Abstract
Purpose
To evaluate the agreement between the two Gas Exchange Thresholds (GETs = GET1 and GET2), identified by the conventional V-Slope method, and two Respiratory Frequency Thresholds (fRTs = fRT1 and fRT2) obtained from a novel, low-cost, and simple method of breakpoint determination.
Methods
Fifty middle-aged males (age: 50–58 years; \(\dot{V}\)o2peak: 37.5 ± 8.6 mL·Kg−1·min−1), either healthy or with chronic illnesses, underwent an incremental cycle exercise test to determine maximal oxygen uptake (\(\dot{V}\)o2max/\(\dot{V}\)o2peak), GETs and fRTs.
Results
There were no statistical differences [P > 0.05; ES: 0.17 to 0.32, small] between absolute and relative (56–60% \(\dot{V}\)o2peak) oxygen uptake (\(\dot{V}\)o2) values at GET1 with those obtained at fRT1, nor between \(\dot{V}\)o2 values at GET2 with those at fRT2 (76–78% \(\dot{V}\)o2peak). Heart rate (HR) at fRT1, and \(\dot{V}\)o2 and HR at fRT2 showed very large correlations (r = 0.75–0.82; P < 0.001) and acceptable precision (SEE < 7–9%) in determination of their corresponding values at GET1 and GET2. The precision in the estimation of \(\dot{V}\)o2 at GET1 from fRT1 was moderate (SEE = 15%), while those of power output at GET1 (SEE = 23%) and GET2 (SEE = 12%) from their corresponding fRTs values were very poor to moderate.
Conclusion
HR at fRT1 and \(\dot{V}\)o2 and HR at fRT2, determined using a new objective and portable approach, may potentially serve as viable predictors of their respective GETs. This method may offer a simplified, cost-effective, and field-based approach for determining exercise threshold intensities during graded exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maximal oxygen uptake (\(\dot{V}\)o2max/\(\dot{V}\)o2peak) attained during maximal graded exercise testing is the most commonly utilized measure to quantify aerobic fitness and cardiorespiratory health in both healthy and patients individuals (Iannetta et al. 2019a, b; Meyer et al. 2005; Powers et al. 1984).
Two submaximal breakpoints or thresholds of important physiological and metabolic implications (Hagberg 2022), occurring at variable fractions of \(\dot{V}\)o2max, have been traditionally identified from the profiles of pulmonary gas exchange and ventilatory measures during maximal graded exercise (Keir et al. 2015, 2022): (1) The first threshold, referred to as the “first gas exchange threshold (GET1)” (Keir et al. 2022) in this paper, corresponds to the first disproportionate increase in the rates of pulmonary carbon dioxide output (\(\dot{V}\)co2) compared to oxygen uptake (\(\dot{V}\)o2) as the work rate increases. Alternative markers of GET1 are the steeper increase in minute ventilation (\(\dot{V}\)E) compared to \(\dot{V}\)o2 with no increase in \(\dot{V}\)E compared to \(\dot{V}\)co2, or an increase in end-tidal oxygen expiration (PETO2) with no decrease in end-tidal carbon dioxide expiration (PETCO2) (Beaver et al. 1986). (2) The second threshold, referred to as the “second gas exchange threshold (GET2)” (Keir et al. 2022) in this paper, is reached at a higher relative intensity than GET1 and marks the first disproportionate rise in \(\dot{V}\)E compared to \(\dot{V}\)co2. Alternative indicators of GET2 are a second steeper increase in \(\dot{V}\)E compared to \(\dot{V}\)o2 or/and the point at which PETCO2 start to decrease after an apparent steady state (Beaver et al. 1986; Meyer et al. 2005; Whipp et al. 1989).
There is currently no widely accepted method for determination of GETs (Keir et al. 2022; Shimizu et al. 1991). Traditional methods involved inspecting graphical plots, which heavily relied on subjective evaluation (Hagberg 2022; Wasserman et al. 1973). Other methods involve objective computerized techniques, with the most cited method (> 2.700 times) (Hagberg 2022) being the so-called “V-slope” method. This method, proposed by Beaver, Wasserman and Whipp in the mid 1980’s (Beaver et al. 1986), involves a mathematical analysis of the slopes of the \(\dot{V}\)E and CO2 output curves to determine GET2, followed by an analysis of the slopes of CO2 and O2 output curves to determine GET1. Finally, some authors utilize a combination of visual and computerized methods in their decision-making (Keir et al. 2022).
These methods have raised concerns regarding their validity and reliability (Powers et al. 1984). In addition, in up to 40% of cases, some of these methods fail to detect deflection points due to irregular physiological behavior (Cheng et al. 1992). Another major limitation is that they require costly and sophisticated laboratory equipment, expert testers, and rather complex interpretive procedures (Carey et al. 2005; James et al. 1989). These limitations restrict the assessment and application of both GETs to laboratory environments (Carey et al. 2005; Cross et al. 2012; Nabetani et al. 2002; Neder and Stein 2006). Considering the importance of these thresholds, it may be beneficial to explore a more economical and straightforward technique for identifying both GET1 and GET2 (Neder and Stein 2006).
Changes in the respiratory rate, also referred to as respiratory frequency (fR), during exercise, have traditionally been disregarded (Nicolo et al. 2020). Since \(\dot{V}\)E is the algebraic product of the mean tidal volume (Vt) and fR, it could be expected that disproportionate changes in Vt and/or fR would occur close to GET1 and GET2. Martin et al. ( 1979) and Whipp, Davis and Wasserman 10 years latter (Whipp et al. 1989) pointed out through subjective visual inspection that the disproportionate and progressive increase in \(\dot{V}\)E compared to \(\dot{V}\)o2 that occur at GET1 was quite coincidental with a disproportionate increase in fR (referred to as respiratory frequency threshold 1 “fRT1” in this paper). In the figures reported by these authors, a clear second acceleration in \(\dot{V}\)E compared to \(\dot{V}\)o2 can be observed around GET2. This acceleration is primarily driven by a much faster increase in fR (referred to as respiratory frequency threshold 2 “fRT2” in this paper). Since then, we have found nine relevant studies that compare GETs and Respiratory Frequency Thresholds (fRTs) during graded cycling exercise (Cannon et al. 2009; Carey et al. 2005, 2009; Cheng et al. 1992; Cross et al. 2012; James et al. 1989; Nabetani et al. 2002; Neary et al. 1995; Neder and Stein 2006). Although these studies have reported nonlinear changes in fR data occurring at exercise intensities corresponding to GET1 and/or GET2 during progressive exercise, their results are highly variable primarily due to differing stage durations in their protocols [from 1 (Cannon et al. 2009; Carey et al. 2005, 2009; Cross et al. 2012; Nabetani et al. 2002; Neder & Stein 2006) to 2–5 min (Cheng et al. 1992; James et al. 1989; Neary et al. 1995)], method of GETs or fRTs determination [visual (James et al. 1989; Nabetani et al. 2002; Neary et al. 1995), mathematical (Carey et al. 2005, 2009; Cheng et al. 1992; Cross et al. 2012) or a combination of both (Cannon et al. 2009; Neder and Stein 2006)], number of threshold detected [two (Carey et al. 2005, 2009; Cheng et al. 1992; James et al. 1989; Nabetani et al. 2002; Neary et al. 1995) or four (Cannon et al. 2009; Cross et al. 2012; Neder & Stein 2006)], and statistical analysis performed [with (Cannon et al. 2009; Cheng et al. 1992; Cross et al. 2012; James et al. 1989; Nabetani et al. 2002; Neary et al. 1995) or without (Carey et al. 2005, 2009; Neder & Stein 2006) regression analysis, and with (Cannon et al. 2009; Cross et al. 2012) or without (Carey et al. 2005, 2009; Cheng et al. 1992; James et al. 1989; Nabetani et al. 2002; Neary et al. 1995; Neder and Stein 2006) additional bias and agreement analyses]. In fact, only two of these studies (Cannon et al. 2009; Cross et al. 2012), the most recent ones, met stringent methodological requirements. However, one major limitation of these two studies is that 42% (Cannon et al. 2009) and 50% (Cross et al. 2012) of participants had one or more of the four thresholds labeled as “undetermined”. Thus, it becomes challenging to draw conclusions about the validity of fR analyses for determining GETs with a strict methodology.
A common feature among all of the aforementioned studies is that they were conducted on young healthy participants who were either recreational or endurance-trained. To our knowledge, there has not been a comprehensive and methodologically appropriate comparison between GETs and fRTs among middle-aged individuals, including those with chronic illnesses. In light of these considerations, the purpose of the current study was to assess the level of agreement between GETs identified by the conventional V-slope method and the fRTs obtained using a new, low-cost, portable and objective mathematical method for breakpoint determination, on middle-aged individuals both healthy or with cardiovascular metabolic diseases.
We hypothesized that fR can be used to estimate GETs during incremental cycling exercise for the first time in middle-aged participants both healthy and with cardiovascular or metabolic diseases, using a simple, objective, cost-effective and strict methodological approach. Consistent with previous research (Beaver et al. 1986; Weston & Gabbett 2001), we hypothesized that estimating HR, \(\dot{V}\)o2 and PO at GET2 based on the corresponding values at fRT2, would be significantly more accurate than estimating these variables at GET1. If the hypotheses are confirmed, this simplified method can be used to safely, non-invasively and inexpensively evaluate cardiovascular fitness in middle-aged adults who are healthy or have chronic diseases. It can also be used for individualizing exercise prescription and measuring the effectiveness of endurance training programs.
Methods
Study design and participants
This was a retrospective, cross-sectional, method comparison study conducted in a single laboratory session. Its primary objective was to evaluate the agreement between a new objective method of fRTs identification and the conventional GETs identification method commonly used in clinical settings. A group of 25 healthy males (HS group, 53.3 ± 2.7 years, range: 50–58), and a group of 25 males with chronic illnesses (DS group, 53.5 ± 2.4 years, range: 50–58), all of them professional firefighters, volunteered. The DS group consisted of clinically stable participants with documented single or multiple diseases including coronary heart disease (n = 10), hypertension (n = 10), cardiac arrhythmia (n = 9), obesity (n = 5), diabetes (n = 4), hyperlipidemia (n = 2), and syncope (n = 1). All participants consistently followed the mandated physical training program implemented by their fire department. They were informed about the risks and benefits of the study, and gave written consent. Procedures were approved by the Local Institutional Review Board and conformed to the Declaration of Helsinki and Tokyo.
Cycling exercise test
The participants visited once the laboratory (23.3 ºC ± 1.4 ºC) in the afternoon, after a light meal at least 3 h prior to testing. They refrained from consuming caffeinated or alcoholic beverages and avoided strenuous or non-habitual exercise for 24 h before testing. All participants were familiar with the equipment and testing procedures.
Each participant completed an incremental exercise test until the point of exhaustion on a mechanically braked cycle ergometer (Monark Ergomedic 824E, Varbeg, Sweden), equipped with toe clips, at a constant pedaling rate of 80 rpm. After a 5-min rest sitting on the cycle ergometer, each participant began with unloaded cycling for 1 min. The workload was then incremented by 20 W each minute until exhaustion or until the required pedaling cadence could not be maintained. The maximal workload of each cycling test (Wmax) was defined as the power output (PO) of the last completed stage. Maximal heart rate (HRmax) was defined as the highest heart rate (HR) achieved during the test. \(\dot{V}\)o2max was determined using the criteria described elsewhere (American College of Sports Medicine 2014; Garcia-Tabar et al. 2015). Because some participants did not meet the criteria, we used the term \(\dot{V}\)o2peak instead of \(\dot{V}\)o2max.
Participants were equipped with thoracic electrodes to record complete 12-lead ECG tracings during exercise, using the Cardioline ETA system (REMCO, Milan, Italy). HR was continuously monitored from the ECG and averaged during the final 10 s of each stage.
Collection of respiratory gases
Participants breathed through a properly sized silicone mask, which was adjusted using a headgear and connected to a lightweight Teflon respiratory block containing two low-resistance valves (ETBM VS1, Chassieu, France). Metabolic data were continuously collected breath by breath using an automated system MMMS7785 (Marianne Modular Metabolism System, TBM, Chassieu, France) composed of an inspiratory circuit connected by a motor-driven tap (X 4_VA Ets Peysson, Vaux en Velin, France) to a pneumotachograph (PN01: 0–12 L·min−1, TBM, Chassieu, France), a MP45 ± 1 cm H2O differential low-pressure transducer and a demodulator (CD23, Validyne, Onrion, USA) or a standardized ATPS pump (PEA-02, Ets Peysson_SARL, Vaux en Velin, France) with a tidal volume of 0.5–2.5 L and a frequency of 0–60 min−1. The expiratory circuit was connected alternatively to one of the two mixing rubber bags and analyzed breath by breath by a MGC-03system (TBM, Lyon, France). It also included O2 (Polarographic OM11, Beckman Instruments, USA) and CO2 (Datex, Gauthier, France) analyzers to measure the concentrations of these gases online. The response times of these analyzers were of 80 ms (O2) and 50 ms (CO2). \(\dot{V}\)E, fR and VT were calculated using a signal generated by the output transducer of the pneumotachograph sensor. From these measurements, the metabolic cart’s computer calculated the \(\dot{V}\)o2 and \(\dot{V}\)co2 (in liters per minute), respiratory exchange ratio (RER = \(\dot{V}\)co2/\(\dot{V}\)o2), and the ventilatory equivalents for O2 (\(\dot{V}\)E/\(\dot{V}\)o2) and CO2 (\(\dot{V}\)E/\(\dot{V}\)co2) as follows.
\(\dot{V}\)o2 calculation:
Ambient air:
\(\dot{V}\)Co2 calculation:
being
\(\dot{V}\)I = ventilatory inspiration. FI = inspiratory fraction. FE = expiratory fraction.
The metabolic measurement software (Marianne met 12; TBM, Lyon—France) reported metabolic data over the last 10-s average of breath-by breath data of each stage, and adjusted the volume of the expired air to standard conditions (STPD: 0 ºC, 760 mmHg and a dry condition).
The O2 and CO2 analyzers were calibrated immediately prior to each test using two-point calibration with two precision-analyzed gas mixtures humidified at 100% (ambient air at 20.93% O2 and 0.03% CO2; highly precise calibration gas at 16% O2 and 4% CO2, and balanced nitrogen). Pneumotachograph flow calibration was determined with a high-precision pump that permitted the use of varying volumes and frequencies included within the physiological range of fR and VT values observed during an incremental maximal cycling test.
Within 15 s of completing each exercise trial, calibration gases and the flow sensor were verified and compared with the calibration references. These verifications were run through the metabolic system to assess whether the analyzers and the pneumotachograph experienced any drift during the measurement period. When drifts were observed in these readings, the measured metabolic data were corrected in accordance with previous recommendations (Garcia-Tabar et al. 2015; Ward 2018).
Determination of first (GET1) and second (GET2) gas exchange thresholds
GET2 determination. GET2 was calculated using the \(\dot{V}\)E/\(\dot{V}\)co2 relationship as proposed by Beaver et al. (Beaver et al. 1986). At first, we removed the data from the initial two stages (0 and 20 W) and the last stages where an increase in \(\dot{V}\)o2 of less than 120 mL·min−1 was recorded from completed stage to completed stage. We generated two regression lines with each value: one based on the values at and below a given \(\dot{V}\)E/\(\dot{V}\)co2 value and the other based on the values at and above that value. To mathematically calculate the GET2, the breaking point separating the two regions from a given value was systematically moved to the next value until the two lines best fit the data by maximizing the ratio of the greatest distance of the intersection point from the single regression line of the data to the mean square error of regression. According to Beaver et al. (1986), the value corresponding to the best fit of two lines was considered as the GET2 value only if the change in slope was greater than 15%. If the change in slope was less than or equal to 15%, the GET2 was considered as “undeterminate”.
GET1 determination. After determining GET2, we calculated GET1 using the \(\dot{V}\)co2/\(\dot{V}\)o2 relationship through the classic V-slope method developed by Beaver et al. (Beaver et al. 1986). We excluded the data from the initial two stages (0 and 20 W), any data of the initial segment of the curve that displays a slope of less than < 0.6, and all data exceeding GET2. At first, we visually identified the \(\dot{V}\)co2/\(\dot{V}\)o2 breaking point. We then computed two regression lines: one from the values at and below the breakpoint and the other from the values at and above this breakpoint. The breaking point was moved until achieving the best fit between the two regression lines as above described for GET2. This GET1 value was only accepted if the change in slope from the lower segment to the upper segment was greater than 0.1 (Beaver et al. 1986). If it was less than or equal to 0.1 the GET1 was considered as “undetermined”. If it was greater than 0.1 its location was transferred to the \(\dot{V}\)co2/\(\dot{V}\)o2.
Determination of first (fRT1) and second (fRT2) respiratory frequency thresholds
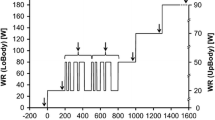
fRT1 determination: Figure 1 depicts the determination of fRT1 and fRT2 for a representative participant. The numerical data of this participant is displayed in Table 1. fRT1 and fRT2 were defined mathematically in the following way:
Example of respiratory frequency (fR) vs. heart rate (HR) plot and determination of fR threshold 1 (fRT1) and 2 (fRT2) during incremental exercise in a representative participant. The numerical data of this participant, including the determination of “provisional” fRT1 and fRT2 are shown in Table 1. The three regression lines (RL1, RL2 and RL3) are depicted in dashed lines. Regression lines obtained from data reported in Table 1 are: RL1: HR = (0.1399 * fR) + 1.9233; RL2: HR = (0.3333 * fR) – 26.179; RL3: HR = (2.3453 * fR) − 361.17. The intersection points between RL1 and RL2 (i.e. fRT1) and between RL2 and RL3 (i.e. fRT2) are the following: fRT1: HR = 146; fR = 22.3, and fRT2: HR = 167; fR = 29.3
For a specific stage (i) and its corresponding respiratory frequency (fRi), we computed:
The average of the precedent fR values, not including fRi:
and the standard deviation (SD) of these data (SDi−1) as well as 2 times the value of SDi−1 (2 * SDi−1).
The fR data from all stages (from stage “1” to stage “i−1”), including the stages from 0 to 60W, were used to calculate the average fRi−1 and SDi−1 (Table 1).
The initial calculation of the “provisional” fRT1 required identifying the first stage at which (fRi—Average fRi−1) exceeded 2*SDi–1, provided that the PO exceeded 60 watts. An increase in fR in a given stage greater than two times the standard deviation of the average fR of the previous stages, indicates a meaningful and significant change in fR compared to previous values. This corresponds to the 95% confidence interval, which provides a range of plausible values for fR above which we considered that a significant disproportionate increase in fR occurred. The restriction of the first stages or minutes of exercise to calculate fRT1 aims to ensure that the computer model follows the major trend of the data and is not excessively influenced by the minor hyperventilation typically observed at the start of an incremental exercise test (Beaver et al. 1986; Keir et al. 2022; Ozcelik et al. 1999; Zuccarelli et al. 2018). There is no agreement on the optimal number of initial stages to exclude for the subsequent determination of GETs. For that reason, to determine frTs, we preliminarily calculated frTs values by excluding the first two, three, four or five stages. We found that excluding the first 4 stages (up to 60 W) resulted in more consistent frTs values that were more acceptably related to GETs values. Additionally, this exclusion allowed for the calculation of frTs in a larger number of subjects, with 98% of the sample being included.
The initial calculation of the “provisional” fRT2 required identifying the first subsequent stage to “provisional fRT1” where (fRi—Average fRi−1) exceeds 2*SDi−1 once again.
Once the”provisional” fRT1 and the “provisional” fRT2 were identified, three regression lines (RLs) were calculated: (1) RL1: all the points from 0 W to the “provisional” fRT1, including the 0 W stage and the “provisional” fRT1 point, (2) RL2: all the points from the “provisional fRT1” to the “provisional fRT2”, including both provisional points, and (3) RL3: all the points from the “provisional fRT2” to the last completed stage (Wmax), including these two points. The intersection between the RL1 and RL2 was defined as the “final fRT1” (henceforth referred to as fRT1). Similarly, the intersection between RL2 and RL3 was defined as the “final fRT2” (henceforth referred to as fRT2).
Once fRT1 and fRT2 were calculated from fR and HR, the \(\dot{V}\)o2 (in L·min−1), and PO (in watts) corresponding to fRT1 and fRT2 were determined from the linear regression equations of \(\dot{V}\)o2 vs. HR, and \(\dot{V}\)o2 vs. PO, respectively.
Statistical analyses
Standard statistical methods were used to calculate means, SDs, standard errors of the estimates (SEEs) and confidence intervals (CIs). Data normality and homoscedasticity were checked. Differences between DS and HS, and between GETs and fRTs, were assessed using Student’s paired t tests and Hedges’ g effect sizes (ES) (Hedges 1981). ES thresholds were small (0.2), moderate (0.6), large (1.2) and very large (2.0) (Hopkins et al. 2009). Agreement plots (Bland and Altman 1986) were used to illustrate the mean bias and limits of agreement (LOAs) between GETs and fRTs. Linear regression analyses with Pearson’s product-moment correlation coefficients (r) were used to determine the magnitude of the relationships between GETs and fRTs. Correlation magnitudes were interpreted according to the following threshold effects (Hopkins et al. 2009): small (0.1), moderate (0.3), large (0.5), very large (0.7) and extremely large (0.9). The accuracy of each regression was assessed using SEEs and CIs. The relative SEE was also calculated as a percentage of the mean, and classified as excellent (< 2%), good (< 5%), acceptable < (10%), moderate (< 15%), poor (< 20%) or very poor (≥ 20%) (Crouter et al. 2006). Analyses were performed using IBM SPSS Statistics 22 (IBM Corporation, Armonk, USA). Statistical significance was set at P < 0.05. Data are reported as mean (SD).
Results
Exclusion of participants
GET2 was “undetermined” in 4 out of the 50 participants (three in HS and one in DS). GET1 could not be calculated in the 4 participants in whom GET2 was “undetermined” and in 3 other participants (one in HS and two in DS). fRT1 and fRT2 were calculated for all participants except for one individual in the DS group. This participant was the individual with the shortest test duration (8 min) and therefore lowest Wmax (140 W). As a result, a total of 8 out of the 50 participants (4 in HS and 4 in DS) were excluded. The following section presents data from the 42 participants (n = 21 in HS; n = 21 in DS) in whom all the four thresholds were determined.
Physical characteristics
No differences were observed between the HS and DS groups in age (53.3 ± 2.5 and 53.8 ± 2.4 years; P = 0.52; ES: 0.20, small) and body height (172.2 ± 6.7 cm and 171.2 ± 6.2 cm; P = 0.62; ES: 0.16). Body mass and body mass index were higher (P < 0.01; ES: 0.65 to 0.83, moderate) in DS (82.1 ± 13 kg; 28 ± 3.8 kg·m−2) than in HS (75.1 ± 8.1 kg; 25.3 ± 2.6 kg·m−2).
Cycling exercise test
The average duration of the maximal cycling exercise test was 13 min (range: 8–16). Wmax achieved was 14% higher (P < 0.01; ES: 0.85, moderate) in the HS (258 ± 43 W) than in the DS (227 ± 28 W). \(\dot{V}\)o2peak was 33% higher (P < 0.001; ES: 1.56, large) in HS (42.8 ± 8.2 mL·Kg−1·min−1; range: 25–62.2) than in DS (32.2 ± 5.0 mL·Kg−1·min−1; range: 24.2 – 42.6). No differences (P < 0.05; ES < 0.25, small) between groups were observed in HRmax (HS: 176 ± 10; DS: 176 ± 13 beats·min−1), RERmax (HS: 1.10 ± 0.08; DS: 1.12 ± 0.08), nor in maximal fR (HS: 54.8 ± 17.8; DS: 51.0 ± 14.9 breaths·min−1).
Determinations of gas exchange (GET) and respiratory frequency (fRT) thresholds
Table 2 displays the average values of fR, HR, \(\dot{V}\)o2, and PO for each threshold. The absolute \(\dot{V}\)o2 at both GETs were 17–18% greater in HS than in DS (ES: 0.72 to 1.05, moderate). However, there was no difference expressed as a percentage of \(\dot{V}\)o2peak (ES: 0.19 to 0.44, small). At GET1 and fRT1, fR was 10% lower in HS compared to DS (ES: 0.63 to 0.69, moderate). In both groups no significant differences were found in \(\dot{V}\)o2 (in L·min−1 or %\(\dot{V}\)o2peak) between GET1 and fRT1 or between GET2 and fRT2 (ES: 0.17–0.32, small). Concerning the HR at the thresholds, only a significant difference (P < 0.05) was found between HR at fRT1 and HR at GET1. However, this difference was clinically small (5 beats·min−1; ES: 0.38). In the HS group, fR at fRT2 was statistically higher than at GET2, but the difference was also small (3 breath·min−1; ES: 0.30). No differences (P > 0.05; ES: 0.17–0.41, small) were observed in PO between GETs and fRTs in HS or DS groups.
Agreement and linear regression analyses between gas exchange (GETs) and respiratory frequency (fRT) thresholds
Figure 2 shows agreement plots between GETs and fRTs. Regression analyses showed non-significant (P = 0.20 to 0.83) relationships between the differences (Y axes) and the means (X axes), indicating that there was no any systematic error. There were no significant differences between fRTs and GETs (P > 0.05; ES: 0.09–0.36, small). Mean bias ranged from − 10.6 to 3.6% of the mean. Figure 3 shows the linear relationships between fRTs and GETs. Correlation magnitudes ranged from moderate to very large and precision in estimation of GETs from fRTs ranged from acceptable to very poor. Figure 4 summarizes the interpretation of the correlation magnitudes and the precision in predicting GETs from fRTs in the entire group of participants.
Agreement plots between gas exchange thresholds (GETs) and respiratory frequency thresholds (fRTs) for oxygen uptake (upper panel), heart rate (middle panel) and power output (lower panel). GET1 vs. fRT1: left panel. GET2 vs. fRT2: right panel. Open circles: DS group (participants with chronic illnesses). Filled circles: HS group (healthy participants). Solid lines: mean bias. Dashed lines: limits of agreements
Individual data-points and linear regression analyses between respiratory frequency thresholds (fRTs) and gas exchange thresholds (GETs) for oxygen uptake (upper panel), heart rate (middle panel) and power output (lower panel). fRT1 vs. GET1: left panel. fRT2 vs. GET2: right panel. Solid lines: linear regression lines for the entire group of participants. Dashed lines: 95% confidence intervals. Open circles: DS group (participants with chronic illnesses). Filled circles: HS group (healthy participants). r Pearson’s product-moment correlation coefficient, SEE standard error of the estimates
Summary of correlation coefficients (upper panel) and standard error of the estimates (lower panel) of oxygen uptake (\(\dot{V}\)o2), heart rate (HR) and power output (PO), in predicting gas exchange thresholds (GETs) from respiratory frequency thresholds (fRTs). Error bars: upper and lower 95% confidence intervals (CIs). Dashed lines: interpretation thresholds
Discussion
The main findings of this study were as follows: first, the external power output (PO) and \(\dot{V}\)o2 levels at fRT1 exhibited very poor and moderate levels of agreement and precision in predicting the corresponding measures at GET1. The precision of fRT1 in predicting HR at GET1 was acceptable. Second, agreement and precision in predicting GET2 from fRT2 (moderate to acceptable) was superior to that of GET1 from fRT1. These results suggest that fRT1 and fRT2 can be used as viable alternatives to traditional ventilatory and gas exchange-based measurements to estimate the exercise intensity associated with GET1 and GET2, in both healthy middle-aged individuals and those with chronic illnesses. Thus, fRTs are proposed as an appealing and cost-effective method for objectively determining exercise-intensity thresholds in field settings.
Oxygen uptake (\(\dot{V}\)o2) and heart rate (HR) at the first gas exchange (GET1) and respiratory frequency (fRT1) thresholds
Absolute \(\dot{V}\)o2 at GET1, measured by the V-slope method, was found to be 20% higher in HS compared to DS and it occurred at ~ 57% of \(\dot{V}\)o2peak. This is consistent with the average \(\dot{V}\)o2peak percentages reported in previous studies using traditional or modified V-slope methods to determine \(\dot{V}\)o2 at GET1 in healthy young (Beaver et al. 1986; Davis et al. 1997; Ozcelik et al. 1999), middle-aged (Davis et al. 1997) and elderly (Davis et al. 1997) males, with average \(\dot{V}\)o2peak values (ranging from 30 to 41 mL·Kg−1·min−1) similar to those of our participants. In the present study, GET1 was not detected in 14% of the participants, a finding consistent with previous studies on middle-aged men (Meyer et al. 1996; Sue et al. 1988). This indicates that a considerable proportion of middle-aged individuals will experience undetectable or unreliable determination of GET1 when utilizing the V-slope method.
Absolute \(\dot{V}\)o2 values at GET1 did not differ from those at fRT1, and were very largely correlated with each other (r = 0.75). Nevertheless, the agreement and precision in the estimation of \(\dot{V}\)o2 at GET1 from fRT1 was moderate, as indicated by the relative SEE and LOAs that were 15% and 33%, respectively. These values compare favorably with SEE values of 27% found in young triathletes (average \(\dot{V}\)o2max: 68 mL·Kg−1·min−1) for whom GET1 and fRT1 were measured by least-squares errors (Carey et al. 2009). However, they compare unfavorably with SEE values of ~ 9% (Cannon et al. 2009) and 12% (Cross et al. 2012), and LOAs of 17% (Cannon et al. 2009) and 20% (Cross et al. 2012) found in the only two published articles conducted in young men (average \(\dot{V}\)o2max: 53–57 mL·Kg−1·min−1) using a rigorous methodology very similar to that used in our present study (1-min stage duration, objective GETs and fRTs determinations, detection of four thresholds, regression and agreement analyses including SEE, mean bias and LOAs). However, one major limitation of these two studies is that 42% (Cannon et al. 2009) and 50% (Cross et al. 2012) of participants had one or more of the four thresholds labeled as “undetermined”. In comparison, in our study, the four thresholds were obtained in 86% of the participants and the two fRTs were obtained in 98% of the participants (49/50). Collectively, these results suggest that using \(\dot{V}\)o2 measurements at fRT1 to estimate V̇o2 at GET1, as found in our study, may potentially be unacceptable in practice due to the observed prediction and agreement errors and the significant proportion of “undetermined” thresholds. Interestingly, the infrequently used HR at fRT1 showed no differences compared to HR at GET1. In agreement with others (Neder & Stein 2006; Weston & Gabbett 2001) occurred on at ~ 75% of HRmax, and was a good predictor of the HR at GET1, based on the very large correlation (r = 0.79), and acceptable SEE (8%) and LOAs (16%). The better accuracy in estimating HR at GET1 from HR at fRT1 than that observed with \(\dot{V}\)o2 may be partly attributed to the lower influence of subjective factors, like motivation or anxiety, on HR in comparison to respiration. It is suggested that HR rather than \(\dot{V}\)o2 at fRT1 may potentially be an acceptable estimator of GET1.
Oxygen uptake (\(\dot{V}\)o2) and heart rate (HR) at the second gas exchange (GET2) and respiratory frequency (fRT2) thresholds
In this study, the absolute \(\dot{V}\)o2 at GET2 was found to be 16% higher in HS than in DS, was determined in 92% of the participants and occurred at ~ 78% \(\dot{V}\)o2peak. This is consistent with average GET2 values occurring at 75–80% \(\dot{V}\)o2max found in the original study presenting the “V-slope” method (Beaver et al. 1986), and in many studies conducted on individuals with comparable \(\dot{V}\)o2max values to those of this study (Keir et al. 2015).
Absolute \(\dot{V}\)o2 at fRT2 did not differ from \(\dot{V}\)o2 at GET2, and both variables were very largely (r = 0.82) correlated. Moreover, SEE (9%) and LOAs (19%) indicated that the relative precision of estimation and agreement was acceptable. This precision is similar to that found when GET2 was estimated using the near-infrared spectroscopy-derived muscle deoxyhemoglobin break point (deoxy-BP) (Keir et al. 2015), but compares unfavorably with respect to the narrower LOAs of 7% reported in the above-mentioned two studies conducted on young men (Cannon et al. 2009; Cross et al. 2012). However, as above mentioned, both of these studies reported a very high percentage of “undetermined” thresholds, challenging their practical application. Similar to fRT1 and GET1, the seldom-used HR at fRT2 did not differ from the HR at GET2. In agreement with prior studies (Neder and Stein 2006), HR at fRT2 typically occurred at ~ 87% of HRmax, and proved to be a good predictor of HR at GET2. This is evidenced by the very large correlation coefficient (r = 0.75), accounting for 56% of the variance, and acceptable SEE (6.6%) and LOAs (13%). Thus, \(\dot{V}\)o2 and HR at fRT2 may serve as acceptable predictors of \(\dot{V}\)o2 and HR at GET2.
Power output (PO) at the gas exchange (GETs) and respiratory frequency (fRTs) thresholds
The PO associated with both fRTs did not differ from the PO calculated at their corresponding GETs. However, the precision of the estimation and the agreement were very poor for GET1 (SEE: 23%; LOAs: 52%) and better, but moderate, for GET2 (SEE: 12%; LOAs: 25%). These precision values of PO are lower compared to those of \(\dot{V}\)o2 and HR. This may be partly due to the considerably lower test–retest reliability of PO at GETs, compared to that of \(\dot{V}\)o2 or HR, as previously reported (Weston and Gabbett 2001). The imprecise PO estimations of GETs from fRT1 and fRT2 hinder its practical use because it may lead to distorted conclusions.
Better precision and agreement at the second than at the first threshold
The precision of estimations for HR, \(\dot{V}\)o2 and PO at GET2, determined from the corresponding values at fRT2, was considerably better than for these variables at GET1 (Fig. 4). This may partly be attributed to: (1) the considerable better test–retest reliability of HR, \(\dot{V}\)o2 and PO at GET2 in comparison with GET1 (Weston & Gabbett 2001), (2) the more pronounced deflection in the respiratory response to incremental exercise occurring at GET2 in comparison to GET1 (Beaver et al. 1986), and (3) the higher proportional contribution of the non-metabolic stressors (such as emotional stress, pain, cognitive load, dyspnea, irregular breathing patterns and heat stimuli) to the changes in fR that predominate below and near GET1, but become less prominent at GET2 (Nicolo et al. 2020).
Limitations
First, we decided that the provisional fRT1 should occur after completing the 60 W stage, that is, after four minutes of the start of the incremental exercise test. Restricting the initial minutes of exercise was already an essential condition in the original V-slope method proposed by Beaver et al. (1986) and has been subsequently used (Keir et al. 2022). These restrictions ensure that the computer model follows the major trend in the data and is not notably influenced by the minor spontaneous hyperventilation frequently seen at the onset of exercise.
Second, the V-slope method of Beaver et al. (1986) is the most widely cited (Hagberg 2022) computerized procedure for detecting GETs and it is considered by many as the reference technique for measuring these gas exchange thresholds (Kang et al. 2014). However, this method is not without methodological issues. For instance, in the original paper (Beaver et al. 1986) the authors acknowledged that the CO2 production data, which are essential to determine GETs, were too low and inaccurate, and had to be arbitrarily corrected for fluctuations in end-tidal PCO2 (Henritze et al. 1985). In addition, the gas exchange data were analyzed by six experts (Beaver et al. 1986). They used a subjective visual identification as the criterion standard measure but all six experts could only grade up to 50% of the small sample (n = 10) of participants studied, and only one of the six experts was able to detect the GET1 in all participants. Despite its widespread acceptance, these methodological problems and weaknesses identified in the original article raise serious doubts and concerns about the suitability of the V-slope method as a valid reference technique for determining GET1 and GET2.
The third limitation concerns the applicability of HR data obtained from incremental tests to prescribe constant load exercise training. During incremental maximal exercise, it is known that the \(\dot{V}\)o2 at GET1 and GET2 remains constant regardless of the protocol used (Davis et al. 1982). However, the PO at which GETs occur differs depending on the rate of PO increase during the test. Indeed, the value of the PO at a given GET is higher when the ramp is steeper (or the duration of the test is shorter) (Davis et al. 1982; Iannetta et al. 2019b). As a result, incremental exercise overestimates the constant power required to elicit the \(\dot{V}\)o2 at the GETs by an average of 1.2–1.5 workload stages at GET1, and approximately 2 workload stages at GET2 (Caen et al. 2020; Iannetta et al. 2019b). The overestimation can be corrected by shifting the \(\dot{V}\)o2 data to the left, based on the individual \(\dot{V}\)o2 mean response time for ramp-incremental exercise (i.e. the lag time between the onset of the ramp and the increase in the \(\dot{V}\)o2 response), as well as the appearance of the \(\dot{V}\)o2 slow component (Caen et al. 2020; Iannetta et al. 2019a, b; Keir et al. 2016). Although it has received less attention, the same issue is present with HR (a lower PO during constant-load exercise compared to incremental testing at a given HR value) (Zuccarelli et al. 2018). Additionally, during constant-load exercise, there is a disproportionate increase in HR over time across all exercise domains once the target HR value is reached after approximately 3–5 min (Teso et al. 2022; Zuccarelli et al. 2018). The relative amplitude of the increase, known as the “slow component” or “cardiovascular drift”, is greater for HR kinetics than for \(\dot{V}\)o2 kinetics (Teso et al. 2022; Zuccarelli et al. 2018). This indicates that the concept of a single HR value corresponding to a specific exercise of constant load exercise carried out for periods longer than a few minutes is not straightforward (Zuccarelli et al. 2018). HR targets should be adjusted over time to ensure that the desired stimulus is maintained throughout the constant-load exercise session (Teso et al. 2022). Additional research is required to determine the appropriate conversion of HR values from incremental exercise to constant-load exercise.
Conclusion
This preliminary study, conducted with a sizable sample of middle-aged men, suggests that HR at fRT1 and \(\dot{V}\)o2 and HR at fRT2, determined by a novel and objective approach, are potentially acceptable estimators of the corresponding variables at GETs. This alternative may serve as simplified low-cost and field-based approach to estimate GETs during graded exercise. Further research is needed to validate fRTs against commonly accepted markers of exercise intensity boundaries, such as the Lactate Thresholds (LTs). Additionally, more research is required to determine the appropriate conversion of heart rate values from incremental exercise to constant-load exercise. This is required to help clarifying the precision of fRTs for determination of either GETs or LTs in other populations or modes of exercise.
Data availability
Data are available on reasonable request from the corresponding author.
Code availability
Not applicable.
Abbreviations
- CIs:
-
Confidence intervals
- deoxy-BP:
-
Near-infrared spectroscopy-derived muscle deoxyhemoglobin break point
- DS:
-
Group of males with chronic illnesses
- ES:
-
Hedges’ g effect sizes
- fR :
-
Respiratory frequency
- fRi :
-
Respiratory frequency for specific exercise stage
- fRT1:
-
Respiratory frequency threshold 1
- fRT2:
-
Respiratory frequency threshold 2
- fRTs:
-
Respiratory frequency thresholds
- GET:
-
Gas exchange thresholds
- GET1:
-
First gas exchange threshold
- GET2:
-
Second gas exchange threshold
- HR:
-
Heart rate
- HRma :
-
Maximal heart rate
- HS:
-
Group of healthy males
- i:
-
Specific exercise stage
- LOAs:
-
Limits of agreement
- LTs:
-
Lactate thresholds
- PETCO2 :
-
End-tidal carbon dioxide expiration
- PETO2 :
-
End-tidal oxygen expiration
- PO:
-
Power output
- RER:
-
Respiratory exchange ratio
- RLs:
-
Regression lines
- SD:
-
Standard deviation
- SEEs:
-
Standard errors of the estimates
- \(\dot{V}\)co2 :
-
Carbon dioxide output
- \(\dot{V}\) E :
-
Minute ventilation
- \(\dot{V}\) E/\(\dot{V}\)co2 :
-
Ventilatory equivalent for CO2
- \(\dot{V}\) E/\(\dot{V}\)o2 :
-
Ventilatory equivalent for O2
- \(\dot{V}\)o2 :
-
Oxygen uptake
- \(\dot{V}\)o2max/\(\dot{V}\)o2peak :
-
Maximal oxygen uptake
- Vt :
-
Tidal volume
- Wmax :
-
Maximal workload
References
American College of Sports Medicine (2014) ACSM’s Guidelines for exercise testing and prescriptions, 9th edn. Lippincott Williams & Wilkins
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60(6):2020–2027. https://doi.org/10.1152/jappl.1986.60.6.2020
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Caen K, Boone J, Bourgois JG, Colosio AL, Pogliaghi S (2020) Translating ramp VO2 into constant power output: a novel strategy that minds the gap. Med Sci Sports Exerc 52(9):2020–2028. https://doi.org/10.1249/MSS.0000000000002328
Cannon DT, Kolkhorst FW, Buono MJ (2009) On the determination of ventilatory threshold and respiratory compensation point via respiratory frequency. Int J Sports Med 30(3):157–162. https://doi.org/10.1055/s-0028-1104569
Carey DG, Schwarz LA, Pliego GJ, Raymond RL (2005) Respiratory rate is a valid and reliable marker for the anaerobic threshold: implications for measuring change in fitness. J Sports Sci Med 4(4):482–488
Carey DG, Tofte C, Pliego GJ, Raymond RL (2009) Transferability of running and cycling training zones in triathletes: implications for steady-state exercise. J Strength Cond Res 23(1):251–258. https://doi.org/10.1519/JSC.0b013e31818767e7
Cheng B, Kuipers H, Snyder AC, Keizer HA, Jeukendrup A, Hesselink M (1992) A new approach for the determination of ventilatory and lactate thresholds. Int J Sports Med 13(7):518–522. https://doi.org/10.1055/s-2007-1021309
Cross TJ, Morris NR, Schneider DA, Sabapathy S (2012) Evidence of break-points in breathing pattern at the gas-exchange thresholds during incremental cycling in young, healthy subjects. Eur J Appl Physiol 112(3):1067–1076. https://doi.org/10.1007/s00421-011-2055-4
Crouter SE, Antczak A, Hudak JR, DellaValle DM, Haas JD (2006) Accuracy and reliability of the ParvoMedics TrueOne 2400 and MedGraphics VO2000 metabolic systems. Eur J Appl Physiol 98(2):139–151. https://doi.org/10.1007/s00421-006-0255-0
Davis JA, Whipp BJ, Lamarra N, Huntsman DJ, Frank MH, Wasserman K (1982) Effect of ramp slope on determination of aerobic parameters from the ramp exercise test. Med Sci Sports Exerc 14(5):339–343
Davis JA, Storer TW, Caiozzo VJ (1997) Prediction of normal values for lactate threshold estimated by gas exchange in men and women. Eur J Appl Physiol Occup Physiol 76(2):157–164. https://doi.org/10.1007/s004210050228
Garcia-Tabar I, Eclache JP, Aramendi JF, Gorostiaga EM (2015) Gas analyzer’s drift leads to systematic error in maximal oxygen uptake and maximal respiratory exchange ratio determination. Front Physiol 6:308. https://doi.org/10.3389/fphys.2015.00308
Hagberg J (2022) A personal biography of a physiological misnomer: the anaerobic threshold. Int J Sports Med 43(5):391–400. https://doi.org/10.1055/a-1664-8854
Hedges LV (1981) Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Stat 6:107–128
Henritze J, Weltman A, Schurrer RL, Barlow K (1985) Effects of training at and above the lactate threshold on the lactate threshold and maximal oxygen uptake. Eur J Appl Physiol Occup Physiol 54(1):84–88. https://doi.org/10.1007/BF00426304
Hopkins WG, Marshall SW, Batterham AM, Hanin J (2009) Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc 41(1):3–13. https://doi.org/10.1249/MSS.0b013e31818cb278
Iannetta D, Azevedo RA, Keir DA, Murias JM (2019a) Establishing the VO2 versus constant-work rate relationship from ramp-incremental exercise: simple strategies for an unsolved problem. J Appl Physiol 127(6):1519–1527. https://doi.org/10.1152/japplphysiol.00508.2019
Iannetta D, Murias JM, Keir DA (2019b) A simple method to quantify the VO2 mean response time of ramp-incremental exercise. Med Sci Sports Exerc 51(5):1080–1086. https://doi.org/10.1249/MSS.0000000000001880
James NW, Adams GM, Wilson AF (1989) Determination of anaerobic threshold by ventilatory frequency. Int J Sports Med 10(3):192–196. https://doi.org/10.1055/s-2007-1024899
Kang S, Kim J, Kwon M, Eom H (2014) Objectivity and validity of EMG method in estimating anaerobic threshold. Int J Sports Med 35(9):737–742. https://doi.org/10.1055/s-0033-1361182
Keir DA, Fontana FY, Robertson TC, Murias JM, Paterson DH, Kowalchuk JM, Pogliaghi S (2015) Exercise intensity thresholds: identifying the boundaries of sustainable performance. Med Sci Sports Exerc 47(9):1932–1940. https://doi.org/10.1249/MSS.0000000000000613
Keir DA, Copithorne DB, Hodgson MD, Pogliaghi S, Rice CL, Kowalchuk JM (2016) The slow component of pulmonary O2 uptake accompanies peripheral muscle fatigue during high-intensity exercise. J Appl Physiol 121(2):493–502. https://doi.org/10.1152/japplphysiol.00249.2016
Keir DA, Iannetta D, Mattioni Maturana F, Kowalchuk JM, Murias JM (2022) Identification of non-invasive exercise thresholds: methods, strategies, and an online app. Sports Med 52(2):237–255. https://doi.org/10.1007/s40279-021-01581-z
Martin BJ, Weil JV (1979) CO2 and exercise tidal volume. J Appl Physiol Respir Environ Exerc Physiol 46(2):322–325. https://doi.org/10.1152/jappl.1979.46.2.322
Meyer K, Hajric R, Westbrook S, Samek L, Lehmann M, Schwaibold M, Betz P, Roskamm H (1996) Ventilatory and lactate threshold determinations in healthy normals and cardiac patients: methodological problems. Eur J Appl Physiol Occup Physiol 72(5–6):387–393. https://doi.org/10.1007/BF00242266
Meyer T, Lucia A, Earnest CP, Kindermann W (2005) A conceptual framework for performance diagnosis and training prescription from submaximal gas exchange parameters–theory and application. Int J Sports Med 26(Suppl 1):38. https://doi.org/10.1055/s-2004-830514
Nabetani T, Ueda T, Teramoto K (2002) Measurement of ventilatory threshold by respiratory frequency. Percept Mot Skills 94(3 Pt 1):851–859. https://doi.org/10.2466/pms.2002.94.3.851
Neary JP, Bhambhani YN, Quinney HA (1995) Validity of breathing frequency to monitor exercise intensity in trained cyclists. Int J Sports Med 16(4):255–259. https://doi.org/10.1055/s-2007-973001
Neder JA, Stein R (2006) A simplified strategy for the estimation of the exercise ventilatory thresholds. Med Sci Sports Exerc 38(5):1007–1013. https://doi.org/10.1249/01.mss.0000218141.90442.6c
Nicolo A, Massaroni C, Schena E, Sacchetti M (2020) The importance of respiratory rate monitoring: from healthcare to sport and exercise. Sensors (basel) 20(21):6396. https://doi.org/10.3390/s20216396
Ozcelik O, Ward SA, Whipp BJ (1999) Effect of altered body CO2 stores on pulmonary gas exchange dynamics during incremental exercise in humans. Exp Physiol 84(5):999–1011. https://doi.org/10.1111/j.1469-445x.1999.01868.x
Powers SK, Dodd S, Garner R (1984) Precision of ventilatory and gas exchange alterations as a predictor of the anaerobic threshold. Eur J Appl Physiol Occup Physiol 52(2):173–177. https://doi.org/10.1007/BF00433388
Shimizu M, Myers J, Buchanan N, Walsh D, Kraemer M, McAuley P, Froelicher VF (1991) The ventilatory threshold: method, protocol, and evaluator agreement. Am Heart J 122(2):509–516. https://doi.org/10.1016/0002-8703(91)91009-c
Sue DY, Wasserman K, Moricca RB, Casaburi R (1988) Metabolic acidosis during exercise in patients with chronic obstructive pulmonary disease. Use of the V-slope method for anaerobic threshold determination. Chest 94(5):931–938. https://doi.org/10.1378/chest.94.5.931
Teso M, Colosio AL, Pogliaghi S (2022) An intensity-dependent slow component of HR interferes with accurate exercise implementation in postmenopausal women. Med Sci Sports Exerc 54(4):655–664. https://doi.org/10.1249/MSS.0000000000002835
Ward SA (2018) Reply to Garcia-Tabar et al.: Quality control of open-circuit respirometry: real-time, laboratory-based systems. Let us spread “good practice.” Eur J Appl Physiol 118(12):2721–2722. https://doi.org/10.1007/s00421-018-3991-z
Wasserman K, Whipp BJ, Koyl SN, Beaver WL (1973) Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 35(2):236–243. https://doi.org/10.1152/jappl.1973.35.2.236
Weston SB, Gabbett TJ (2001) Reproducibility of ventilation of thresholds in trained cyclists during ramp cycle exercise. J Sci Med Sport 4(3):357–366. https://doi.org/10.1016/s1440-2440(01)80044-x
Whipp BJ, Davis JA, Wasserman K (1989) Ventilatory control of the ‘isocapnic buffering’ region in rapidly-incremental exercise. Respir Physiol 76(3):357–367. https://doi.org/10.1016/0034-5687(89)90076-5
Zuccarelli L, Porcelli S, Rasica L, Marzorati M, Grassi B (2018) Comparison between slow components of HR and VO2 kinetics: functional significance. Med Sci Sports Exerc 50(8):1649–1657. https://doi.org/10.1249/MSS.0000000000001612
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
Conception and design of research: JPE and EMG; conducted experiments: JPE; analyzed data JPE, IGT and EMG; formal analysis of data: IGT; interpretation of data: JPE, IGT and EMG; writing of the original draft: JPE, IGT and EMG; review and editing of manuscript: JPE, IGT and EMG. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest, financial or otherwise, are declared by the authors.
Ethical approval
Ethical approval for this study was obtained from the Institutional Review Board of the University. The study was conducted conformed to the Declaration of Helsinki and Tokyo.
Consent to participate and publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Guido Ferretti.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eclache, J.P., Garcia-Tabar, I. & Gorostiaga, E.M. A new objective method for determining exercise gas exchange thresholds by respiratory frequency in middle-aged men. Eur J Appl Physiol (2024). https://doi.org/10.1007/s00421-024-05520-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00421-024-05520-4