Abstract
Purpose
This study examined the acute effects of interrupting sitting with light-intensity walking on postprandial cardiometabolic risk markers in South Asian adults.
Methods
South Asians with overweight/obesity (n = 19; body mass index [BMI] > 23 kg·m−2) and normal-weight (n = 8; BMI 18.0–22.9 kg·m−2) aged 48.8 ± 5.6 years completed two, 5-h conditions: (1) prolonged sitting (SIT), and (2) interrupted sitting with 5-min bouts of light-intensity walking every 30-min (INT-SIT). Blood samples and resting expired air samples were collected throughout each condition. Statistical analyses were completed using linear mixed models.
Results
In participants with overweight/obesity, postprandial glucose, triglycerides (TAG) and metabolic load index (MLI) over time were lower, whereas resting substrate utilisation and resting energy expenditure (REE) were higher, in INT-SIT than SIT (all p ≤ 0.05). Compared with SIT (0.18 [95% CI 0.13, 0.22] kcal.min−1), INT-SIT (0.23 [95% CI 0.18, 0.27] kcal.min−1) increased postprandial REE iAUC in participants with overweight/obesity (p = 0.04, d = 0.51). Postprandial TAG concentrations over time were lower in INT-SIT versus SIT (p = 0.01, d = 30) in normal-weight participants, with no differences in any other outcomes for this sample group.
Conclusion
These findings suggest that interrupting sitting with 5-min bouts of light walking every 30-min acutely attenuates cardiometabolic risk markers among South Asians living with overweight/obesity, whereas limited effects may be seen in individuals with normal-weight.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
South Asians are the indigenous population originating from the Indian subcontinent, including Bangladesh, India, Pakistan, Sri-Lanka, and Nepal (Jalal et al. 2019). Individuals of this ethnic background represent approximately 25% of the world’s population (The World Bank Group 2021). South Asians have a significantly increased risk (up to six times) of developing cardiometabolic diseases, such as cardiovascular disease (CVD) and Type 2 diabetes, compared with other ethnic groups (Hanif and Susarla 2018; Misra and Khurana 2011). This may be in part due to having a thin outside, fat inside phenotype; thus, South Asians have excess internal body fat (e.g., higher abdominal, visceral, and hepatic fat), lower lean muscle mass, and greater accumulation of fat in ectopic sites including liver and skeletal muscle, compared to other ethnic groups (Bays et al. 2022; Misra and Khurana 2011). In attempts to account for this distinct phenotype, lower body mass index (BMI) and waist circumference cut-off points have been proposed for South Asians (Misra and Khurana 2011). Obesity, and in particular abdominal fatness, is a predisposing factor in the development of cardiometabolic disease, possibly due to the presence of insulin resistance (Gray et al. 2011). For instance, type 2 diabetes is reported to be five times more prevalent in individuals with obesity than normal-weight adults (Abdullah et al. 2010). Thus, South Asians living with overweight/obesity are considered a high-risk group that would benefit from interventions to reduce the risk of cardiometabolic disease.
Overweight and obesity is associated with lower physical activity and higher sedentary time in the general population (Gibbs et al. 2017; Van Dyck et al. 2015). Increased physical activity engagement in individuals with overweight and obesity is related to self-perceived good health, self-efficacy, social support and exercise enjoyment (Curran et al. 2023). There is some evidence that being an office worker, severity of obesity and number of comorbidities is related to greater sedentary time (Curran et al. 2023). Higher sedentary time is detrimentally associated with cardiometabolic risk markers (such as fasting glucose and triglycerides [TAG]) and incidence of type 2 diabetes, CVD and CVD mortality (Bailey et al. 2019; Healy et al. 2011; Patterson et al. 2018). Increased postprandial hyperglycaemia and hyperlipidaemia are strong predictors of cardiometabolic disease and may represent a suitable intervention target for managing cardiometabolic health (Einarson et al. 2011; O’Keefe and Bell 2007). Interrupting prolonged sitting with 1-min 40-s to 5-min bouts of light or moderate-intensity walking every 20 to 30-min significantly attenuated postprandial cardiometabolic risk markers (e.g., glucose and insulin) in Caucasian participants who are normal-weight or living with overweight and obesity (Champion et al. 2018; Dunstan et al. 2012; Henson et al. 2016; Larsen et al. 2015; Peddie et al. 2013). Interrupting prolonged sitting with 5-min bouts of light walking also attenuated postprandial insulin in older South Asians (aged 65–79 years) with mixed weight status (Yates et al. 2020). Fat oxidation and resting energy expenditure (REE) were also significantly higher in response to interrupting sitting with light or moderate-intensity walking for 1 to 2-min every 30-min, chair squats or intermittent standing every 20-min, compared with prolonged sitting in Caucasians living with normal-weight or overweight/obesity (Hawari et al. 2019, 2016; Larsen et al. 2017; Peddie et al. 2013). Thus, interrupting sitting has acute beneficial cardiometabolic and substrate utilisation effects.
The benefits of interrupting sitting appear to be more pronounced in participants with overweight and obesity than those with normal-weight. This could be due to a larger scope for improvement as well as physical activity being a more stressful stimulus in less fit populations (Bell et al. 2023). South Asians spend a large proportion of their time being sedentary, particularly when measured using device-based methods (~ 9 h/day) (Dey et al. 2021). This could place them at increased cardiometabolic disease risk, especially if they are overweight or obese (Ahmad et al. 2017). Yet, there is limited evidence examining the effects of interrupting sitting on cardiometabolic health in South Asian adults of differing weight status. Such research is important to inform specific target groups that may benefit from this type of intervention.
This study aimed to determine the effects of interrupting sitting with light walking on postprandial cardiometabolic risk markers (primary outcome) and resting metabolic rate (i.e., resting substrate utilisation and energy expenditure; secondary outcomes) in South Asian adults living with normal-weight and overweight/obesity. It was hypothesised that interrupting sitting would attenuate postprandial glucose in South Asian adults, but this effect would be more pronounced in participants with overweight/obesity.
Methods
Study overview
This two-condition randomised crossover study was conducted according to the Declaration of Helsinki principles and approved by the University of Bedfordshire Institute for Sport and Physical Activity Research Ethics Committee (2019ISPAR003). Participants provided written informed consent prior to taking part in any study procedures. The study was conducted and reported in line with the Consolidated Standards of Reporting Trials (CONSORT) guidance (Moher et al. 2012); see checklist in Supplementary Material S1. The trial was registered with clinicaltrials.gov/ (NCT03898206). Experimental condition order was randomised using an online computer-generated randomisation method (https://www.randomizer.org/). Following a preliminary testing visit, participants completed two experimental conditions separated by ≥ 3 to 28 days to eliminate potential carryover effects (Mikines et al. 1988). Female participants were tested between 1 and 10 days into their follicular phase to minimise the influence of hormonal fluctuations on glucose metabolism (Pulido and Salazar 1999). The study was interrupted by the COVID-19 pandemic, affecting the ability to continue data collection; the associated impact on the study protocol is described below. All testing procedures took place at the University of Bedfordshire Sport and Exercise Science Laboratories.
Participants
South Asian adults aged 18 to 75 years who were normal-weight (BMI 18.0–22.90 kg.m−2) or overweight/obese (BMI > 23 kg.m−2) were eligible to take part. These BMI thresholds were used in line with recommendations for South Asian populations (Bays et al. 2022). Body mass index was calculated as body mass (kg) ÷ height (m)2. ‘South Asian’ was defined as anyone identifying themselves as South Asian or British South Asian (Bays et al. 2022). Exclusion criteria were self-reported CVD, diabetes, any known blood borne disease, pregnancy, recent or current smoker, allergies to the test meals, other known health issues (e.g., neurological disorders), or any injuries that might limit the ability to perform light walking. Participants were recruited from the local community (Luton and Bedford, UK) using adverts through social media posts (e.g., Facebook and Twitter) and distribution of flyers.
Sample size calculations
This study was originally designed to investigate the interaction between weight status and interrupted sitting on cardiometabolic outcomes. The primary outcome was postprandial glucose iAUC. An a-priori sample size was calculated to provide sufficient power to detect a weight status x experimental condition interaction, which resulted in an estimated 52 participants being required (26 in each the normal-weight and overweight/obese groups). Unfortunately, data collection was suspended due to the COVID-19 pandemic, which meant that it was no longer possible to complete data collection for the intended 52 participants within the time constraints of the study. Thus, sample size estimations were re-visited in an attempt to use the available data in the most meaningful way. Rather than examining the weight status x experimental condition interaction, analyses comparing experimental conditions were conducted separately for normal-weight and participants with overweight/obesity, with between-group comparisons interpreted descriptively in the discussion rather than being determined statistically (Gondim et al. 2015).
To detect statistical significance between conditions in each group separately, a total of nine normal-weight and 12 participants with overweight/obesity were required. These calculations were based on a mean effect size of d = 1.12 for normal-weight and d = 0.89 for participants with overweight/obesity from previous research (Bailey and Locke 2015; Dunstan et al. 2012; Henson et al. 2016; Peddie et al. 2013; Yates et al. 2020) to achieve 80% power with an alpha level of 5%. A total of 12 normal-weight and 16 participants with overweight/obesity, allowing for a 20% dropout, was the revised target sample size. Sample size calculations were performed using G* power (version 3.0.10; Germany).
Preliminary measures
Height (cm) was measured to the nearest 0.1 cm using a stadiometer (Harpenden 98.602, Crymych, UK). Body mass (kg) was measured to the nearest 0.1 kg, and the percentage of body fat (BF %) was estimated after fasting for 4 h, using the Tanita BC-418 Segmental Body Composition Analyzer (Tanita Corp., Tokyo, Japan). Waist circumference (cm) was measured at minimal inspiration to the nearest 0.1 cm (Lohman et al. 1988). Resting blood pressure (BP; mmHg) and heart rate (HR; beats.min−1) were measured using an automatic device (Omron M5-I; Omron Matsusaka Co. Ltd., Matsusaka, Japan). Participants were familiarised with the Borg Rating of Perceived Exertion (RPE) scale (Borg 1982) and the Woodway motorised treadmill (Woodway PPS55Med-i, GmbH, Germany). An exercise protocol to determine the walking speed for each participant in the relevant experimental condition began at a speed of 1.2 km.h−1 and increased by 0.5 km.h−1 every 2-min until an RPE of 9 (very light) was reached. This speed was recorded for each participant (Bailey and Locke 2015).
Experimental protocol
Participants attended two separate laboratory visits at 08:30 am in the fasted state (Henson et al. 2016). They were asked to refrain from food and drink containing alcohol and caffeine for 24-h before and to avoid moderate-to-vigorous exercise 48-h before each condition to exclude possible acute influences on insulin sensitivity (Mikines et al. 1988). Participants were asked to weigh and record all food and beverages consumed for 24-h before their first experimental condition and then consume the same volume of food and beverage at the exact times in the 24-h before their second experimental condition. This was to minimise the influence of chronobiological aspects of dietary intake (e.g., timing, and frequency) and macronutrient intake on cardiometabolic risk marker responses (Ekmekcioglu and Touitou 2011). Participants were instructed to travel by car and park as close as possible to the laboratories to minimise physical activity in the hours before each condition. Upon arrival, participants sat for 5-min and resting BP and HR were measured. Afterwards, resting expired air was collected continuously for 5-min using a Metalyzer 3B (Cortex Biophysik, Leipzig, Germany). A fasting blood sample was then taken immediately before consuming a standardised breakfast. The 5-h experimental condition began immediately after the breakfast was consumed. The conditions were as follows, as illustrated in Fig. 1:
-
(1)
SIT: Participants remained seated at a desk for 5-h and were instructed to reduce excessive movement.
-
(2)
INT-SIT: Participants interrupted their sitting every 30-min with walking on a motorised treadmill at a light-intensity for 5-min. Participants started the walking breaks at 30, 60, 90, 120, 150 and 180-min into the breakfast postprandial period and 30, 60 and 90-min into the lunch postprandial period. The walking breaks were undertaken on nine occasions, providing a total of 45-min of light walking.
A standardised lunch meal was provided at 3 h into each condition. Participants were permitted to read books, newspapers, and magazines, or work on a laptop/computer throughout the conditions. When participants needed to use the toilet, they were transported in a wheelchair to avoid physical activity.
Test meals
The standardised breakfast and lunch meals both provided 25% of the estimated daily energy requirements for each participant (Mattes and Campbell 2009). Energy requirements were estimated based on each participant’s age and body mass using Mifflin equations (Mifflin et al. 1990). Breakfast consisted of cornflakes, whole milk, jam sandwich and orange juice that comprised 58% carbohydrate, 28% fat and 13% protein (Champion et al. 2018). Lunch consisted of a chicken (non-halal or halal) or cheese sandwich, salted crisps, chocolate and Lucozade original drink that comprised 58% carbohydrate, 28% fat and 13% protein (Champion et al. 2018). The glycaemic index (GI) of the breakfast and lunch was 73 and 74, respectively; values were obtained from the International Tables of GI and Glycaemic Load Values 2008 (Atkinson et al. 2008). The macronutrient content and GI of the meals were intended to provide a postprandial stimulus that would be sensitive to breaks in sitting (Augustin et al. 2015). Participants were asked to consume each meal within 15-min and replicate the consumption times from the first condition in the second condition (Henson et al. 2016). Water was provided ad libitum during the first condition, and the total volume consumed was recorded. Participants were asked to replicate this amount during the second condition (Henson et al. 2016).
Blood collection and biochemistry
Capillary finger prick blood samples were collected in a fasted state at baseline followed by subsequent samples at 25, 55, 85, 115, and 175-min during the breakfast postprandial period and at 25, 55, 85, and 115-min during the lunch postprandial period. Whole blood was used to analyse glucose (mmol.L−1) using the YSI 2300 STAT glucose analyser (YSI Inc., Yellow Springs, OH, USA) and TAG (mmol.L−1) using the Reflotron®Plus (Roche Diagnostics, Burgess Hill, UK). The remaining blood was centrifuged using a micro-centrifugal machine (Heraeus Pico 17 microcentrifuge, Loughborough, UK) at 2000 × g for 5-min (Bailey and Locke 2015). Plasma was extracted and stored at − 80 °C. Plasma insulin (mU.L−1) was analysed using an enzyme-linked immunosorbent assay kit (Mercodia AB, Uppsala, Sweden).
Resting substrate utilisation and energy expenditure
Expired air samples were collected for 5-min after a 10–20 min rest to estimate resting fat oxidation (mg.min−1), carbohydrate oxidation (mg.min−1) and REE (kcal.min−1) using the Metalyzer 3B. These samples were taken in a fasted state at baseline followed by samples at 20, 50, 80, 110, 140, and 170-min during the breakfast postprandial period and 20, 50, 80, and 110-min during the lunch postprandial period.
Blood pressure and heart rate measurement
Resting BP (mmHg) and HR (beats.min−1) were measured on the left arm while seated in an upright resting position. At baseline, three readings were taken with the mean from the lowest two measurements being recorded. Subsequent single readings were taken at 15, 45, 75, 105, 135 and 165-min during the breakfast postprandial period and 15, 45, 75 and 105-min during the lunch postprandial period.
Calculation of outcome variables
The total 300-min (5-h) area under the curve (tAUC), incremental AUC (iAUC) and positive iAUC (p-iAUC; i.e., excluding any data below baseline) were calculated for postprandial blood glucose, TAG, metabolic load index (MLI) and plasma insulin. Total area under the curve and iAUC were calculated for resting fat oxidation, carbohydrate oxidation and REE. Area under the curve was calculated using the trapezoidal rule and p-iAUC was calculated as tAUC above the baseline value (Wolever and Jenkins 1986). The MLI was calculated using the following equation: MLI (mmol.L−1) = blood glucose (mmol.L−1) + TAG (mmol.L−1) (Emerson et al. 2016). Resting substrate utilisation was calculated by indirect calorimetry using stoichiometric equations with the assumption that the contribution of protein to energy expenditure is negligible (Frayn 1983). The following formula was used to calculate mean arterial pressure (MAP), where P is BP (systolic or diastolic) (DeMers and Wachs 2019): MAP = PDiastolic + 1/3 (PSystolic – PDiastolic).
Statistical analysis
Statistical analyses were performed using SPSS version 26.0 (SPSS Inc., NY, USA). Data were tested for normality using Q–Q plots prior to statistical analysis. Linear mixed models were used to determine the main effect of condition (INT-SIT vs. SIT) for the AUC variables and the condition × time (i.e. sample time points during each condition) interaction for all other outcomes. All models were adjusted for condition order and the baseline value of each outcome. Condition, time and covariates were included as fixed factors and participants were a random factor in each model. Two-tailed statistical significance was set at p ≤ 0.05. Cohen’s d effect sizes were calculated with 0.2, 0.5, and 0.8 indicating a small, medium or large effect, respectively (Cohen 1988). All data are presented as mean (95% confidential interval [CI]) unless stated otherwise.
Results
Recruitment and data collection of participants took place between April 2019 and March 2020. Participant flow throughout the study is shown in Supplementary Material S2. Following screening, 54 participants were enrolled into the study. Twenty-seven participants were unable to attend the laboratory to complete data collection due to the COVID-19 pandemic. Therefore, 27 (eight normal-weight and 19 with overweight/obesity) datasets were included in the analysis. Descriptive characteristics of the participants are presented in Table 1. The average (SEM) walking bout speed for the normal-weight and overweight/obese group was 2.5 ± 0.2 and 2.6 ± 0.2 km.h−1, respectively. There were no differences in the baseline variables between the two experimental conditions in either the normal-weight or overweight/obese groups (see Table 2).
Cardiometabolic risk markers
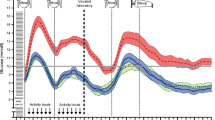
Postprandial glucose, triglycerides and MLI over time for each condition are shown in Fig. 2. Blood glucose concentrations across the 5-h were lower by -0.20 mmol.L−1 (95% CI -0.36, -0.04) in INT-SIT than SIT in the overweight/obese group (see Table 2). There was a trend for lower postprandial glucose iAUC in INT-SIT compared with SIT in the overweight/obese group. Triglycerides and MLI across the 5-h were attenuated in the overweight/obese group in INT-SIT by -0.09 mmol.L−1 (95% CI -0.17, 0.00) and -0.25 mmol.L−1 (95% CI -0.43, -0.06), respectively, compared with SIT (Table 2). Postprandial insulin, MAP and HR did not differ between conditions in the overweight/obese group. In the normal-weight group, TAG across the 5-h was attenuated by -0.12 mmol.L−1 (95% CI -0.22, -0.03) in INT-SIT than SIT (Table 2). There were no differences between conditions for the remaining cardiometabolic risk markers in the normal-weight group. There were no condition x time interaction effects for any variable in either group (see Fig. 2 and Supplementary Material S3; all p ≥ 0.27).
Postprandial blood glucose (A), triglycerides (C), and metabolic load index (E) in normal-weight South Asians and blood glucose (B), triglycerides (D) and metabolic load index (F) in South Asians living with overweight/obesity for the prolonged sitting (SIT) and sitting interrupted with light walking (INT-SIT) conditions. Data are mean and 95% confidence interval. Dotted lines indicate standardised test meals for breakfast and lunch
Substrate utilisation
Fat and carbohydrate oxidation across the 5-h were higher in INT-SIT by 2.81 mg.min−1 (95% CI 0.52, 5.09) and 11.41 mg.min−1 (95% CI 4.40, 18.43), respectively, compared with SIT in the overweight/obese group (see Supplementary Material S4). Postprandial substrate utilisation iAUC did not differ between conditions in the overweight/obese group. Resting energy expenditure across 5-h and iAUC were higher by 0.04 kcal.min−1 (95% CI 0.02, 0.06) and 0.05 kcal.min−1 (95% CI 0.00, 0.09), respectively, in INT-SIT than SIT in the overweight/obese group (see Supplementary Material S4). There was no condition x time interaction for any substrate utilisation outcomes in the overweight/obese group (p ≥ 0.81). In the normal-weight group, the main effect of condition and condition x time interactions for substrate utilisation outcomes were all non-significant (p ≥ 0.12) (see Supplementary Material S5).
Discussion
The findings of this study supported the hypothesis that interrupting sitting with 5-min bouts of light walking every 30-min acutely attenuated postprandial glucose, TAG and MLI in South Asians with overweight/obesity, with limited effects seen in participants with normal-weight. This supports previous research that has consistently found beneficial cardiometabolic responses to interrupting sitting with 2 to 5-min of walking every 20 to 30-min in overweight/obese Caucasians (Dunstan et al. 2012; Henson et al. 2016; Larsen et al. 2015). Similar to the present findings, other studies have found no changes in postprandial glucose or TAG when sitting was interrupted with light or moderate-intensity walking or cycling for 2 to 8-min every 20 to 60-min in normal-weight Caucasians (Altenburg et al. 2013; Hansen et al. 2016), although the literature is conflicting (Bailey and Locke 2015; Bailey et al. 2017; Peddie et al. 2013). This evidence suggests that interrupted sitting may provide a more pronounced and consistent cardiometabolic effect in participants with overweight or obesity than normal-weight individuals, perhaps due to their larger ‘scope for improvement’. Indeed, previous research shown that interrupted sitting with light walking consistently attenuates cardiometabolic risk markers (e.g., glucose) in populations with increased cardiometabolic risk, including individuals with overweight/obesity, Type 2 diabetes, and postmenopausal women (Dempsey et al. 2016; Dunstan et al. 2012; Henson et al. 2016; Larsen et al. 2015). The magnitude of response also appears to be comparatively greater in these population groups than in apparently healthy individuals (Hansen et al. 2016). The findings of the current study support a focus on interrupting sitting for managing cardiometabolic health in the short term, especially in individuals with overweight/obesity, regardless of their ethnicity.
There was a trend for interrupting sitting with light walking to attenuate postprandial glucose area under the curve (by 13% for iAUC) in South Asians with overweight/obesity, whereas no such trend was apparent for postprandial insulin. In Caucasians living with overweight/obesity, interrupting sitting with light walking for 2 to 5-min every 20 to 30-min attenuated postprandial glucose iAUC by 28% to 32% (Henson et al. 2016; Larsen et al. 2015) and insulin iAUC by 15% to 37% (Dunstan et al. 2012; Henson et al. 2016). The greater responses in these previous studies may have reflected the participants having larger impairments in cardiometabolic health (e.g., reduced glucose tolerance) and lower aerobic fitness than the present study’s sample. This cannot be said conclusively, though, as such measures of physical and cardiometabolic health are not taken consistently across studies. In Caucasians with normal-weight, reductions of 16% and 21% in glucose and insulin iAUC, respectively, have been found when sitting is interrupted with 2-min light walking every 20-min (Bailey and Locke 2015; Pulsford et al. 2017). The magnitude of the glucose reduction in the present study is comparatively lower. In addition to potential explanatory factors discussed above, the less frequent interruptions in sitting (i.e., every 30-min) compared with previous studies (i.e., every 20-min) could account for the lack of change in postprandial metabolism. Further studies are, therefore, required to understand the cardiometabolic effects of interrupting sitting with different frequencies and durations of physical activity in South Asians to better inform recommendations for managing cardiometabolic health. This research should also investigate the influence of physical and cardiometabolic health on postprandial metabolism.
In the only previous experimental study with South Asian participants (older adults aged > 65 years with a BMI of 26 [95% CI 23.7, 29.5] kg.m−2), interrupting sitting with light walking for 5-min every 30-min reduced postprandial insulin AUC by 27%, but did not affect postprandial glucose (Yates et al. 2020). The attenuated glucose in the absence of insulin changes in the present study may reflect an improved insulin sensitivity, or enhanced contraction-mediated glucose uptake, in response to interrupting sitting. In the study by Yates et al. (2020), participants were comparatively older (mean age 69 years) compared to the present participants (mean age 50 years). It is possible that postprandial glucose and insulin responses could be different in younger individuals due to differences in muscle or adipose tissue physiology, or fitness level (Bowden et al. 2019). The longer experimental condition in the study by Yates et al. (2020) meant that more walking bouts were accumulated that could have provided a greater stimulus for glucose uptake across the day, resulting in lower concentrations of insulin being required. The higher percentage of carbohydrate in the test meals in the present study could have resulted in a higher postprandial glucose response with more scope for reductions through interrupting sitting. These data suggest that interrupting sitting with light walking benefits postprandial metabolism in South Asian adults with overweight/obesity. Whether this is in the context of attenuated glucose or insulin may depend on the characteristics of the participants, the number of sitting interruptions or the test meal composition. It is recommended that interrupting sitting with light walking be considered as a potential strategy for improving postprandial metabolism in this ethnic group.
The present study observed reductions in postprandial TAG in both the overweight/obese and normal-weight groups in response to interrupting sitting. This is similar to studies in which sitting was interrupted with 3-min walking bouts in participants with normal-weight or overweight/obesity (Miyashita et al. 2015, 2006). Metabolic load index, which is a summative index reflecting excess energy from glucose and triglycerides, was reduced in the interrupted sitting condition in South Asian participants with overweight/obesity, but not in those with a normal-weight. Higher adiposity, that is associated with metabolic inflexibility and insulin resistance, may explain the more pronounced effects in individuals with overweight/obesity (Bays et al. 2022; Sattar and Gill 2015). Previous studies have not evaluated MLI. It is recommended that this outcome be considered in future research to extend knowledge regarding cardiometabolic responses to interrupting sitting.
Consistent with studies in normal-weight Caucasians (Charlett et al. 2021) and Caucasians living with overweight/obesity (Larsen et al. 2014), the present study found no change in MAP and HR in response to interrupting sitting. In contrast, other research has reported reductions in MAP (Barone Gibbs et al. 2017) when alternating between sitting and standing every 30-min in individuals with overweight/obesity and hypertension. It is plausible that individuals with hypertension may respond to interruptions in sitting to a greater extent than individuals with normal blood pressure levels. Alternatively, sitting may need to be interrupted for a longer duration for MAP benefits to be realised. This is supported with evidence of reduced MAP in response to alternating sitting and standing every 30-min (Barone Gibbs et al. 2017) and light walking for 20-min bouts each hour (Champion et al. 2018). According to the findings presented here, interrupting sitting with 5-min bouts of light walking every 30-min does not benefit MAP, acutely, in South Asians. Informed by previous data in Caucasians (Barone Gibbs et al. 2017; Champion et al. 2018), the effects of interrupting sitting with longer bouts of standing or physical activity should be examined in this ethnic group.
There was an increase in REE by 25% in response to interrupted sitting with light walking in South Asians living with overweight/obesity. Resting energy expenditure was also increased by up to 20% when interrupting sitting with chair squats (standing and sitting 10 times for 30-s every 20-min) or intermittent standing (standing 10 times for 1.5-min every 30-min) compared to prolonged sitting in adults Caucasian living with overweight/obesity (Hawari et al. 2019, 2016). The higher REE may be explained by higher fat (+ 14%) and carbohydrate (+ 19%) oxidation in response to interrupting sitting with light walking in the present study. Increased carbohydrate and fat oxidation were also reported in previous studies using chair squats, intermittent standing, and light or moderate-intensity walking bouts (Hawari et al. 2019, 2016; Peddie et al. 2013). The higher REE and substrate oxidation would aid in replenishing the additional energy used for muscle contractions during the sitting interruptions. Despite these effects in the overweight/obese group, the present study did not observe any changes in the normal-weight group. The benefits of interrupted sitting could be more pronounced in individuals with overweight/obesity compared with normal-weight due to walking being a weight-bearing activity, meaning a greater energy demand for those carrying more weight, or a lower fitness resulting in higher metabolic stress. That said, the 0.06 kcal/min−1 higher REE compared with prolonged sitting would equate to an additional energy expenditure of 126 kcal per week, which could have limited implications for long-term weight management. The magnitude of effect on substrate utilisation in South Asians with overweight/obesity should be explored in future studies with differing protocols for interrupting sitting to inform the potential of this strategy for weight management.
Strengths and limitations
This study adds important knowledge to the scarce literature investigating the effects of interrupted sitting on cardiometabolic risk markers and resting substrate utilisation in South Asians living with normal-weight and overweight/obesity. The strengths of this study also include the randomised cross-over design in a controlled laboratory setting, where manipulations in sitting and dietary intake were strictly controlled throughout the experimental protocol. This acute study meant that any long-term effects were not examined. A further limitation is the evaluation of postprandial responses to standardised meals that consisted of foods that may not reflect usual dietary intake in South Asians; thus, the findings may lack ecological validity. The COVID-19 pandemic also caused data collection to be suspended, meaning that there were not sufficient participants to examine a condition x weight status interaction. This should be explored in the future to provide definitive conclusions regarding the effects of interrupting sitting across South Asians of differing weight status. Finally, the cardiometabolic health benefits of interrupting sitting were not directly compared to other ethnic groups (e.g., Caucasians). Thus, future research should investigate the interacting effects of interrupting sitting in participants with normal-weight and overweight/obesity across different ethnic groups.
Conclusion
Interrupted sitting with 5-min bouts of light walking every 30-min acutely attenuated postprandial glucose, TAG and MLI in South Asians with overweight/obesity. In normal-weight South Asians, there was less widespread cardiometabolic health benefits from this type of acute intervention. Resting energy expenditure from both carbohydrate and fat oxidation was increased with light walking bouts only in participants living with overweight/obesity. Future research should examine the effectiveness of interrupting sitting in free-living settings and over the longer term in South Asians to inform potential public health intervention targets for this ethnic group.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- SIT:
-
Prolonged sitting
- INT-SIT:
-
Interrupted sitting
- iAUC:
-
Incremental area under the curve
- REE:
-
Resting energy expenditure
- TAG:
-
Triglycerides
- MLI:
-
Metabolic load index
- CVD:
-
Cardiovascular disease
- CONSORT:
-
Consolidated Standards of Reporting Trials
- BP:
-
Blood pressure
- HR:
-
Heart rate
- RPE:
-
Borg rating of perceived exertion
- GI:
-
Glycaemic index
- tAUC:
-
Total area under the curve
- p-iAUC:
-
Positive incremental area under the curve
- MAP:
-
Mean arterial pressure
- CI:
-
Confidential interval
References
Abdullah A, Peeters A, de Courten M, Stoelwinder J (2010) The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 89:309–319
Ahmad S, Shanmugasegaram S, Walker KL, Prince SA (2017) Examining sedentary time as a risk factor for cardiometabolic diseases and their markers in South Asian adults: a systematic review. Int J Public Health 62:503–515
Altenburg TM, Rotteveel J, Dunstan DW, Salmon J, Chinapaw MJ (2013) The effect of interrupting prolonged sitting time with short, hourly, moderate-intensity cycling bouts on cardiometabolic risk factors in healthy, young adults. J Appl Physiol 115:1751–1756
Atkinson FS, Foster-Powell K, Brand-Miller JC (2008) International tables of glycemic index and glycemic load values: 2008. Diabetes Care 31:2281–2283
Augustin LS, Kendall CW, Jenkins DJ, Willett WC, Astrup A, Barclay AW, Björck I, Brand-Miller JC, Brighenti F, Buyken AE (2015) Glycemic index, glycemic load and glycemic response: an International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr Metab Cardiovasc Dis 25:795–815
Bailey DP, Locke CD (2015) Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J Sci Med Sport 18:294–298
Bailey DP, Maylor BD, Orton CJ, Zakrzewski-Fruer JK (2017) Effects of breaking up prolonged sitting following low and high glycaemic index breakfast consumption on glucose and insulin concentrations. Eur J Appl Physiol 117:1299–1307
Bailey DP, Hewson DJ, Champion RB, Sayegh SM (2019) Sitting time and risk of cardiovascular disease and diabetes: a systematic review and meta-analysis. Am J Prev Med 57:408–416
Barone Gibbs B, Kowalsky RJ, Perdomo SJ, Taormina JM, Balzer JR, Jakicic JM (2017) Effect of alternating standing and sitting on blood pressure and pulse wave velocity during a simulated workday in adults with overweight/obesity. J Hypertens 35:2411–2418
Bays HE, Shrestha A, Niranjan V, Khanna M, Kambhamettu L (2022) Obesity Pillars roundtable: Obesity and South Asians. Obesity Pillars 1:100006
Bell AC, Richards J, Zakrzewski-Fruer JK, Smith LR, Bailey DP (2023) Sedentary Behaviour-A Target for the Prevention and Management of Cardiovascular Disease. Int J Environ Res Public Health 20:532
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Bowden Davies KA, Pickles S, Sprung VS, Kemp GJ, Alam U, Moore DR, Tahrani AA, Cuthbertson DJ (2019) Reduced physical activity in young and older adults: metabolic and musculoskeletal implications. Ther Adv Endocrinol Metab 10:2042018819888824
Champion RB, Smith LR, Smith J, Hirlav B, Maylor BD, White SL, Bailey DP (2018) Reducing prolonged sedentary time using a treadmill desk acutely improves cardiometabolic risk markers in male and female adults. J Sports Sci 36:2484–2491
Charlett OP, Morari V, Bailey DP (2021) Impaired postprandial glucose and no improvement in other cardiometabolic responses or cognitive function by breaking up sitting with bodyweight resistance exercises: a randomised crossover trial. J Sports Sci 39:792–800
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale, NJ
Curran F, Davis ME, Murphy K, Tersigni N, King A, Ngo N, O’Donoghue G (2023) Correlates of physical activity and sedentary behavior in adults living with overweight and obesity: A systematic review. Obes Rev 24:e13615
DeMers D, Wachs D (2019) Physiology, mean arterial pressure. StatPearls Publishing, Treasure Island
Dempsey PC, Larsen RN, Sethi P, Sacre JW, Straznicky NE, Cohen ND, Cerin E, Lambert GW, Owen N, Kingwell BA, Dunstan DW (2016) Benefits for Type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Diabetes Care 39:964–972
Dey KC, Zakrzewski-Fruer JK, Smith LR, Jones RL, Bailey DP (2021) The Prevalence of Daily Sedentary Time in South Asian Adults: A Systematic Review. Int J Environ Res Public Health 18:9275
Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, Shaw JE, Bertovic DA, Zimmet PZ, Salmon J, Owen N (2012) Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care 35:976–983
Einarson TR, Machado M, Henk Hemels ME (2011) Blood glucose and subsequent cardiovascular disease: update of a meta-analysis. Curr Med Res Opin 27:2155–2163
Ekmekcioglu C, Touitou Y (2011) Chronobiological aspects of food intake and metabolism and their relevance on energy balance and weight regulation. Obes Rev 12:14–25
Emerson SR, Haub MD, Teeman CS, Kurti SP, Rosenkranz SK (2016) Summation of blood glucose and TAG to characterise the ‘metabolic load index. Br J Nutr 116:1553–1563
Frayn KN (1983) Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol Respir Environ Exerc Physiol 55:628–634
Gibbs BB, Gabriel KP, Carnethon MR, Gary-Webb T, Jakicic JM, Rana JS, Lewis CE (2017) Sedentary time, physical activity, and adiposity: cross-sectional and longitudinal associations in CARDIA. Am J Prev Med 53:764–771
Gondim OS, Camargo VTND, Gutierrez FA, Martins PFDO, Passos MEP, Momesso CM, Santos VC, Gorjão R, Pithon-Curi TC, Cury-Boaventura MF (2015) Benefits of regular exercise on inflammatory and cardiovascular risk markers in normal weight, overweight and obese adults. PLoS ONE 10:e0140596
Gray LJ, Yates T, Davies MJ, Brady E, Webb DR, Sattar N, Khunti K (2011) Defining obesity cut-off points for migrant South Asians. PLoS ONE 6:e26464
Hanif RW, Susarla R (2018) Diabetes and cardiovascular risk in UK South Asians: an overview. Br J Cardiol 25:S8–S13
Hansen RK, Andersen JB, Vinther AS, Pielmeier U, Larsen RG (2016) Breaking up prolonged sitting does not alter postprandial glycemia in young, normal-weight men and women. Int J Sports Med 37:1097–1102
Hawari NS, Al-Shayji I, Wilson J, Gill JM (2016) Frequency of breaks in sedentary time and postprandial metabolic responses. Med Sci Sports Exerc 48:2495–2502
Hawari NS, Wilson J, Gill JM (2019) Effects of breaking up sedentary time with “chair squats” on postprandial metabolism. J Sports Sci 37:331–338
Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N (2011) Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J 32:590–597
Henson J, Davies MJ, Bodicoat DH, Edwardson CL, Gill JM, Stensel DJ, Tolfrey K, Dunstan DW, Khunti K, Yates T (2016) Breaking Up Prolonged Sitting with Standing or Walking Attenuates the Postprandial Metabolic Response in Postmenopausal Women: A Randomized Acute Study. Diabetes Care 39:130–138
Jalal Z, Antoniou S, Taylor D, Paudyal V, Finlay K, Smith F (2019) South Asians living in the UK and adherence to coronary heart disease medication: a mixed-method study. Int J Clin Pharm 41:122–130
Larsen R, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW (2014) Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis 24:976–982
Larsen RN, Kingwell BA, Robinson C, Hammond L, Cerin E, Shaw JE, Healy GN, Hamilton MT, Owen N, Dunstan DW (2015) Breaking up of prolonged sitting over three days sustains, but does not enhance, lowering of postprandial plasma glucose and insulin in overweight and obese adults. Clin Sci 129:117–127
Larsen RN, Dempsey PC, Dillon F, Grace M, Kingwell BA, Owen N, Dunstan DW (2017) Does the type of activity “break” from prolonged sitting differentially impact on postprandial blood glucose reductions? An exploratory analysis. Appl Physiol Nutr Metab 42:897–900
Lohman TG, Roche AF, Martorell R (1988) Anthropometric standardization reference manual. Human kinetics books Champaign.
Mattes RD, Campbell WW (2009) Effects of food form and timing of ingestion on appetite and energy intake in lean young adults and in young adults with obesity. J Am Diet Assoc 109:430–437
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO (1990) A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 51:241–247
Mikines KJ, Sonne B, Farrell PA, Tronier B, Galbo H (1988) Effect of physical exercise on sensitivity and responsiveness to insulin in humans. Am J Physiol 254:E248–E259
Misra A, Khurana L (2011) Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes 35:167–187
Miyashita M, Burns SF, Stensel DJ (2006) Exercise and postprandial lipemia: effect of continuous compared with intermittent activity patterns. Am J Clin Nutr 83:24–29
Miyashita M, Edamoto K, Kidokoro T, Yanaoka T, Kashiwabara K, Takahashi M, Burns S (2015) Interrupting sitting time with regular walks attenuates postprandial triglycerides. Int J Sports Med 28:97–103
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2012) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg 10:28–55
O’Keefe JH, Bell DS (2007) Postprandial hyperglycemia/hyperlipidemia (postprandial dysmetabolism) is a cardiovascular risk factor. Am J Cardiol 100:899–904
Patterson R, McNamara E, Tainio M, de Sá TH, Smith AD, Sharp SJ, Edwards P, Woodcock J, Brage S, Wijndaele K (2018) Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol 33:811–829
Peddie MC, Bone JL, Rehrer NJ, Skeaff CM, Gray AR, Perry TL (2013) Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: a randomized crossover trial. Am J Clin Nutr 98:358–366
Pulido JME, Salazar MA (1999) Changes in insulin sensitivity, secretion and glucose effectiveness during menstrual cycle. Arch Med Res 30:19–22
Pulsford RM, Blackwell J, Hillsdon M, Kos K (2017) Intermittent walking, but not standing, improves postprandial insulin and glucose relative to sustained sitting: a randomised cross-over study in inactive middle-aged men. J Sci Med Sport 20:278–283
Sattar N, Gill JM (2015) Type 2 diabetes in migrant south Asians: mechanisms, mitigation, and management. Lancet Diabetes Endocrinol 3:1004–1016
The World Bank Group (2021) The total population of South Asian region. https://data.worldbank.org/region/south-asia. Accessed 22 September 2021.
Van Dyck D, Cerin E, De Bourdeaudhuij I, Hinckson E, Reis RS, Davey R, Sarmiento OL, Mitas J, Troelsen J, MacFarlane D, Salvo D, Aguinaga-Ontoso I, Owen N, Cain K, Sallis JF (2015) International study of objectively measured physical activity and sedentary time with body mass index and obesity: IPEN adult study. Int J Obes 39:199–207
Wolever TM, Jenkins DJ (1986) The use of the glycémie index in predicting the blood glucose response to mixed meals. Am J Clin Nutr 43:167–172
Yates T, Edwardson CL, Celis-Morales C, Biddle SJ, Bodicoat D, Davies MJ, Esliger D, Henson J, Kazi A, Khunti K (2020) Metabolic effects of breaking prolonged sitting with standing or light walking in older South Asians and white Europeans: a randomized acute study. J Gerontol A Biol Sci Med Sci: Series A 75:139–146
Acknowledgements
The authors would like to thank all individuals who volunteered their time to participate in this study.
Author information
Authors and Affiliations
Contributions
The experimental study was designed by KCD, JKZF, LRS, RLJ and DPB. KCD conducted the study protocols including participant recruitment, screening, data collection and data analysis. KCD prepared the first draft of the manuscript. All authors contributed to data interpretation and critical review of the manuscript. The final version of the manuscript was approved by all authors.
Corresponding authors
Ethics declarations
Conflict of interest:
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Ethical approval was obtained before starting the study (Approval number: 2019ISPAR003).
Additional information
Communicated by Philip D. Chilibeck.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dey, K.C., Zakrzewski-Fruer, J.K., Smith, L.R. et al. Interrupting sitting acutely attenuates cardiometabolic risk markers in South Asian adults living with overweight and obesity. Eur J Appl Physiol 124, 1163–1174 (2024). https://doi.org/10.1007/s00421-023-05345-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-023-05345-7