilar in terms of wound morbidity. We describe outcomes after open component separation by a single surgical team over the entire breadth of our experience.
Methods
We queried a prospectively maintained database for ventral hernias who received an open bilateral component separation between January 2014 and January 2020. A retrospective review was performed to analyze patient demographics, perioperative events, adverse outcomes, and recurrence.
Results
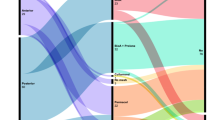
One hundred twenty-seven patients met the inclusion criteria of which 44 underwent anterior component separation (ACS) and 83 underwent posterior component separation (PCS). The two groups were broadly similar in terms of demographic and hernia-related variables. Mesh:defect area ratios, operative time, and estimated intraoperative blood loss were higher in the PCS group. The ACS group had more frequent use of drains which remained in situ for longer, along with a longer hospital stay. Surgical site occurrences (SSOs), including those needing procedural intervention (SSOPIs) were significantly more common after ACS. This group was also more likely to undergo a reoperation within 30 days of index repair. A single recurrence was noted in the ACS group after a mean follow-up duration of 43 months.
Conclusions
Open PCS may be more technically demanding than ACS, but it has a lower risk of postoperative morbidity and reoperation. While we now utilize PCS more frequently in our practice, ACS remains an important tool in our armamentarium.


Similar content being viewed by others
Data availability
The data is being maintained in a local database, and details are available at request from the corresponding author with masked identifying details.
Code availability
No custom software of code was employed for this research work.
References
Cherla DV, Moses ML, Viso CP, Holihan JL, Flores-Gonzalez JR, Kao LS, Ko TC, Liang MK (2018) Impact of abdominal wall hernias and repair on patient quality of life. World J Surg 42:19–25. https://doi.org/10.1007/s00268-017-4173-6
Langbach O, Bukholm I, Benth JŠ, Røkke O (2016) Long-term quality of life and functionality after ventral hernia mesh repair. Surg Endosc 30:5023–5033. https://doi.org/10.1007/s00464-016-4850-9
Holihan JL, Askenasy EP, Greenberg JA, Keith JN, Martindale RG, Roth JS, Mo J, Ko TC, Kao LS, Liang MK (2016) Component separation vs. bridged repair- a multi- institutional risk adjusted comparison, systematic review, and meta-analysis. Surg Infect 17:17–26. https://doi.org/10.1089/sur.2015.124
Cobb WS, Carbonell AM, Kalbaugh CL, Jones Y, Lokey JS (2009) Infection risk of open placement of intraperitoneal composite mesh. Am Surg 75:762–767. https://doi.org/10.1177/000313480907500905
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204:709–716. https://doi.org/10.1016/j.amjsurg.2012.02.008
Sneiders D, Yurtkap Y, Kroese LFL, Jeekel J, Muysoms FE, Kleinrensink GJ, Lange JF (2019) Anatomical study comparing medialization after Rives-Stoppa, anterior component separation, and posterior component separation. Surgery 165:996–1002. https://doi.org/10.1016/j.surg.2018.11.013
Hodgkinson JD, Leo CA, Maeda Y, Bassett P, Oke SM, Vaizey CJ, Warusavitarne J (2018) A meta-analysis comparing open anterior component separation with posterior component separation and transversus abdominis release in the repair of midline ventral hernias. Hernia 22:617–626. https://doi.org/10.1007/s10029-018-1757-5
Tanaka EY, Yoo JH, Rodrigues AJ, Utiyama EM, Birolini D, Rasslan S (2010) A computerized tomography scan method for calculating the hernia sac and abdominal cavity volume in complex large incisional hernia with loss of domain. Hernia 14:63–69. https://doi.org/10.1007/s10029-009-0560-8
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RKJ, Simons MP, Śmietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
AJ M, TC H, ML P, LC S, WR J (2000) Guideline for prevention of surgical site infection. Bull Am Coll Surg 85:23–29. https://doi.org/10.1086/501620
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia 22:737–738. https://doi.org/10.1007/s10029-018-1813-1
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–526. https://doi.org/10.1097/00006534-199009000-00023
Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, Orenstein SB (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264:226–232. https://doi.org/10.1097/SLA.0000000000001673
Punjani R, Shaikh I, Soni V (2015) Component separation technique: an effective way of treating large ventral hernia. Indian J Surg 77:1476–1479. https://doi.org/10.1007/s12262-015-1265-0
Punjani R, Arora E, Mankeshwar R, Gala J (2021) An early experience with transversus abdominis release for complex ventral hernias: a retrospective review of 100 cases. Hernia 25:353–364. https://doi.org/10.1007/s10029-020-02202-w
Majumder A, Miller HJ, del Campo LM, Soltanian H, Novitsky YW (2018) Assessment of myofascial medialization following posterior component separation via transversus abdominis muscle release in a cadaveric model. Hernia 22:637–644. https://doi.org/10.1007/s10029-018-1771-7
Majumder A, Martin-del-Campo LA, Miller HJ, Podolsky D, Soltanian H, Novitsky YW (2020) Evaluation of anterior versus posterior component separation for hernia repair in a cadaveric model. Surg Endosc 34:2682–2689. https://doi.org/10.1007/s00464-019-07046-9
Helgstrand F (2016) National results after ventral hernia repair. Dan Med J 63(7):B5258
Singhal V, Szeto P, VanderMeer TJ, Cagir B (2012) Ventral hernia repair: outcomes change with long-term follow-up. J Soc Laparoendosc Surg 16:373–379. https://doi.org/10.4293/108680812X13427982377067
Maloney SR, Schlosser KA, Prasad T, Kasten KR, Gersin KS, Colavita PD, Kercher KW, Augenstein VA, Heniford BT (2019) Twelve years of component separation technique in abdominal wall reconstruction. Surgery 166:435–444. https://doi.org/10.1016/j.surg.2019.05.043
Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ (2012) Posterior and open anterior components separations: a comparative analysis. Am J Surg 203:318–322. https://doi.org/10.1016/j.amjsurg.2011.10.009
Saulis AS, Dumanian GA (2002) Periumbilical rectus abdominis perforator preservation significantly reduces superficial wound complications in "separation of parts" hernia repairs. Plast Reconstr Surg 109:2275–80; discussion 2281–2. https://doi.org/10.1097/00006534-200206000-00016
Lowe JB, Garza JR, Bowman JL, Rohrich RJ, Strodel WE (2000) Endoscopically assisted “components separation” for closure of abdominal wall defects. Plast Reconstr Surg 105:720–9; quiz 730 . https://doi.org/10.1097/00006534-200002000-00039
Scheuerlein H, Thiessen A, Schug-Pass C, Köckerling F (2018) What do we know about component separation techniques for abdominal wall hernia repair? Front Surg 5:24. https://doi.org/10.3389/fsurg.2018.00024
Ghali S, Turza KC, Baumann DP, Butler CE (2012) Minimally invasive component separation results in fewer wound-healing complications than open component separation for large ventral hernia repairs. J Am Coll Surg 214:981–989. https://doi.org/10.1016/j.jamcollsurg.2012.02.017
Cornette B, De Bacquer D, Berrevoet F (2018) Component separation technique for giant incisional hernia: a systematic review. Am J Surg 215:719–726. https://doi.org/10.1016/j.amjsurg.2017.07.032
Kumar S, Edmunds RW, Callie D, Wayne Chang YW, King R, Roth JS (2018) Anterior versus posterior component separation: which is better? Plast Reconstr Surg 142:47S-53S. https://doi.org/10.1097/PRS.0000000000004852
Arnold M, Otero J, Schlosser KA, Kao A, Prasad T, Lincourt AEA, Augenstein VVA, Heniford BT (2018) A decade of components separation technique: an increasing trend in open ventral hernia repair. - Academic Surgical Congress Abstracts Archive. In: American College of Surgeons. p 70.10
Author information
Authors and Affiliations
Contributions
Ramesh Punjani and Eham Arora contributed to the study conception and design. Material preparation and data acquisition were performed by Eham Arora, Emily Coughlin, and Rahul Mhaskar. Analysis and interpretation of data were performed by Ramesh Punjani, Eham Arora, and Rahul Mhaskar. The first draft of the manuscript was written by Eham Arora, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
An institutional ethics committee approval was obtained for this retrospective analysis of data. All procedures being performed as a part of the study were a part of routine care. This research work is compliant with STROBE guidelines for observational studies.
Informed consent for participation and publication.
Prior to surgical intervention, all participating patients have consented to undergo the procedural interventions described as well as the collection of their data and its subsequent analysis and publication.
Conflict of interest
• Dr. Ramesh Punjani declares no competing interests.
• Dr. Eham Arora has received honoraria for speaking engagements from Johnson & Johnson Pvt Ltd, India and is a partner in HerniaCAT Surgical Radiology Inc. This is beyond the scope of the submitted work.
• Ms. Emily Coughlin declares no competing interests.
• Dr. Rahul Mhaskar declares no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Punjani, R., Arora, E., Coughlin, E. et al. A retrospective comparison of outcomes after open anterior and posterior component separation by a single surgical team. Langenbecks Arch Surg 407, 1701–1709 (2022). https://doi.org/10.1007/s00423-022-02438-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02438-3