Abstract
Purpose
To compare external and internal training load markers during resistance training (RT) in normoxia (N), intermittent hypobaric hypoxia (HH), and intermittent normobaric hypoxia (NH).
Methods
Thirty-three volunteers were assigned an 8-week RT program in either N (690 m, n = 10), HH (2320 m, n = 10), or NH (inspired fraction of oxygen = 15.9%; ~ 2320 m, n = 13). The RT program (3x/week) consisted of six exercises, with three sets of six to 12 repetitions at ~ 70% of one repetition maximum (1RM) with the first session of each week used for analysis. 1RM in back squat and bench press was used to evaluate muscle strength before and after the program. External load was assessed by the volume load relative to body mass (RVL, kg·kg−1). Internal load was assessed by the ratings of perceived exertion (RPE) and heart rate (HR).
Results
Smaller relative improvements were found for the back squat in the N group (11.5 ± 8.8%) when compared to the NH group (22.2 ± 8.2%, P = 0.01) and the HH group (22 ± 8.1%, P = 0.02). All groups showed similar RVL, HR responses and RPE across the program (P˃0.05). However, reduced HR recovery values, calculated as the difference between the highest HR value (HRpeak) and the resting heart rate after a two min rest, were seen in the N and NH groups across the program (P \(<\) 0.05).
Conclusion
It seems that 8 weeks of intermittent RT in hypoxic environments could maximize time-efficiency when aiming to improve strength levels in back squat without evoking higher levels of physiological stress. Performing RT at hypobaric hypoxia may improve the cardiorespiratory response, which in turn could speed recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Altitude training is widely used by coaches and athletes to complement normal training at sea level. Applied to strength, studies have shown how hypertrophy resistance training (RT) under moderate hypoxic conditions promote the mechanisms related to maximal strength and muscle mass development (Kurobe et al. 2015; Kon et al. 2010). The alternatives to performing RT under moderate hypoxic conditions are numerous and will depend on the combination of the dosage of hypoxia (chronic vs. intermittent) and the type of hypoxia (hypobaric hypoxia [HH] or real altitude vs. normobaric hypoxia [NH]). Regarding dosage, intermittent exposure, such as “living low—training high”, seems to be more advantageous than permanent exposure. It has been observed that permanent exposure can lead to a reduction in muscle cross-sectional area and a decrease in the size of muscle fibers in humans (Narici and Kayser 1995). It can also result in increased neuromuscular fatigue during exercise by impairing neuromuscular transmission during contractions (Amann et al. 2006), and by decreasing the muscle fibers’ capacity for relaxation (Allen et al. 2008). Regarding the types of hypoxia: HH can be achieved by ascending to a real moderate altitude, while NH can be achieved by reducing the oxygen pressure in the inspired air (nitrogen dilution or oxygen filtration). For economical and logistical reasons, NH is often used as a laboratory alternative to HH, because athletes do not have to ascend to a higher altitude nor spend time acclimating. Alternative techniques can also be employed to trigger a hypoxic response in muscles. Applying pressure to the blood vessels near the skeletal muscles leads to insufficient oxygen delivery (hypoxia) to the muscle tissue (Patterson et al. 2019). Instead of decreasing atmospheric oxygen globally, hypoxia can be localized by exerting external pressure on the limbs, causing partial restriction of blood flow, a method known as blood flow restriction.
The efficiency, safety, and effectiveness of RT training programs are paramount for sport conditioning. Coaches try to identify the optimal doses of the training load (product of exercise intensity and volume) since, if it is insufficient, adaptation might not occur, while excessive stress might impair performance and potentially increase the risk of injury (Halson 2014). For this reason, it becomes really important to monitor parameters of both internal (i.e., the athlete’s individual responses, such as heart rate [HR] and ratings of perceived exertion [RPE]) and external (i.e., the total volume of load lifted: sets × reps × kg) loads to quantify the training stress and hence estimate the training efficacy (McLaren et al. 2017). When evaluating the response to training stress, internal load provides a more precise and individualized measurement compared to external load. However, factors such as training status, nutrition, health, psychological status, environment (e.g., altitude, temperature) and genetics may lead to variation in their internal load when providing the same external load (Impellizzeri et al. 2018). The optimal dose of training intensity for RT under hypoxic conditions may differ, as the environmental condition per se seems to be physiologically more demanding than at sea level (Rodríguez-Zamora et al. 2019). In addition, when comparing the hypoxic conditions (HH vs. NH), it has been reported that HH represents a more severe physiological stimulus than NH at the same theoretical altitude (Millet and Debevec 2020; Timon et al. 2022). Thus, the quantification of the training load could be distinct depending on the RT environment.
Ratings of perceived exertion and HR monitoring have been widely used to verify the internal load in athletes. While RPE seems to be a valid surrogate measure of the internal load in RT (McGuigan et al. 2004; Sweet et al. 2004), the use of HR monitoring as a direct indicator is scarce (Apkarian 2019; Moreira et al. 2017). Heart rate monitoring during RT serves as a practical and cost-effective method to gauge the physiological response to exercise. It provides real-time insights into the cardiovascular demands of RT, aiding in the assessment of internal training load (de Beukelaar and Mantini 2023). Research suggests that HR can serve as a reliable indicator of exercise intensity and metabolic stress during RT sessions (de Beukelaar and Mantini 2023). This approach offers a non-invasive means to monitor, and tailor individualized training programs, enhancing both safety and effectiveness. However, it is essential to consider individual variations and factors influencing HR response to ensure accurate interpretation in the context of RT (Scott et al. 2017).
RT involves a blend of static and dynamic contractions that elicits hemodynamic responses (Apkarian 2019; Hill and Butler 1991). When parasympathetic activity is decreased and sympathetic activity increased there is tachycardia and increased cardiac output, increased total peripheric resistance, as well as an increase in both systolic and diastolic blood pressures (Hill and Butler 1991). However, the magnitude of this response may be affected by several factors such as the exercise load, movement velocity, rest interval duration, muscle mass involved, exercise duration, age, training status and altitude exposure (Apkarian 2019; Mourot 2018).
Unfortunately, to date, there are no longitudinal investigations comparing training load markers during intermittent hypoxic RT in normobaric vs. hypobaric hypoxia with the equivalent training in normoxia. Therefore, we aimed to compare external and internal training load markers during an 8-week RT program in normoxia, intermittent normobaric hypoxia, and intermittent hypobaric hypoxia. We hypothesized that: 1) the two hypoxic groups (HH and NH) will lift higher loads across the RT program compared to normoxia; and 2) real moderate altitude would lead to higher psychophysiological stress (HR and RPE) values when compared to the other two conditions.
Methods
Participants
Thirty-three physically trained Sport Science students familiarized with the RT exercises employed volunteered to participate in the study. The mean ± SD of age, training experience, height, body mass, BMI, fat mass, and fat free mass were: 22.4 ± 3.2 years, 2.9 ± 1.8 years, 176.5 ± 6.5 cm, 73.8 ± 10.1 kg, 23.7 ± 2.8 kg∙m−2, 8.1 ± 4.2 kg, and 65.7 ± 6.8 kg, respectively. To be included, volunteers could have no self-reported health issues or muscle injuries and not have been exposed to more than three to four consecutive days of altitudes higher than 1500 m above sea level (MASL) for at least 2 months before the study. Participants were provided with information on the research protocol, and they provided signed informed consent. This study was approved by the local Ethics Committee (PEIBA/2018) and was conducted in accordance with the Declaration of Helsinki.
Design
A longitudinal quasi-experimental design was employed to compare changes in the relative volume load (RVL), ratings of perceived exertion (RPE, a.u), and the heart rate (HR, bpm) response during an 8-week RT program. Participants were grouped according to the following conditions: living and training in normoxia (N; 690 m; n = 10); living in normoxia and training at moderate altitude (HH; 2.320 m; n = 10); and living in normoxia and training at normobaric hypoxia (NH; inspired fraction of oxygen [FiO2] = 15.9%; ~ 2320 m; n = 13). The characteristics of each group are shown in Table 1. To see the effect of the RT program on one repetition maximum (RM) in the three conditions, we compared the relative one RM values when executing back squat and bench press exercises before and after the program in normoxic conditions (PiO2 = 149 mmHg). The training program comprised three RT sessions·week−1 (24 in total) at the same time of day with two additional weeks allocated for pre- and post-muscular strength and anthropometric assessments. The first session of each week (Mondays = control session) was used for the analysis. Both the N and NH groups trained at the faculty laboratory (below 700 MASL), while the HH group conducted the training sessions at the High-Performance Center in Sierra Nevada, Granada, Spain (2320 MASL). All volunteers took part in a pre-intervention 2-week conditioning-training program. To ensure the essential amino acids intake for performance during the training periods subjects were provided with a standard protein shake after each training session. To minimize the potential for instruction bias, the researchers remained the same for all the groups. Participants were instructed to abstain from intense exercise and alcohol intake, and to maintain their customary sleep and diet habits during the study.
Methodology
The normobaric hypoxic condition
The NH condition was created in a normobaric tent (CAT 430, Colorado Altitude Training, USA), where oxygen-depleted air was pumped from a hypoxic generator with a semi-permeable filtration membrane (nitrogen filter technique; CAT 310, Louisville, Colorado, USA) to simulate hypoxic conditions (FiO2 = 15.9%, equivalent to 2320 MASL). Barometric pressure in the tent was equivalent to that of University of Granada campus (704 mmHg). Ambient O2 was continuously monitored by a digital controller (Handi + , Maxtec, USA) to maintain the hypoxic conditions in the tent. Immediately before and after each first RT session of the week, arterial oxygen saturation (SpO2) was measured per duplicate using a pulse oximeter (Wristox 3100; Nonin, Plymouth, MN, USA).
The training session
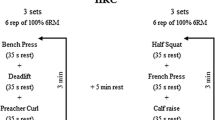
Each RT session encompassed ~ 15 min of warm-up and the execution of six exercises, with three sets of six to 12 repetitions at 65–80% of 1RM with 90 s of rest between sets and exercises (Fig. 1) to promote muscle growth (Kraemer et al. 1991). During the recovery, participants were asked to sit for 2 min. The lifted load was individually adjusted in every session so the participants could perform ± 2 rep. If a participant could perform ± 3 reps, the training load was adjusted by ± 5% accordingly (Kraemer et al. 2009). All the training sessions were supervised by experts to guarantee proper technique and safe execution. Because volume load is largely related to measures of internal load and physiological stress during resistance exercise at various intensities (Genner and Weston 2014), the relative volume load (RVL, kg·kg−1) as well as its percentage of change (ΔRVL) were calculated for every RT session and were considered for further analysis. (Relative volume load was calculated as a product of the total number of repetitions performed and the amount of mass lifted divided per body weight; ΔRVL was defined as the difference in RVL between session one and sessions two to eight, expressed in %).
Strength performance
One RM was estimated for each of the six main exercises of the training program (back squat, bench press, deadlift, pulldown prone grip, barbell row, and shoulder press) using a progressive trial and error procedure (Brown and Weir 2001). Three sets of three to six repetitions at increasing loads were completed before performing one set of two to three repetitions to failure. Rest periods between sets were kept to 5 min. Using the two–three RM load, one RM values were predicted using Brzycki’s equation (Brzycki 1993). After the RT program, subjects repeated the same procedure for the back squat and the bench press for upper- and lower-body comparison. These exercises, back squat and bench press, were selected due to differences in training machine models between locations for the deadlift, pulldown prone grip, barbell row, and shoulder press. Relative one RM (kg·kg−1 of body weight) as its percentage of change (Δ%) in back squat and bench press were considered for further analysis.
Body composition
A segmental multi-frequency bioimpedance analyzer (Tanita BC 418 segmental, Tokyo, Japan) was used to assess weight and body composition, and height was measured by a height rod (Seca 202, Seca Ltd., Hamburg, Germany).
Oxygen saturation
Immediately before and after each control session, peripheral arterial oxygen saturation (SpO2) was measured per duplicate using a pulse oximeter fingertip sensor (Wristox 3100; Nonin, Plymouth, MN, USA).
Heart rate
Heart rate (HR) was continuously recorded beat-by-beat by a Polar Memory Belt HR monitor (Polar, Vantaa, Finland) and a Polar M430 watch (Polar Electro Oy, Kempele, Finland). The belt was placed on the participant’s chest ten min before the HT session and removed after the recovery assessment. To minimize potential instrumentation bias, participants wore the HR monitor during the pre-intervention period. Then, data were transferred to the software Polar Flow Sync 3 (version for Windows) and exported to an Excel file. Pre-exercise HR (HRpre) was the average HR for the minute immediately before the start of the RT session; HRpeak and HRmin were the highest and lowest HR values during the RT session, while HRmean was the arithmetic mean for RT session. The value for heart rate recovery (HRR) was calculated as the difference between HRpeak and the resting heart rate after a 1 min rest (HRR1) and two min rest (HRR2) (Cole et al. 2000, 1999).
Ratings of perceived exertion
Rating of perceived exertion (RPE) was assessed after the RT session using the Borg CR-10 scale (Noble et al. 1983). To ensure the quality of the data collected, all subjects used the CR-10 scale on three different occasions 1 week prior to starting the training program (Psycharakis 2011).
Statistical analysis
Data were presented as means and standard deviations (± SD) unless otherwise indicated. Differences in relative and absolute RM for each exercise (back squat and bench press) were assessed using two-way mixed ANOVA, with one between-subject factor (condition: N vs. NH vs. HH) and one within-subject factor (time: pre–post-RT program) and interaction terms (condition x time). Differences in Δ% were assessed using a one-way ANOVA, with one between-subject factor (condition: N vs. NH vs. HH). Differences in HR parameters, RVL, and ΔRVL were assessed using a two-way mixed ANOVA, with one between-subject factor (condition: N vs. NH vs. HH) and one within-subject factor (session: from one to eight) and interaction terms (condition x session). A three-factor mixed model ANOVA with a between-subject factor (N vs. NH vs. HH) and two within-subject factors ([session: from 1 to 8] and time [pre–post-training session]) were applied on SpO2. Post hoc comparisons, when justified, were performed using Bonferroni correction for multiple pairwise comparisons. Partial eta squared from the ANOVA (η2p) was interpreted using the following classification: 0.02 (small), 0.13 (medium), and 0.26 (large) (Bakeman 2005). A two-tailed Pearson product moment correlation coefficient (r) was used to look for relationships among RVL and HR parameters during the session. The following scales were used to interpret the magnitude of the correlations: < 0.1 trivial, 0.1–0.3 small, 0.31–0.5 moderate, 0.51–0.7 large, 0.71–0.9 very large, > 0.9 nearly perfect (Cohen 1988). Differences in RPE were determined by an ART two-way mixed ANOVA with one between-subject factor (condition: N vs. NH vs. HH) and one within-subject factor (session: from one to eight) and interaction terms (condition x session). The original RPE data first underwent ART (ARTool for Windows, version 2.1.2), and then, the ranked RPE data were analyzed with the usual ANOVA procedure (Feys 2016). The level of significance was set a priori at P < 0.05. Statistical analyses were conducted using SPSS Statistics for Windows (v. 22; IBM Corp., Armonk, NY).
Results
Strength performance
After the intervention, all three groups significantly improved both the absolute and the relative load lifted in back squat (F = 161.2, P < 0.001, η2p = 0.8; and F = 149.2, P < 0.001, η2p = 0.8, respectively) and bench press (F = 139.9, P < 0.001, η2p = 0.8; and F = 281.8, P < 0.001, η2p = 0.9, respectively, Table 2). In back squat, the absolute and the relative load lifted was significantly higher in the NH group compared to the HH group (123.8 ± 17.7 kg vs. 103.9 ± 15.2 kg, P = 0.03 and 1.6 ± 0.2 kg vs. 1.4 ± 0.2 kg, P = 0.04, respectively). However, in bench press, no differences were found among groups in absolute (F = 2.1, P = 0.1, η2p = 0.1) nor relative values (F = 2.6, P = 0.09, η2p = 0.1).
Regarding changes, lower Δ% in the absolute load lifted were found for the back squat in N when compared to the NH group (12.9 ± 9.9% vs. 23.2 ± 8.2%, F = 4.5, P = 0.03, η2p = 0.2, Table 2) with no significant differences in bench press among groups (F = 1.7, P = 0.2, η2p = 0.1). Similarly, lower Δ% in the relative load lifted were found for the back squat in the N group (11.5 ± 8.8%) when compared to the NH group (22.2 ± 8.2%, P = 0.01) and the HH group (22 ± 8.1%, P = 0.02). However, no significant differences were found for this parameter in bench press among groups (F = 2.8, P = 0.08, η2p = 0.2).
The displaced external load
The RVL distribution across the RT program was similar in all three groups (F = 0.7, P = 0.7, η2p = 0.05), with a significant main effect for “session” (F = 15.4, P < 0.001, η2p = 0.4; Table 3). Similar ΔRVL across 8 weeks were found for all three groups (F = 0.6, P = 0.8, η2p = 0.04), with a significant main effect for “session” (F = 12.4, P < 0.001, η2p = 0.3; Fig. 2). At the end of the RT program, mean ΔRVL values were N: 20.4 ± 14.6% vs. HH: 25 ± 12.3% vs. NH: 31.5 ± 15.4%; (F = 0.9, P = 0.4, η2p = 0.05) in their respective conditions.
Internal load markers
The average SpO2 values were significantly lower in HH and NH compared to N, both before (HH: 93.8 ± 1.5 and NH: 94 ± 2.2 vs. N: 97.7 ± 1.3%; F = 56.5, P < 0.001, η2p = 0.8) and after the program (HH: 93.5 ± 1.3 and NH: 92.5 ± 2.7 vs. N: 96.3 ± 1.1%; F = 113.7, P < 0.001, η2p = 0.9). Significant differences between pre- and post-session SpO2 values were found in NH (F = 19.2, P < 0.001, η2p = 0.2) and N (F = 44.9, P < 0.001, η2p = 0.4), with lower values observed after the session.
The pattern of HR response was similar in most of the HR parameters for all three groups. However, a significant main effect for “session” was found in HRpre (F = 8.6, P < 0.001, η2p = 0.2) and HRmin (F = 5, P < 0.001, η2p = 0.1; Table 3).
There were no significant differences among groups in HRR1 (N: 39.2 ± 11.1 beats, HH: 36.1 ± 17.3 beats, NH: 44.4 ± 14 beats, F = 1.4, P = 0.2, η2p = 0.8). However, there was a main effect for “session” (F = 24.6, P < 0.001, η2p = 0.5; Table 3). A significant condition x session interaction effect was found in HRR2 (N: 52.8 ± 12.1 beats, HH: 53.9 ± 13.2 beats, NH: 51.4 ± 11.4 beats, F = 2.8, P = 0.006, η2p = 0.2), with the N group showing reduced values at sessions three (P < 0.001), five (P = 0.01), and six (P = 0.003), and the NH group showing reduced values at sessions four (P = 0.01), 6 (P = 0.02), and seven (P = 0.04, Table 4).
No significant differences in RPE were found among groups (F = 0.3, P = 0.7) nor between sessions (F = 0.8, P = 0.5). Even a significant condition x session interaction effect was found (F = 4.3, P = 0.026, η2p = 0.3), pairwise comparisons showed no significant differences (P˃0.05).
Discussion
This is the first study to monitor and compare both external and internal load markers during an 8-week RT program in three different environments: normoxia, intermittent hypobaric hypoxia, and intermittent normobaric hypoxia. Our research led to three principal findings: (1) the RVL dynamics were similar in all three groups across the 8-week program, with the hypoxic groups achieving larger improvements in relative 1RM back squat; (2) the indices of physiological stress (HR and RPE) during the RT program seemed to be similar in all three groups; and (3) the exposure to hypobaric hypoxia seems to speed recovery during RT.
In our study, all three groups showed similar RVL dynamics during the RT program (Table 3), with an increased RVL at the end (Fig. 2). In agreement with recent studies (Inness et al. 2016; Guardado et al. 2020), the HH and NH groups showed higher values of relative 1RM in back squat compared to the N group after the program. It is well known that RT in intermittent hypoxic conditions produces some physiological adaptations resulting in higher levels of both muscle hypertrophy and maximal strength compared to the same RT performed in normoxia (Kurobe et al. 2015; Kon et al. 2010). So, why did the relative one RM for bench press not improve? The benefit of RT under hypoxic conditions is based on the large accumulation of metabolic byproducts due to hypoxia, such as blood lactate, protons (H+), calcium, and inorganic phosphorus, among others, derived from the increase in anaerobic metabolism to compensate the loss of oxygen availability (Kon et al. 2012; Kurobe et al. 2015; Schoenfeld 2013). In the back squat, where more muscle mass is at work, a larger accumulation of metabolic waste byproducts occurs with the concomitant larger improvement in the strength levels. In addition, the observed distinctions in back squat performance could also be attributed to the program's design, particularly the inclusion of two lower-body push exercises vs. one upper-body push exercise as illustrated in Fig. 1.
Concerning the HR, all three groups showed similar HR responses across the RT program. This is in line with Scott et al. (2017), who reported similar HR responses between a normoxic group (FiO2 = 21%) and a hypoxic group (FiO2 = 16%) during a RT session (Scott et al. 2017). It is well known that there is a linear relationship between SpO2 and HR. While at sea level, SpO2 hovers around 98–100%; above 3100 MASL (FiO2 = 14%), SpO2 drops to 80% due to the lower PaO2, requiring the heart to increase the HR to maintain appropriate oxygen delivery to tissues (Cardiology 2012). In our study, on average, the difference in SpO2 between the hypoxic groups and the N group both before (-3.8%) and after the session (-3.3%) would not have been enough to significantly modify the HR pattern. Another possible explanation could rely on the intrasubject variation. Expressed in bpm, the day-to-day variations in submaximal HR could be estimated at around five–eight bpm (Lamberts et al. 2004). This means that the expected difference between normoxia and hypoxia in terms of the HR pattern at moderate altitude (for instance, our 2320 MASL) could be hidden by the spontaneous fluctuations of HR for a given training load. Furthermore, it is well known that other factors such as endurance training experience and genetics could have also affected the HR response of our participants (Mollard et al. 2007; Masschelein et al. 2015).
In the present study, the HH group showed larger HRR2 values during a few sessions of the RT program (Table 4) showing faster recovery. According to the literature, higher levels of HRR2 are indicative of a more efficient cardiovascular system, suggesting that the heart can rapidly return to baseline levels after exertion, which is generally associated with better cardiovascular fitness and health (Cole et al. 2000). HRR2 is influenced by the gradual decrease in sympathetic activity and the removal of metabolites (such as epinephrine, lactate, and H+) from the bloodstream, both of which are consequences of engaging in intense exercise (Imai et al. 1994). Terrestrial altitude in comparison to simulated leads to grater hypocapnia and blood alkalosis for the equivalent “altitude” due to the barometric pressure reduction (Savourey et al. 2003). In this sense, performing 2 months of RT at moderate hypobaric hypoxia may produce cardiorespiratory adaptations which in turn would speed recovery (Álvarez-Herms et al. 2012; Savourey et al. 2003). Our findings are consistent with those of Bhattarai et al. (2018), who observed comparable basal HR but significantly faster recovery of HR after step test in highlanders (~ 3000 MASL) vs. lowlanders (Bhattarai et al. 2018) and with those of Álvarez-Herms et al. (2012), who found better HRR2 values after 4 weeks RT in a hypobaric chamber compared to normoxia (Álvarez-Herms et al. 2012).
Regarding RPE, the Borg scale CR-10 has been proposed as a surrogate measure for the internal load during RT (Sweet et al. 2004; McGuigan et al. 2004). The lack of differences in RPE among groups could be explained by the same intensity applied (~ 70% 1RM) in all three conditions (Gearhart et al. 2002) and the dosage of hypoxia. Progressive arterial hypoxemia and increases in ventilation have been identified as the primary cues for determining RPE in moderate (FiO2 = 15.2%) and severe hypoxic (FiO2 = 11.4%) environments (Jeffries et al. 2019). It seems that in our study, the averaged SpO2 achieved in the hypoxic groups (HH: 93.5 ± 1.3 and NH: 92.5 ± 2.7) was not enough to trigger a decline in the perceptual responses. Attenuated RPE after hypoxic training has been described (Brocherie et al. 2017), suggesting an improved tolerance or acclimatization to hypoxia after only one session. In contrast, RT in hypoxia has been perceived as tougher (Inness et al. 2016; Rodríguez-Zamora et al. 2019) or without effect (Scott et al. 2015). These discrepancies may be attributed to the Borg scale used (6–20 vs. CR-10) and the athletic experience (Noble and Robertson 1996; Barroso et al. 2014). Future work should explore which parameters can explain the perceived exertion in RT under hypoxic conditions and to determine which internal load markers could potentially help the most to provide information about the athlete’s physiological stress in hypoxic environments.
Certain issues and limitations regarding the design, methodology, and overall validity of this study need to be considered. To include as many participants as possible in each group, it was decided to make the groups according to the subjects’ availability. Hence, there could have been some intrinsic characteristics of the groups (differences in motivation, personality, stress, etc.) that could have influenced the results of the study. In addition, the exact timing for parasympathetic reactivation post-exercise is likely to be highly impacted by an individual’s health and training status, and thus it is likely to vary from person to person. However, the within-subject design would have helped to minimize any potential variations attributed to that fact. In terms of methodology, the inclusion of markers for muscle activation and blood/urine samples could have offered valuable insights into the physiological responses to our intervention. However, a conscious decision was made to streamline our study design, prioritizing feasibility and practicality to address our primary research question. Studies with a larger sample size are recommended. Finally, due to technical problems with the HR devices, HRR2 for session two was not calculated.
Conclusions
The results of this study suggest that 8 weeks of intermittent RT in a hypoxic environment could help to maximize time-efficiency when aiming to improve strength levels in back squat. However, further research is needed. It seems that athletes may lift similar loads (%RM) compared to what can be lifted in normoxia without evoking higher levels of physiological stress. In addition, performing intermittent RT at hypobaric hypoxia may improve the cardiorespiratory response, which in turn could speed recovery. This is of considerable relevance for coaches because it highlights the importance of not only applying the appropriate training loads but also selecting the proper muscular environment during RT.
Data availability
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Abbreviations
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- FiO2 :
-
Inspired fraction of oxygen
- HH:
-
Hypobaric hypoxia
- HR:
-
Heart rate
- HRpre :
-
Average HR for the minute immediately before the start of the RT session
- HRmin :
-
Lowest HR value during the RT session
- HRpeak :
-
Highest HR value during the RT session
- HRmean :
-
Arithmetic HR mean for RT session
- HRR:
-
Heart rate recovery
- HRR1 :
-
HRR calculated as the difference between HRpeak and the resting heart rate after a 1 min rest
- HRR2 :
-
HRR calculated as the difference between HRpeak and the resting heart rate after a 2 min rest
- MASL:
-
Meters above sea level
- NH:
-
Normobaric hypoxia
- N:
-
Normoxia
- PaO2 :
-
Oxygen partial pressure
- RM:
-
Repetition maximum
- Δ%:
-
Repetition maximum percentage of change
- RVL:
-
Relative volume load
- ΔRVL:
-
Relative volume load percentage of change
- RT :
-
Resistance training
- RPE:
-
Rating of perceived exertion
- SpO2 :
-
Arterial oxygen saturation
- SD:
-
Standard deviation
References
Allen DG, Lamb GD, Westerblad H (2008) Skeletal muscle fatigue: cellular mechanisms. Physiol Rev 88(1):287–332
Álvarez-Herms J, Julià-Sánchez S, Corbi F, Pagès T, Viscor G (2012) Changes in heart rate recovery index after a programme of strength/endurance training in hypoxia. Apunts Sports Medicine 47(173):23–29
Amann M, Romer LM, Pegelow DF, Jacques AJ, Hess CJ, Dempsey JA (2006) Effects of arterial oxygen content on peripheral locomotor muscle fatigue. J Appl Physiol 101(1):119–127
Apkarian M (2019) Acute heart rate responses to resistance exercise at different cadenc-es. Int J Sports Exerc Med 5:143
Bakeman R (2005) Recommended effect size statistics for repeated measures designs. Behav Res Methods 37(3):379–384
Barroso R, Cardoso RK, do Carmo EC, Tricoli V (2014) Perceived exertion in coaches and young swimmers with different training experience. Int J Sports Physiol Perform 9 (2):212-216
de Beukelaar TT, Mantini D (2023) Monitoring resistance training in real time with wearable technology: current applications and future directions. Bioengineering (Basel) 10 (9). doi:https://doi.org/10.3390/bioengineering10091085
Bhattarai P, Paudel BH, Thakur D, Bhattarai B, Subedi B, Khadka R (2018) Effect of long term high altitude exposure on cardiovascular autonomic adjustment during rest and post-exercise recovery. Ann Occupat Environ Med 30(1):1–6
Brocherie F, Millet GP, Girard O (2017) Psychophysiological responses to repeated-sprint training in normobaric hypoxia and normoxia. Int J Sports Physiol Perform 12(1):115–123
Brown LE, Weir JP (2001) ASEP procedures recommendation I: accurate assessment of muscular strength and power. J Exerc Physiol Online 4 (3)
Brzycki M (1993) Strength Testing—predicting a one rep max from reps to fatigue. J Phys Educ Recreat Dance 64(1):88–90
Cardiology ACo (2012) Elevated thinking: altitude and the heart.
Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrance Eribaum Association, 2 edn.,
Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS (1999) Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med 341(18):1351–1357
Cole CR, Foody JM, Blackstone EH, Lauer MS (2000) Heart rate recovery after submaximal exercise testing as a predictor of mortality in a cardiovascularly healthy cohort. Ann Intern Med 132(7):552–555
Feys J (2016) New nonparametric rank tests for interactions in factorial designs with repeated measures. J Mod Appl Stat Methods 15(1):6
Gearhart RE Jr, Goss FL, Lagally KM, Jakicic JM, Gallagher J, Gallagher KI, Robertson RJ (2002) Ratings of perceived exertion in active muscle during high-intensity and low-intensity resistance exercise. J Strength Cond Res 16(1):87–91
Genner KM, Weston M (2014) A comparison of workload quantification methods in relation to physiological responses to resistance exercise. J Strength Cond Res 28(9):2621–2627
Guardado IM, Ureña BS, Cardenosa AC, Cardenosa MC, Camacho GO, Andrada RT (2020) Effects of strength training under hypoxic conditions on muscle performance, body composition and haematological variables. Biol Sport 37(2):121–129
Halson SL (2014) Monitoring training load to understand fatigue in athletes. Sports Med 44(2):139–147
Hill DW, Butler SD (1991) Haemodynamic responses to weightlifting exercise. Sports Med 12:1–7
Imai K, Sato H, Hori M, Kusuoka H, Ozaki H, Yokoyama H, Takeda H, Inoue M, Kamada T (1994) Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J Am Coll Cardiol 24(6):1529–1535. https://doi.org/10.1016/0735-1097(94)90150-3
Impellizzeri FM, Marcora SM, Coutts AJ (2018) Internal and external training load: 15 years on. Int J Sports Physiol Perform 14(2):270–273
Inness MW, Billaut F, Walker EJ, Petersen AC, Sweeting AJ, Aughey RJ (2016) Heavy Resistance Training in Hypoxia Enhances 1RM Squat Performance. Front Physiol 7:502
Jeffries O, Patterson SD, Waldron M (2019) The effect of severe and moderate hypoxia on exercise at a fixed level of perceived exertion. Eur J Appl Physiol 119(5):1213–1224
Kon M, Ikeda T, Homma T, Akimoto T, Suzuki Y, Kawahara T (2010) Effects of acute hypoxia on metabolic and hormonal responses to resistance exercise. Med Sci Sports Exerc 42(7):1279–1285
Kon M, Ikeda T, Homma T, Suzuki Y (2012) Effects of low-intensity resistance exercise under acute systemic hypoxia on hormonal responses. J Strength Cond Res 26
Kraemer WJ, Gordon SE, Fleck SJ, Marchitelli LJ, Mello R, Dziados JE, Friedl K, Harman E, Maresh C, Fry AC (1991) Endogenous anabolic hormonal and growth factor responses to heavy resistance exercise in males and females. Int J Sports Med 12(2):228–235
Kraemer WJ, Adams K, Cafarelli E, Dudley GA, Dooly C, Feigenbaum MS, Fleck SJ, Franklin B, Fry AC, Hoffman JR, Newton RU, Potteiger J, Stone MH, Ratamess NA, T. T-M (2009) American College of Sports Medicine. Progression Models in Resistance Training for Healthy Adults. 41 (3):687-708
Kurobe K, Huang Z, Nishiwaki M, Yamamoto M, Kanehisa H, Ogita F (2015) Effects of resistance training under hypoxic conditions on muscle hypertrophy and strength. Clin Physiol Funct Imaging 35(3):197–202
Lamberts RP, Lemmink KA, Durandt JJ, Lambert MI (2004) Variation in heart rate during submaximal exercise: implications for monitoring training. J Strength Cond Res 18(3):641–645
Masschelein E, Van Thienen R, Thomis M, Hespel P (2015) High twin resemblance for sensitivity to hypoxia. Med Sci Sports Exerc 47(1):74–81
McGuigan MR, Egan AD, Foster C (2004) Salivary cortisol responses and perceived exertion during high intensity and low intensity bouts of resistance exercise. J Sports Sci Med 3(1):8–15
McLaren SJ, Smith A, Spears IR, Weston M (2017) A detailed quantification of differential ratings of perceived exertion during team-sport training. J Sci Med Sport 20(3):290–295
Millet GP, Debevec T (2020) CrossTalk proposal: Barometric pressure, independent of, is the forgotten parameter in altitude physiology and mountain medicine. J Physiol 598(5):893–896
Mollard P, Woorons X, Letournel M, Lamberto C, Favret F, Pichon A, Beaudry M, Richalet J-P (2007) Determinants of maximal oxygen uptake in moderate acute hypoxia in endurance athletes. Eur J Appl Physiol 100(6):663–673
Moreira OC, Oliveira CEP, Matos DG, Silva SF, Hickner RC, Aidar FJ (2017) Cardiovascular response to strength training is more affected by intensity than volume in healthy subjects. Revista Andaluza De Medicina Del Deporte. https://doi.org/10.1016/j.ramd.2017.01.002
Mourot L (2018) Limitation of maximal heart rate in hypoxia: mechanisms and clinical importance. Front Physiol 9:972
Narici MV, Kayser B (1995) Hypertrophic response of human skeletal muscle to strength training in hypoxia and normoxia. Eur J Appl Physiol Occup Physiol 70(3):213–219
Noble BJ, Robertson RJ (1996) Perceived Exertion. Human Kinetics, Champaign, IL
Noble BJ, Borg GAV, Jacobs I, Ceci R, Kaiser P (1983) A category-ratio perceived exertion scale: relationship to blood and muscle lactates and heart rate. Med Sci Sports Exerc 15(6):523–528
Patterson SD, Hughes L, Warmington S, Burr J, Scott BR, Owens J, Abe T, Nielsen JL, Libardi CA, Laurentino G, Neto GR, Brandner C, Martin-Hernandez J, Loenneke J (2019) Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol 10:533. https://doi.org/10.3389/fphys.2019.00533
Psycharakis SG (2011) A longitudinal analysis on the validity and reliability of ratings of perceived exertion for elite swimmers. J Strength Cond Res 25(2):420–426
Rodríguez-Zamora L, Padial P, Schoenfeld BJ, Feriche B (2019) Mean propulsive velocity is a viable method for adjusting the resistance-training load at moderate altitude. Front Sports Act Living 1:52
Savourey G, Launay JC, Besnard Y, Guinet A, Travers S (2003) Normo- and hypobaric hypoxia: are there any physiological differences? Eur J Appl Physiol 89(2):122–126. https://doi.org/10.1007/s00421-002-0789-8
Schoenfeld BJ (2013) Potential mechanisms for a role of metabolic stress in hypertrophic adaptations to resistance training. Sports Med 43(3):179–194
Scott BR, Slattery KM, Sculley DV, Hodson JA, Dascombe BJ (2015) Physical performance during high-intensity resistance exercise in normoxic and hypoxic conditions. J Strength Cond Res 29(3):807–815
Scott BR, Slattery KM, Sculley DV, Lockhart C, Dascombe BJ (2017) Acute physiological responses to moderate-load resistance exercise in hypoxia. J Strength Cond Res 31(7):1973–1981
Sweet TW, Foster C, Mcguigan MR, Brice G (2004) Quantitation of resistance training using the session rating of perceived exertion method. J Strength Cond Res 18(4):796–802
Timon R, Olcina G, Padial P, Bonitch-Góngora J, Martínez-Guardado I, Benavente C, de la Fuente B, Feriche B (2022) Effects of Resistance Training in Hypobaric vs. Normobaric Hypoxia on Circulating Ions and Hormones. International Journal of Environmental Research and Public Health 19 (6):3436
Acknowledgements
We thank the subjects for participating and the High-Performance Center of Sierra Nevada (CSD, Granada, Spain) for allowing the study to be done. The authors also thank Life Pro Nutrition for supplying the protein shakes used as supplements in this study, and to Diego Montiel Rojas for his valuable advice regarding statistics. Our grateful thanks are also extended to Mr. Leo Jacobsson for his help in language editing. Finally, to Prof. Ferran Rodríguez Guisado, who passed away on 23rd of January 2023 at the age of 66, for contributing indirectly with his unsurpassed knowledge in exercise physiology.
Funding
Open access funding provided by Örebro University. This work was supported by the Spanish Ministry of Science, Innovation and Universities under grant [PGC2018-097388-B-I00-MCI/AEI/FEDER, UE], by the Andalusian FEDER Operational Program [B-CTS-374-UGR20] and FPU pre-doctoral grant [FPU18/00686] awarded to one of the authors. The Örebro University provided the funding for publication.
Author information
Authors and Affiliations
Contributions
LR-Z, PP, and BF: conceived and designed the experiments. LR-Z, CB, IP, PP, RT, JA and BF: performed the experiments. LR-Z, CB, IP: analyzed the data. LR-Z wrote the paper. BF: revised the paper. All the authors have reviewed and approved the manuscript prior submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Communicated by William J. Kraemer.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rodríguez-Zamora, L., Benavente, C., Petrer, I. et al. Hypoxia matters: comparison of external and internal training load markers during an 8-week resistance training program in normoxia, normobaric hypoxia and hypobaric hypoxia. Eur J Appl Physiol (2024). https://doi.org/10.1007/s00421-024-05442-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00421-024-05442-1