Abstract
Purpose
Prognostic factors for survival ≥ 15 years and life years lost after liver transplantation are largely unknown.
Methods
One thousand six hundred thirty primary adult liver transplants between 1983 and 2014 were analyzed. Risk factors for survival were identified with multivariable Cox regression and subsequently tested for their relevance as prognostic factors for observed 15-year survival using multivariable logistic regression and c statistics. The difference of life expectancy between a matched national reference population and survival in patients with post-transplant survival ≥ 15 years was calculated.
Results
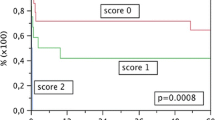
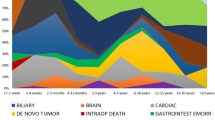
Survival of ≥ 15 years was observed in 361 patients (22%). Sixty-nine adults died after more than 15 years losing a median of 15 years of life expectancy. One of those patients lived longer while 292 patients still have the chance to survive longer than their normal life expectancy. The indication primary sclerosing cholangitis (PSC) and later eras of transplantation were identified as significant independent protective factors while recipient age > 36.8 years, graft loss due to initial non-function or thrombosis, the indications hepatocellular carcinoma (HCC), hepatitis-C-virus-related cirrhosis (HCV-cirrhosis) and all other indications, donor age > 53 years, the number of surgical complications, and operative durations > 4.5 h were identified as significant independent risk factors limiting survival. All of these factors except the duration of operation had also a significant independent influence on observed 15-year survival (AUROC = 0.739).
Conclusions
Recipients can exceptionally live longer than their normal life expectancy. Older recipients and patients with the indications HCC, HCV-cirrhosis, or other indications except PSC, should be transplanted with younger donor organs.





Similar content being viewed by others
References
Starzl TE, Porter KA (1969) Clinical and pathologic observations after orthotopic transplantation of the human liver. Surg Gynecol Obstet 128:327–339
National Institutes of Health Consensus Development Conference Statement (1984) Liver Transplantation-June 20-23. Hepatology 4:107S–110S
Neuberger J, Ferguson J, Newsome PN (2014) Liver transplantation: clinical assessment and management. Wiley Blackwell, United Kingdom
Jain A, Reyes J, Kashyap R, Dodson F, Demetris AJ, Starzl TE et al (2000) Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg 232:490–500
Busuttil RW, Farmer DG, Yersiz H, Hiatt JR, McDiarmid SV, Goldstein LI et al (2005) Analysis of long-term outcomes of 3200 liver transplantations over two decades: a single-center experience. Ann Surg 241:905–916 discussion 916–8
Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M, Pollard S, Lerut J, Paul A, Garcia-Valdecasas JC, Rodríguez FS, Burroughs A, All contributing centers (www.eltr.org), European Liver and Intestine Transplant Association (ELITA) (2012) Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol 57:675–688. https://doi.org/10.1016/j.jhep.2012.04.015
Åberg F, Gisslaer M, Karlsen TH, Ericzon B-G, Foss A, Isoniemi H (2015) Differences in long-term survival among liver transplant recipients and the general population: a population-based Nordic Study. Hepatology 61(2):668–677. https://doi.org/10.1002/hep.27538
Neuberger J, James O (1999) Guidelines for selection of patients for liver transplantation in the era of donor-organ shortage. Lancet 354:1636–1639. https://doi.org/10.1016/S0140-6736(99)90002-8
Kaltenborn A, Hartmann C, Salinas R, Ramackers W, Kleine M, Vondran FW et al (2015) Risk factors for short- and long-term mortality in liver transplant recipients with MELD score ≥30. Ann Transplant 20:59–69. https://doi.org/10.12659/AOT.892322
Schrem H, Focken J, Gunson B, Reichert B, Mirza D, Kaltenborn A et al (2016) The new liver allocation score for transplantation is validated and improved transplant survival benefit in Germany but not in the United Kingdom. Liver Transpl 22:743–756. https://doi.org/10.1002/lt.24421
Schrem H, Volz S, Koch H, Gwiasda J, Kürsch P, Goldis A et al (2017) Statistical approach to quality assessment in liver transplantation. Langenbeck’s Arch Surg 403:61–71. https://doi.org/10.1007/s00423-017-1612-7
Lee KJ, Carlin JB (2010) Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol 171:624–632. https://doi.org/10.1093/aje/kwp425
Hosmer DW, Lemeshow S, Sturdivant RX (2013) Applied Logistic Regression. Wiley, Canada
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Cuervas-Mons V, de la Rosa G, Pardo F, San Juan F, Valdivieso A (2015) Activity and results of liver transplantation in Spain during 1984-2012. Analysis of the Spanish Liver Transplant Registry. Med Clin 144:337–347. https://doi.org/10.1016/j.medcli.2014.07.036
Gwiasda J, Schrem H, Klempnauer J, Kaltenborn A (2017) Identifying independent risk factors for graft loss after primary liver transplantation. Langenbeck’s Arch Surg 402:757–766. https://doi.org/10.1007/s00423-017-1594-5
Grant support
This work was supported by a grant from the German Federal Ministry of Education and Research (reference number 01EO1302).
Author information
Authors and Affiliations
Contributions
Soufiane Filali Bouami: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript. Jill Gwiasda: analysis and interpretation of data, critical revision of manuscript. Jan Beneke: study conception and design, analysis, and interpretation of data. Alexander Kaltenborn: analysis and interpretation of data, critical revision of manuscript. Sebastian Liersch: study conception and design, critical revision of manuscript. Eduardo M. Suero: study conception and design, analysis and interpretation of data, critical revision of manuscript. Hans-Friedrich Koch: study conception and design, critical revision of manuscript. Christian Krauth: study conception and design, critical revision of manuscript. Jürgen Klempnauer: critical revision of manuscript. Harald Schrem: study conception and design, analysis and interpretation of data, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Committee of Hannover Medical School approved of this retrospective study (approval decision number 1683-2013).
Informed consent
Informed consent was obtained from all individual participants included in the study. Patients provided informed consent that their data may be used for scientific purposes at the time of hospital admission which is the general policy of our institution.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Filali Bouami, S., Gwiasda, J., Beneke, J. et al. Prognostic factors for long-term survival after adult liver transplantation. Langenbecks Arch Surg 403, 495–508 (2018). https://doi.org/10.1007/s00423-018-1670-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1670-5