Abstract
Purpose
Divers can experience cognitive impairment due to inert gas narcosis (IGN) at depth. Brain-derived neurotrophic factor (BDNF) rules neuronal connectivity/metabolism to maintain cognitive function and protect tissues against oxidative stress (OxS). Dopamine and glutamate enhance BDNF bioavailability. Thus, we hypothesized that lower circulating BDNF levels (via lessened dopamine and/or glutamate release) underpin IGN in divers, while testing if BDNF loss is associated with increased OxS.
Methods
To mimic IGN, we administered a deep narcosis test via a dry dive test (DDT) at 48 msw in a multiplace hyperbaric chamber to six well-trained divers. We collected: (1) saliva samples before DDT (T0), 25 msw (descending, T1), 48 msw (depth, T2), 25 msw (ascending, T3), 10 min after decompression (T4) to dopamine and/or reactive oxygen species (ROS) levels; (2) blood and urine samples at T0 and T4 for OxS too. We administered cognitive tests at T0, T2, and re-evaluated the divers at T4.
Results
At 48 msw, all subjects experienced IGN, as revealed by the cognitive test failure. Dopamine and total antioxidant capacity (TAC) reached a nadir at T2 when ROS emission was maximal. At decompression (T4), a marked drop of BDNF/glutamate content was evidenced, coinciding with a persisting decline in dopamine and cognitive capacity.
Conclusions
Divers encounter IGN at – 48 msw, exhibiting a marked loss in circulating dopamine levels, likely accounting for BDNF-dependent impairment of mental capacity and heightened OxS. The decline in dopamine and BDNF appears to persist at decompression; thus, boosting dopamine/BDNF signaling via pharmacological or other intervention types might attenuate IGN in deep dives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diving at great depths (or the permanence at high pressures) induces some peculiar perturbations in the cognitive domain. This evidence dates back to 1935 when Behnke and colleagues first associated this phenomenon with increased inert gas accumulation, mainly N2 (Grover et al. 2014). Now, we know that pressures greater than 4 absolute atmospheres (ATA) (30 m of seawater (msw) = partial N2 pressure of ≅ 3.1 ATA) can usher in inert gas narcosis (nitrogen narcosis, IGN). IGN is a reversible change in consciousness that occurs while diving at deep depths. Certain gases at high pressure cause an anesthetic effect that alters a diver's consciousness (Kirkland et al. 2021; Moon et al. 2009; Vann et al. 2011).
IGN encompasses subjective and objective mental disturbance (Clark 2015) and can manifest during self-contained underwater breathing apparatus (SCUBA) diving. Since divers inhale gas mixtures at different pressures, in theory, and practice, IGN could be blunted by using N2-deprived gas mixtures, such as helium–oxygen (Bennett et al. 1975; Gelfand et al. 1983; Kirkland et al. 2021). However, elite breath-hold divers can reach extreme depths nowadays, and they also report IGN symptoms when trying to stretch their limits in record-breaking dives (Freiberger et al. 2016; Lindholm et al. 2009). Hence, factors accounting for IGN genesis remain worth investigating.
IGN can impair cognitive functions and physical performance from depths as low as 10 m, becoming more apparent at 30–40 m depth (Rostain et al. 2011), and it remains one of the leading causes of underwater accidents (Unsworth 1966; Ranapurwala et al. 2014; Clark 2015). Importantly, IGN occurs especially during recreational diving at depths greater than 40 msw (Vann et al. 2011). Clinically, it includes several psychomotor disorders, with reversible alterations (Turle et al. 1998). Its symptoms closely resemble the cognitive, neuromuscular, and vestibular alterations experienced by subjects drinking alcohol, being mild and benign at shallow depths and more severe and debilitating when divers go deeper (Clark 2015). The Meyer–Overton hypothesis is at the roots of IGN neurochemistry; this hypothesis is based on the correlation between anesthetic potency and lipid solubility, and the anesthetic potency is proportional to the lipid/water partition coefficient (Meyer 1899; Overton & Lipnick 1991). Furthermore, the lipid solubility of inert gases is one of its key postulations (Bennett et al. 1989; Rostain et al. 2011). However, this rule suffers from several weaknesses; in fact, stereoisomers of an anesthetic can have very different narcotic potency, even though their oil/gas partition coefficients are similar (Cameron 2006).
Over the years, IGN pathogenesis has been linked to alterations in GABAa and glutamatergic NMDA neuronal receptors systems (Rostain et al. 2016). For example, changes in the extracellular concentrations of GABA have also been described during exposure to hyperbaric oxygen (HBO2) at 5 ATA (Zhang et al. 2004). Similarly, declines in norepinephrine (NE) and dopamine (DA) release occur in the rat caudate nucleus and hypothalamus after exposure to a nitrogen–oxygen mixture at 20 ATA (McLeod et al. 1988). Nevertheless, all this evidence always comes from the rat and/or scuba and technical divers (Yang et al. 2002; Rocco et al. 2019).
Ambient pressure increases by one ATA at depth every 10 msw; therefore, a hyperbaric chamber approach can conveniently circumvent these hurdles. Indeed, it allows higher concentrations of gases to be inhaled and dissolved into cells, membranes, and body fluids under dry conditions, de facto mimicking what occurs in deep divers in the sea.
Brain-derived neurotrophic factor (BDNF) is essential for neuronal growth, differentiation, and connectivity, acting as an on-demand tissue protectant under stress conditions (Agrimi et al. 2019; Kowianski et al. 2018; Rothman et al. 2013). It—directly or indirectly (via glutamate excitatory neurotransmission)—preserves cognitive function (Benarroch et al. 2015; Miranda et al. 2019). BDNF is also vital in maintaining normal cardiac contraction and relaxation (Agrimi et al. 2019; Feng et al. 2015) and shields tissues against oxidative stress. For instance, in schizophrenic patients, a marked decline in circulating BDNF levels correlates with low levels of antioxidants, such as superoxide dismutase and glutathione peroxidase, and with a substantial rise in malondialdehyde (MDA) and end products of lipid peroxidation (Zhang et al. 2015). Finally, many neurotransmitters, including dopamine and glutamate can enhance BDNF bioavailability in neurons (Bagayogo et al. 2009; Kuppers et al. 2001). On these grounds, we enrolled healthy (highly experienced) divers and subjected them to a simulated dive to 48 msw (5.8 ATA) inside a hyperbaric chamber to test the following three new hypotheses. First, IGN narcosis stems, at least in part, from the lack of circulating BDNF. Second, this loss is attributable to a lack of BDNF-releasing neurotransmitters, such as dopamine and glutamate; third, impoverished levels of systemic and likely local pools of BDNF contribute to heightening oxidative stress in deep divers. Ultimately, all events would drive cognitive impairment in divers at depth.
Materials and methods
We performed the current observational study employing a dry dive test at 5.8 ATA—a depth narcosis induction test—at the ATIP hyperbaric facility in a hyperbaric multiplace chamber VECOM, Padova (Italy).
Selections of participants
We enrolled in the protocol six well-trained scuba and breath-hold divers, with more than 5 years of high-level experience, (four males, two females): age (43.5 ± 14.6 yrs), height (174.5 ± 6.7 cm), weight (68.5 ± 12.3 kg) e BMI (22.4 ± 3.1 kg.m−2) (mean ± SD). Exclusion criteria were: pregnancy, smoking, alcohol, drugs, vitamin/minerals/herbs/antioxidant supplements, exercise/training in the pre-test week, and/or a SCUBA dive made within 2 weeks before the experiment.
Ethical considerations
The subjects were recruited voluntarily (no incentives were provided to the participants) and they signed a written informed consent form. The experimental protocol was approved by the Ethical Committee of the University of Milan (Aut. #37/17) and adhered to the principles of the Declaration of Helsinki.
Experimental protocol
On the day of the experiment, the included subjects underwent a general medical screening, anthropometric measurements, a first set of biological samplings (blood, urine, and saliva) and cognitive tests to assess their basal status (T0). Then, the participants were compressed in a hyperbaric chamber to a depth of − 48 msw (157.48 feet), breathing room air. An anesthesiologist accompanied the subjects inside the chamber to assist in case of medical issues. Saliva samples were also obtained inside the chamber at 25 msw descending (T1), at the bottom, 48 msw (T2), and 25 msw ascending (T3). Once at depth, subjects performed cognitive tests. Then, they were progressively decompressed to the surface in 45 min (Fig. 1), breathing oxygen from 12 m to the surface. Ten minutes after the end of the compression, another set of samples (blood, urine, and saliva) and cognitive tests were obtained from each subject (T4).
Cognitive tests
To determine whether the enrolled divers can experience IGN when at depth (48 msw) in the hyperbaric chamber, thus to validate our methodological application, we administered two psycho-aptitude tests on functional domains as per visuospatial abilities and executive functions (Hegarthy et al. 2005): the intuitive geometric constructions and the labyrinth (Miyake et al. 2000, 2001; Predovan et al. 2021). These tests were administered to the diver volunteers before (T0), at the bottom of the dive (T2), and at the time of surfacing (T4). Spatial ability is the capacity to understand and remember the spatial relations among objects. In a spatial ability test (also called spatial reasoning test), the tested person is required to draw two-dimensional and three-dimensional figures by connecting the dots (Miyake et al. 2000, set of paper-and-pencil tests of spatial abilities that load on three correlated, but distinguishable factors: spatial visualization, spatial relations, and perceptual speed). Executive functions are required when the behavior or information processing is not automated and requires some control. This control may be necessary because of the unpredictability of the situation (Predovan et al. 2021). Labyrinth testing is structured as a nonverbal intellectual level test. The test consists of a series of mazes that the subject has to solve. The labyrinths are of varying complexity. The test lasts 15–60 s, allowing the subject to solve as many mazes as possible.
The participants were provided with different tests each time, so there was no possibility of 'learning' or 'condition' or 'difficulty' level impacting test performance.
Blood, urine, and saliva sample collection
Approximately, 9 ml of venous blood was drawn from an antecubital vein, with subjects sitting or lying on a bed. Each time, samples to assess oxidative stress were collected in lithium-heparinized and EDTA tubes (Vacutainer, Becton Dickinson, USA). Plasma was separated by centrifuge (5702R, Eppendorf, Germany) at 3500g × 10 min at 4 °C. Samples of plasma and erythrocytes were then stored in multiple aliquots at − 80 °C until assayed. Samples were thawed only once before analysis, performed within 1 month from the collection. Urine was collected by voluntary voiding in a sterile container and stored in multiple aliquots at − 20 °C until assayed and thawed only before analysis. Blood and urine samples were collected at pre- and post-hyperbaric chambers. Approximately, 1 mL of saliva was obtained by Salivette devices (Sarstedt, Nümbrecht, Germany). The subjects were instructed on the correct use (i.e., no eating, drinking, or oral intake of drugs 1 h before sample collection) (Mrakic-Sposta et al. 2020). Saliva samples were collected before DDT (T0), at 25 msw (descending, T1), 48 msw (depth, T2), and 25 msw (ascending, T3), and 10 min after decompression (T4). Salivettes were centrifuged at 1500g × 20 min at 4 °C and retrieved saliva was transferred, and aliquoted, then stored at − 80 °C until assayed and thawed only once before analysis.
Assessment of circulating BDNF, glutamate, and dopamine levels
BDNF was detected using the ELISA method according to the manufacturer's instructions (Human BDNF ELISA kit, Abcam, USA). Tertiary antibodies were conjugated to horseradish peroxidase. Wells were developed with tetramethylbenzidine and measured at 450. BDNF content was quantified against a standard curve calibrated with known amounts of protein. The detection limits were 2.4 pg.mL−1. Measurements were performed in duplicate and are expressed as ng.mL−1. According to the manufacturer's instructions, glutamate concentrations were measured using an assay kit (Glutamate ELISA KIT, LDN, Germany). Detection limits were 0.3 μg.mL−1. The amount of glutamate was quantified by colorimetric spectrophotometry at 450 nm against a standard curve. Measurements were performed in duplicate and are expressed as μM.L−1 according to the manufacturer's conversion suggested. Dopamine in plasma and saliva was determined by a kit (cat. no. EU0392; FineTest, Wuhan, China) based on a competitive ELISA detection method, sensitivity 0.938 ng.mL−1. Analysis was carried out according to the manufacturer's instructions. Dopamine concentration was determined using a standard curve. Samples and standards were read spectrophotometrically at a wavelength of 450 nm and concentrations are expressed in ng.mL−1.
Oxidative stress
-
1)
Reactive oxygen species (ROS) and antioxidant capacity (TAC) by electron paramagnetic resonance (EPR) in plasma and saliva
We used electron paramagnetic resonance (EPR) spectroscopy X-band (E-Scan-Bruker BioSpin, GmbH, MA USA) to assess total ROS production and total antioxidant capacity (TAC) before and after the dry dive session (from blood samples), as well as their kinetics during timeline: at baseline (T0), descending at 25 msw (T1), depth 48 (T2), in ascending, at 25 msw (T3) and at the end (T4), using the saliva of the enrolled highly trained divers, according to previously described methods (Mrakic-Sposta et al. 2014; 2019; 2020; 2022; Bosco et al, 2018a; 2021). CMH (1-hydroxy-3-methoxycarbonyl-2,2,5,5-tetramethylpyrrolidine) spin trap probe was used for ROS determination in both fluids. A stable radical CP· (3-carboxy2,2,5,5-tetramethyl-1-pyrrolidinyloxy) was used as an external reference to convert ROS determinations into absolute quantitative values (μmol.min−1). TAC was measured using 1,1-diphenyl-2-picrylhydrazyl (DPPH•) quenching, in both fluids (plasma and saliva) (Mrakic-Sposta et al. 2019; 2020; Giacon et al. 2021). The calculated antioxidant capacity was expressed in terms of Trolox equivalent antioxidant capacity (TAC, mM). Samples were stabilized at 37 °C with "Bio III" unit, interfaced with the spectrometer.
-
2)
8-isoprostane in urine
As a marker of oxidative stress in the urine, we measured 8-isoprostane concentration (8-iso-PGF2α) by an immunoassay kit (Cayman Chemical, Ann Arbor, MI, USA) as previously described (Mrakic-Sposta et al. 2014; Bosco et al. 2019; 2021). Samples were read spectrophotometrically at a wavelength of 512 nm.
Nitric oxide pathway
Nitrite and nitrate (NO−2, NO−3) are the end products of NO. oxidation pathway. NO. metabolites (NO2, + NO3 = NOx) were determined in urine via a colorimetric method based on the Griess reaction, using a commercial kit (Cayman Chemical, Ann Arbor, MI, USA) described (Green et al. 1982; Mrakic-Sposta et al. 2019; Niu et al. 2012). Samples were read at 545 nm and the concentration was assessed by a standard curve. Inducible nitric oxide synthase (iNOS) expression in plasma was determined using a human NOS2/iNOS ELISA kit (cat. no. EH0556; FineTest, Wuhan, China). This assay was based on sandwich enzyme-linked immune-sorbent assay technology. NOS2/iNOS protein synthesis was determined using a standard curve. Samples and standards were read at a wavelength of 450 nm, and the analysis was carried out according to the manufacturer's instructions.
All samples were read in duplicate and the immune-enzymatic determinations were performed by a spectrophotometer microplate reader (Infinite M200, Tecan Group Ltd., Männedorf, Switzerland).
Thiols
Total (tot) aminothiols (Cys: cysteine; CysGly: cysteinyl glycine; Hcy: homocysteine; and GSH: glutathione) were measured in red blood cells according to previously validated methods (Dellanoce et al. 2014; Vezzoli et al. 2016). Briefly, thiol separation was performed at room temperature by isocratic HPLC analysis on a Discovery C-18 column (250 × 4.6 mm I.D, Supelco, Sigma-Aldrich, St. Louis, MOS, USA), eluted with a solution of 0.1 M acetate buffer, pH 4.0: methanol, 81:19 (v/v), at a flow rate of 1 mL.min−1. Fluorescence intensities were measured with an excitation wavelength at 390 nm and an emission wavelength at 510 nm, using a fluorescence spectrophotometer (Jasco, Japan). A standard calibration curve was used.
Creatinine, neopterin, and uric acid concentration
Creatinine and neopterin concentrations were measured using high-pressure liquid chromatography (HPLC), as described (Mrakic-Sposta et al. 2019; Vezzoli et al. 2016). A Varian instrument (pump 240, autosampler ProStar 410) determined uric acid levels coupled to a UV–VIS detector (Shimadzu SPD 10-AV, λ = 240 nm) after centrifugation at 13,000 rpm for 5 min at 4 °C. Analytic separations were performed at 50 °C on a 5 µm Discovery C18 analytical column (250 × 4.6 mm I.D., Supelco, Sigma-Aldrich) at a 0.9 mL.min−1 flow rate. The calibration curves were linear over the range of 0.125–1 μmol.L−1, 0.625–20 mmol.L−1, and 1.25–10 mmol.L−1 for neopterin, uric acid, and creatinine levels, respectively. Inter-assay and intra-assay coefficients of variation were < 5%.
Data collection and analysis
Data were analyzed using the GraphPad Prism package (GraphPad Prism 9.3.0, GraphPad software Inc., San Diego, CA) and SPSS Statistics (SPSS version 25, IBM). Kolmogorov–Smirnov testing was utilized to determine the distribution of each data set. Data were analyzed with a non-parametric test; Wilcoxon matched-pair test was used to compare the values of the assessed biomarkers at the pre- (T0) versus post-hyperbaric chamber (T4). Kinetics (from T0 to T4) by saliva samples were compared by ANOVA repeated measures, followed by Tukey's multiple comparison test to further check the groups' significance; also cognitive tests were analyzed by ANOVA and post hoc test. Spearman product–moment correlation coefficient (r) with 95% confidence intervals (CI) was used to show up possible relationships between selected parameters. Finally, the phi coefficient (ϕ) was used to evaluate the association. All data are presented as mean ± SD, and significance was determined at p < 0.05.
Results
Reaching -48msw in the hyperbaric chamber triggers IGN-like effects in healthy divers
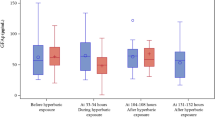
In scuba divers, IGN can impair several cognitive domains (Binder et al. 2004; Martin et al. 2011; Rocco et al. 2019; Karakaya et al. 2021). Yet, what specific executive functions and neurotransmitter levels are eventually altered during and after narcosis in-depth remain to be fully deciphered. To fill this gap, we subjected the enrolled highly trained divers to a dry hyperbaric chamber diving approach to mimic a real-life "wet" IGN scenario, administering the labyrinth and Porteous tests to evaluate their cognitive functions (Miyake et al. 2000; Predovan et al. 2021). As shown in Fig. 2A, B, nitrogen narcosis at 48 msw (500 kPa) pressure in the dry hyperbaric chamber had a mild-to-moderate negative effect on divers' cognitive performance. In particular, we recorded a significant decrease (p < 0.05) in labyrinth test score Fig. 2A and a similar (with an increase 20% at T4 and T2) tendency in the picture construction test score Fig. 2B.
Bar charts (mean ± SD) of A labyrinth test score), B picture construction test score, at T0, T2, and T4; C BDNF, D glutamate, and E dopamine concentration in plasma collected at T0 and T4. Time course of F dopamine concentration in saliva at T0, T1, T2, T3, and T4. *p < 0.05, **p < 0.01 significantly different
BDNF, dopamine, and glutamate levels are reduced during a dry dive test in healthy divers
BDNF is essential for the survival and differentiation of neurons in the peripheral and central nervous systems (CNS) (Binder et al. 2004; Kowianski et al. 2018). We found that BDNF, glutamate, and dopamine plasma levels are markedly decreased in healthy highly trained divers subjected to a dry dive test at 48 msw. BDNF declined from 5.16 ± 0.87 (T0) to 2.81 ± 1.48 ng.mL−1 (T4), while glutamate dropped from 80.59 ± 11.97 to 52.22 ± 7.17 μM.L−1 and dopamine from 35.14 ± 3.61 to 27.20 ± 3.55 ng.mL−1 (all p < 0.05, Fig. 2C, D and E). Furthermore, significant differences in the saliva levels of dopamine were also found. As depicted in Fig. 2F, dopamine levels were peaking at T0 (7.47 ± 1.43 ng.mL−1) and plummeted over the sampling period. In detail, dopamine decreased, reaching the lowest peak value at depth (T2: 3.29 ± 0.93 ng.mL−1) and remaining low at T3 and T4 (T3: 3.49 ± 1.10; T4: 5.16 ± 1.19 ng.mL−1).
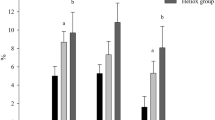
A dry dive test triggers ROS production, while depleting antioxidant capacity in healthy divers’ saliva and blood, respectively
Under normal physiological conditions, approximately 1.2% of inspired O2 is converted to reactive oxygen species (ROS), and hyperoxia increases this amount (Bruakk et al. 2014). As shown in Fig. 3A, plasma ROS emission rose substantially after the dry dive test: from 0.18 ± 0.01 (T0) to 0.25 ± 0.024 µmol.min−1 (T4). The saliva-based EPR approach adopted allowed to follow the kinetics of ROS production (Fig. 3B). Representative pre- and post-test EPR spectra are shown in Fig. 3C. With this tool in hand, we found that, as compared to baseline values (T0: 0.19 ± 0.01 µmol.min−1), ROS production rate markedly increased (range p = 0.05–0.01) during the dry dive test, reaching a peak value at a depth of − 48 msw (T2: 0.49 ± 0.11 µmol.min−1; p < 0.01) while declining at − 25 msw (T3: 0.39 ± 0.09 µmol.min−1). Yet, this burst remained significantly above T0 value values when reaching T4 (0.32 ± 0.06 µmol.min−1).
Bar chart (mean ± SD) of A ROS production rate. B Time course of ROS production rate. C Stacked plots of the EPR spectra show an increase of the signal amplitude (a. u.) at T4 (blu lines) with respect to T0 (black lines). The spectra are centered at g = 1.997. *p < 0.05 and **p < 0.0 are significantly different. D Bar chart of total antioxidant capacity (TAC). E Time course of total antioxidant capacity in saliva at T0, T1, T2, T3, and T4. F Bar chart of lipid peroxidation (8-isoprostane) in plasma collected at T0 and T4
Antioxidant defenses are up-regulated in response to ROS production, and recent studies have shown that endogenous antioxidant activity can be enhanced after saturation diving (Bosco et al. 2010; Morabito et al, 2011). Our data show that total antioxidant activity (TAC) declined at T4 as compared to T0, both in plasma (− 11%; Fig. 3D) and saliva samples (− 19%; Fig. 3E). Moreover, following the TAC kinetics, we found that salivary TAC reached a nadir at T2 (1.57 ± 0.25 mM) and T4 (1.52 ± 0.21 mM) with respect to the basal level (T0: 1.91 ± 0.19 mM). Together, these data indicate that a dry test is sufficient to trigger ROS emission in highly trained breath-hold divers that are not immediately countered by a parallel rise in total antioxidant capacity. No significant differences in pre- and post-8-isoPGF2-α concentration (Fig. 3F) were found.
ROS production correlates with bioavailable dopamine decline
We determined whether a correlation exists between the magnitude of ROS emission and dopamine levels after a dry dive test. As shown in Fig. 4A, by considering T0 and T4 times taken all together versus a single specific biomarker, a significant (p < 0.05) linear inverse relationship appears to exist between ROS emission and dopamine levels (r = 0.69; and ϕ = 3.31).
A dry test in the hyperbaric chamber fuels pro-oxidizing and pro-inflammatory conditions in deep divers
As shown above, a dry test can trigger pro-oxidizing conditions in healthy breath-hold divers. Hence, we next interrogated whether the levels of GSH, a primary antioxidant, can underpin, at least in part, the elevated ROS emission found in these divers. Of note, there are no human data in this regard. We found that the GSH levels were significantly (p = 0.05) increased at T4 (Table 1), along with that of homocysteine. Conversely, the concentration of other total aminothiols, such as cysteine and cysteinyl glycine, was not significantly altered in the erythrocytes at post-deep.
Next, we tested whether a dry test (in the hyperbaric chamber) would alter the levels of NO. metabolites in these divers. We observed no differences in urine between T0 and T4 in total oxidized products of NO. (NOx) 391.8 ± 282.7 μM (T0) vs. 375.6 ± 283.2 μM (T4) (Fig. 5A) or nitrite (NO2) 1.41 ± 0.43 (T0) vs. 1.25 ± 0.31 (T4) μM (Fig. 5B), with a significant (p < 0.05) rise in iNOS levels, from 19.65 ± 3.95 (T0) vs 35.79 ± 8.15 IU. mL−1 (T4) (Fig. 5C).
Neopterin and creatinine levels are elevated after a dry dive test
Here, we report, for the first time, that neopterin levels are more elevated at T4 than at T0: 175.0 ± 61.9 vs. 102.6 ± 47.8 (μmol.mol−1creatinine) (Fig. 6A), with an increase in creatinine level at T4 and T0: 0.45 ± 0.24 vs. 0.21 ± 0.09 g.L−1 (Fig. 6B).
Discussion
Hyperbaric oxygen can have toxic effects on the central nervous system (CNS) (Gasier et al. 2017), but the mechanisms whereby narcosis induces cognitive impairment in divers are unclear. The present observational study reveals, for the first time, that, after a dry dive test at depth in a hyperbaric chamber to mimic in-depth sea diving, highly trained divers manifest: (1) cognitive impairment coupled to low circulating and/or saliva content of dopamine, glutamate, and BDNF; (2) overall increased ROS emission paralleled by depleted antioxidant levels; (3) pro-oxidizing and pro-inflammatory conditions likely subtending altered vascular reactivity; and (4) elevated neopterin and homocysteine levels that may account, on the one hand, for the onset of inflammation and loss of BDNF signaling, and thus cognitive deficits, on the other (Fig. 7).
Scheme of deep narcosis test via a dry dive test (DDT) at 48 m in a multiplace hyperbaric chamber. The Inert Gas Narcosis (IGN) consists in a reversible depression of neuronal excitatory signaling - BDNF (−47%), Glutamate (−35%), Dopamine (−23%) -, and an imbalance between ROS and antioxidant defenses (i.e., ROS: +43% and TAC −10%), caused in particular by nitrogen and oxygen breathing at higher partial pressures. The influence on clinical presentation can include decreased cognitive performance. The onset varies, but can be seen around 30 msw or deeper
Narcosis: short-term and long-term consequences
Narcosis-like symptoms could be common and similar between scuba and free divers; for instance, in the latter, it may occur when breath-hold divers exceed ~ 70–90 msw, leading to transient amnesia (Patrician et al. 2021a). Recently, Patrician and colleagues reported that two breath-hold divers spent 26 and 42 s, respectively, beyond 90 msw—with maximum depths of 102 and 117 msw, PAN2 increases with depth, and the total time exposed at these extreme depths appears to play a crucial role in both divers reporting narcosis (Patrician et al. 2021b). Well-trained divers adopt a range of physiological adaptations to overcome the limits; however, these modifications could interfere with some safety mechanisms that grant homeostasis and integrity of the organism (Elia et al. 2021). Long-term consequences of breath-hold diving encompass neurocognitive disorders caused by chronic exposition to hypoxia and subsequent neuroinflammation, aside from other diving-related illnesses such as blood gas embolisms (Elia et al. 2021). For example, memory impairment is not rare in these subjects compared to healthy, age-matched subjects (Billaut et al. 2018). We administered the labyrinth test or Porteus maze test (Miyake et al. 2000; Predovan et al. 2021) in hyperbaric conditions to fill this gap. Thus, the present findings extend recent evidence obtained in SCUBA divers subjected to hyperbaric chamber-simulated depth showing IGN-induced cognitive impairment during a dry dive test (Karakaya et al. 2021), which may threaten the safety of diving. Thus, as articulated above, the extent of achieved bottom depth and the time spent there are primary determinants of the partial pressure of alveolar nitrogen (PAN2), and its inordinate elevation facilitates nitrogen diffusion into the blood (Patrician et al. 2021a).
Especially when recurrent, exposures to narcosis can desensitize GABAA receptors on dopamine cells and decrease glutamate release while increasing the sensitivity of NMDA receptors, resulting in overall neurological toxic effects and motor impairment (Rostain et al. 2016). Of relevance, deficits in cognitive performance in the underwater environment are significantly more frequent in anxious subjects (Hos et al. 2011). Notwithstanding, the reasons accounting for all the phenomena described above remain ill defined. This gap in our knowledge, the consequent lack of potential interventions directed to lower IGN incidence, and the eventual severity of its remote functional and psychological repercussions deserve more investigation. On the one hand, reaching this goal will allow divers to be more focused and efficient in completing the immersion. On the other, increased knowledge and awareness, along with possible chemical or pharmacological interventions directed to attenuate the effects of narcosis will reduce the extent of an athlete's anxiety while performing deep diving and the long-term consequences of recurrent narcosis episodes.
Nitrogen and neurotransmitters during narcosis
According to Henry's law, nitrogen carried from the lungs dissolves in the brain, causing a drunken sensation beyond about 30 m depth. Nitrogen concentrations alter neuronal or synaptic transmission, causing impaired cognitive function, euphoria, slowing of reflexes, and stupor (Fitz-Clarke 2018). Glutamate is the major excitatory neurotransmitter in the brain (Petroff 2002). Our present data show that glutamate release is significantly decreased at T4 (− 35%). Glutamate stimulates the production of BDNF, which, in turn, modifies neuronal glutamate sensitivity, Ca2+ homeostasis, and plasticity (Mattson 2008). Besides trophic actions, BDNF affects synaptic transmission and plasticity, enhancing excitatory synaptic transmission through pre- and postsynaptic mechanisms, partially via augmented glutamate release (Martin et al. 2011). Vallee and colleagues (2009) have shown that nitrogen reduces the extent of glutamate and other amino acids in the striatum of rats compressed up to 0.1 Mpa at a rate of 0.01 Mpa/min and then up to 3 Mpa at a rate of 0.1 Mpa/min in a hyperbaric chamber, accounting for IGN-motor and cognitive disturbances in nitrogen narcosis (Valee et al. 2009). Yet, whether circulating BDNF levels are altered in IGN-experiencing subjects remains to be tested. Moreover, lack of dopamine and glutamate stimulation can account, at least in part, for low levels of systemic BDNF in divers at the depth. This, in turn, may contribute to altered synaptic transmission, and thus cognitive impairment in divers at the depth, in agreement with that previously found both experimentally and in humans (Yang et al. 2002; Rostain et al. 2011). In our study, we found that a correlation exists between BDNF and glutamate levels, and this evidence goes hand in hand with the fact that the excitatory neurotransmitter glutamate and BDNF are chiefly involved in the phenomena of cellular and synaptic plasticity (Gulyaeva 2017). More specifically, our present findings help explain recent evidence showing that repeated dives, even when compliant with the most up-to-date decompression tables, can progressively lead to micro-lesions in the myelin sheet, thus accounting for altered result's neuronal function (Coco et al. 2019). In the same vein, current data concerning dopamine serve two mechanistic purposes. First, they lend support to the concept that dopamine could influence BDNF levels. Dopamine enhances BDNF protein levels, and the mRNA gene transcripts for its specific receptor, tropomyosin receptor kinase B (TrkB), in neuronal and astroglia cultures of the mouse striatum (Kuppers et al. 2001); indeed, stimulating these neurons with dopamine or a dopamine D1 receptor agonist elevates their BDNF content, suggesting that dopamine effects on GABAergic cells can intersect with BDNF action (Kuppers et al. 2001). Moreover, the overall deficit in BDNF levels can lead to an imbalance in excitatory/inhibitory neurotransmission, including dysregulation of GABAergic transmission, ultimately leading to neurodegeneration (Kim et al. 2017). Second, constitutive low BDNF levels selectively alter serotonergic neurotransmission in the hippocampus via a reduced expression, and thus the function of the serotonin reuptake transporter, SERT, leading to an hyperserotoninergic phenotype (Guiard et al. 2008). There is evidence that antidepressants, such as selective serotonin uptake inhibitors (SSRIs), can increase the incidence of narcosis (Querido 2017).
Nitrogen and hyperoxia during narcosis
Hyperbaric hyperoxia with challenging variations in PO2 can develop inflammation and display augmented ROS production in mammals (Balestra et al. 2021; Bosco et al. 2018a, 2021; Morabito et al, 2011), leading to cell damage via oxidative modifications in proteins, lipids, and nucleic acids. Recently, we assessed ROS production in saliva samples by EPR spectroscopy to measure a 30-day saturation dive (Mrakic-Sposta et al. 2020). EPR is the only currently available technique capable of directly detecting oxygen-free radicals by specific spin probes (Dikalov et al. 2018). There are no studies investigating IGN-induced ROS during a dry dive test in the hyperbaric chamber using this very specific and quantitative methodology. This approach may help address a vexing question such as if the body of breath-hold or scuba divers actually emits more ROS (Mrakic-Sposta et al. 2019, 2020), what role it may have in IGN unfolding. Indeed, excessive ROS emission can impair synaptic plasticity and memory function (reviewed in Massad et al. 2011); on the other hand, ROS such as superoxide anion can directly quench NO., reducing its bioavailability, and thus the biological effects (Paolocci et al. 2001). Here, we show that a dry dive test boosts ROS emission and depletes total antioxidant capacity in otherwise healthy breath-hold divers, likely preparing the ground not only for a pro-oxidizing environment, but also for a pro-inflammatory terrain, as indicated by the rise in iNOS and homocysteine levels.
Of note, in our study the athletes breathed compressed air during descent and oxygen from 12 msw during decompression. When considering the narcosis mechanisms, it should be remarked that, in general, they are very similar to those of anesthetic gases, i.e., oxygen can dissolve in the fatty substances in the neuronal membranes and, because of its physical effect on altering ionic conductance through the membranes, it may reduce neuronal excitability. Surprisingly, however, a few studies made a vis-à-vis comparison between breathing air and enriched air nitrox (EAN) on IGN, and with controversial outcomes. Some highlighted worse psychomotor performance when using O2, EANx, or TRIMIX (Lafere et al. 2016, 2019; Balestra et al. 2018; Rocco et al. 2019). Conversely, others concluded that narcotic impairment was the same, although divers may perceive otherwise using TRIMIX (Piispanen et al. 2021).
It is worth stressing that we chose to let them breathe oxygen during decompression to obtain a nitrogen washout in our volunteers engaged in the diving training program the day after the experiment. Thus, throughout the test, the divers may have breathed a relevant hyperoxic gas mixture, almost 1.2 bar O2 at depth, and up to 2.2 bar pO2 for a longer time during decompression. Thus, in addition to IGN, hyperoxia may have also contributed to the symptomatology of the divers. Since high pO2 can cause a number of well-known effects, including sympatholytic effects (e.g., hyperoxic bradycardia) and oxidative stress, some of the effects seen at depth may relate not only to IGN, i.e., high pN2, but also to high pO2. Moreover, hyperoxia could have an impact on all the measured parameters, in particular on ROS and TAC levels. However, the contribution of hyperoxia to IGN—both at depth and surface remains to be understood better, especially with respect to the decline in cognitive tests. This is fertile terrain for future investigation.
Narcosis: antioxidant and immune activation during inflammation
To further investigate possible antioxidant or pro-oxidant pathways that may be altered during the dry test in healthy breath-hold drivers, accounting for unremitted ROS emission, we first assessed the levels of glutathione (GSH), a primary antioxidant. Its role in HBO therapy remains, indeed, controversial. On the one hand, GSH appears to be up-regulated after HBO during liver regeneration in rats (Ozden et al. 2004). On the other, when investigating possible HBO-imparted protection in mice with myocardial infarction (MI), Oliveira and colleagues concluded that augmented levels of reduced GSH accentuate the pro-oxidizing conditions found in the post-MI rat heart (Oliverira et al. 2020). Of note, no data are available on GSH bioavailability at depth in humans. These alterations, in addition to the likelihood of reduced NO. bioavailability, could pave the way, among other effects, to an altered arterial reactivity. In aggregate, these data corroborate our contention that a dry test in a hyperbaric chamber may lead to a pro-oxidizing environment, as attested by homocysteine and GSH level rise, and likely to pro-inflammatory conditions, as hinted at by the rise in iNOS levels. In tandem, these pro-oxidizing/pro-inflammatory conditions could acutely impair vascular reactivity. Indeed, among other effects, elevated homocysteine levels could alter arterial reactivity to adrenergic stimulation, modifying vascular sensitivity to norepinephrine, thus prompting vasorelaxation (Cipolla et al. 2000). A complex range of mechanisms conjures up in regulating the cerebral blood flow during dives. When altered, some of them could have a detrimental impact on brain functioning and can endure even after the dive (Caldwell et al. 2020; McKnight et al. 2021). Accordingly, it is well consolidated that even a single air dive can cause transient endothelial dysfunction (Culic et al. 2014), and breath-hold diving can induce significant alterations in blood gases and partial pressures in relatively short periods and shallow depths (Bosco et al. 2018b-c; 2020). Among other possible causes, all of this is not foreign to altered circulating BDNF levels. Indeed, as recalled above, in patients with psychiatric disorders, markedly reduced BDNF levels correlate with low superoxide dismutase and glutathione peroxidase, with a substantial rise in malondialdehyde (MDA) and end product of lipid peroxidation (Zhang et al. 2015). On the one hand, the activation of the dopamine D1-like receptor induces the expression of BDNF in cortical, striatal, and hippocampal rat tissue slices (Williams et al. 2009). On the other, dopamine oxidative catabolism by monoamine oxidases (MAO) B leads to an ROS outburst (Kaludercic et al. 2014a, b). Against this background, we sought to determine whether a correlation exists between the extent of ROS production and dopamine levels after a dry dive test. Hence, our data suggest that low dopamine levels could account for lower circulating BDNF levels, and thus cognitive deficit, while hinting at the intriguing possibility that its accelerated catabolism by MAO may contribute to the overall rise in ROS emission seen in deep divers.
Neopterin is a clinical marker of immune activation during inflammation, and it has been widely studied, particularly under stressful conditions (Gieseg et al. 2018). Moreover, high levels of this potent antioxidant could be generated by interferon-γ-activated macrophages and derive from the oxidation of 7,8-dihydroneopterin. Of note, neopterin levels are elevated in brain illnesses, such as depression (Celik et al. 2010; Maes et al. 2012). Intriguingly, when subjected to repetitive transcranial magnetic stimulation (rTMS), patients suffering from depression manifest symptom improvement, along with an inverse correlation between BDNF and neopterin. In fact, after rTMS, BDNF levels are more elevated and neopterin is lower than in sham-treated patients (Leblhuber et al. 2019). This evidence further supports the notion that a cross talk exists between BDNF and neopterin bioavailability that is central to IGN pathogenesis. At this time, we can only speculate that monitoring neopterin levels can serve as a footprint of narcosis duration/intensity.
Limitations and studies in perspective
The present study comes with some limitations that need further, in-depth investigation. First, for safety reasons, we enrolled a relatively small sample size of subjects in the hyperbaric chamber (protocol). Future studies would be conducted in larger populations at greater depths and in open water. Second, we acknowledge the observational nature of our experimental approach that, at the moment, precludes answering some salient mechanistic questions, such as factors leading to the decline of the systemic levels of dopamine, glutamate, and BDNF. We anticipate this question can be satisfactorily addressed only using animal models where sources of ROS can also be dissected in great detail. In the same vein, studying IGN onset and unfolding in small rodents would help determine if and in which brain regions pools of BDNF and key neurotransmitters, such as dopamine and glutamate, are more severely affected by single or repeated episodes of IGN, and same for the status of the BDNF-specific receptors, TrkB. All these relevant questions warrant future in-depth investigation and a more nuanced assessment of vascular reactivity.
Conclusion
Our study shows that healthy divers challenged with a dry dive test in a hyperbaric chamber develop narcosis and loss of cognitive function when at deep depth, i.e., 48 msw. A marked loss in circulating levels of dopamine/glutamate and BDNF at T4, i.e., 10 min after resurfacing, accompanies this phenomenon, along with altered systemic redox conditions, as revealed by the overall ROS emission detected both in the saliva and blood of these subjects, and a drop in total antioxidant capacity was shown. The present findings suggest that boosting dopamine/BDNF signaling pharmacological or behavioral interventions—pre-, during, or after diving—can attenuate narcosis and, therefore, its short- and long-term adverse effects, particularly in those subjects that undergo repeated deep diving.
Data availability
All raw data that were presented or mentioned in the manuscript are available from the corresponding authors on request.
Abbreviations
- ATA:
-
Absolute atmosphere
- BDNF:
-
Brain-derived neurotrophic factor
- Cys:
-
Cysteine
- CysGly:
-
Cysteinyl glycine
- CNS:
-
Central nervous systems
- DA:
-
Dopamine
- DDT:
-
Dry dive test
- EPR:
-
Electron paramagnetic resonance
- GSH:
-
Glutathione
- HBO2 :
-
Hyperbaric oxygen
- Hcy:
-
Homocysteine
- HPLC:
-
High-performance liquid chromatography
- IGN:
-
Inert gas narcosis
- iNOS:
-
Inducible nitric oxide synthase
- NE:
-
Norepinephrine
- NO:
-
Nitric oxide
- NO metabolites:
-
NO2, + NO3 = NOx
- OxS:
-
Oxidative stress
- ROS:
-
Reactive oxygen species
- TAC:
-
Total antioxidant capacity
- 8-iso-PGF2α:
-
8-Isoprostane
References
Agrimi J, Spalletti C, Baroni C et al (2019) Obese mice exposed to psychosocial stress display cardiac and hippocampal dysfunction associated with local brain-derived neurotrophic factor depletion. EBioMedicine 47:384–401. https://doi.org/10.1016/j.ebiom.2019.08.042
Bagayogo IP, Dreyfus CF (2009) Regulated release of BDNF by cortical oligodendrocytes is mediated through metabotropic glutamate receptors and the PLC pathway. ASN Neuro, 1. https://doi.org/10.1042/AN20090006
Balestra C, Machado ML, Theunissen S et al (2018) Critical flicker fusion frequency: a marker of cerebral arousal during modified gravitational conditions related to parabolic flights. Front Physiol 9:1403. https://doi.org/10.3389/fphys.2018.01403
Balestra C, Lambrechts K, Mrakic-Sposta S et al (2021) Hypoxic and hyperoxic breathing as a complement to low-intensity physical exercise programs: a proof-of-principle study. Int J Mol Sci 22(17):9600. https://doi.org/10.3390/ijms22179600
Benarroch EE (2015) Brain-derived neurotrophic factor: Regulation, effects, and potential clinical relevance. Neurology 84:1693–1704. https://doi.org/10.1212/WNL.0000000000001507
Bennett PB (1989) Physiological limitations to underwater exploration and work. Comp Biochem Physiol A Comp Physiol 93:295–300. https://doi.org/10.1016/0300-9629(89)90220-x
Bennett PB, Simon RS, Youngblood D (1975) Optimal use of nitrogen to suppress the high pressure nervous syndrome. Aviat Space Environ Med 46:37–40
Billaut F, Gueit P, Faure S, Costalat G, Lemaitre F (2018) Do elite breath-hold divers suffer from mild short-term memory impairments? Appl Physiol Nutr Metab 43:247–251. https://doi.org/10.1139/apnm-2017-0245
Binder DK, Scharfman HE (2004) Brain-derived neurotrophic factor. Growth Factors 22:123–131. https://doi.org/10.1080/08977190410001723308
Bosco G, Yang ZJ, Di Tano G et al (1985) (2010) Effect of in-water oxygen prebreathing at different depths on decompression-induced bubble formation and platelet activation. J Appl Physiol 108:1077–1083. https://doi.org/10.1152/japplphysiol.01058.2009
Bosco G, Rizzato A, Quartesan S et al (2018a) Spirometry and oxidative stress after rebreather diving in warm water. Undersea Hyperb Med 45:191–198
Bosco G, Rizzato A, Martani L et al (2018b) Arterial blood gas analysis in breath-hold divers at depth. Front Physiol 9:1558. https://doi.org/10.3389/fphys.2018.01558
Bosco G, Rizzato A, Moon RE, Camporesi EM (2018c) Environmental physiology and diving medicine. Front Psychol 9:72. https://doi.org/10.3389/fpsyg.2018.00072
Bosco G, Paganini M, Rizzato A et al (2020) Arterial blood gases in divers at surface after prolonged breath-hold. Eur J Appl Physiol 120:505–512. https://doi.org/10.1007/s00421-019-04296-2
Bosco G, Paganini M, Giacon TA et al (2021) Oxidative stress and inflammation, MicroRNA, and hemoglobin variations after administration of oxygen at different pressures and concentrations: a randomized trial. Int J Environ Res Public Health 18(18):9755. https://doi.org/10.3390/ijerph18189755
Brubakk AO, Ross JA, Thom SR (2014) Saturation diving; physiology and pathophysiology. Compr Physiol 4:1229–1272. https://doi.org/10.1002/cphy.c130048
Caldwell HG, Hoiland RL, Barak OF et al (2020) Alterations in resting cerebrovascular regulation do not affect reactivity to hypoxia, hyperoxia or neurovascular coupling following a SCUBA dive. Exp Physiol 105:1540–1549. https://doi.org/10.1113/EP088746
Cameron JW (2006) The molecular mechanisms of general anaesthesia: dissecting the GABAA receptor. Continuing Education in Anaesthesia, Critical Care & Pain 6:49–53
Celik C, Erdem M, Cayci T et al (2010) The association between serum levels of neopterin and number of depressive episodes of major depression. Prog Neuropsychopharmacol Biol Psychiatry 34:372–375. https://doi.org/10.1016/j.pnpbp.2010.01.002
Cipolla MJ, Williamson WK, Nehler ML, Taylor LM Jr, Porter JM (2000) The effect of elevated homocysteine levels on adrenergic vasoconstriction of human resistance arteries: the role of the endothelium and reactive oxygen species. J Vasc Surg 31:751–759. https://doi.org/10.1067/mva.2000.103797
Clark JE (2015) Moving in extreme environments: inert gas narcosis and underwater activities. Extrem Physiol Med 4:1. https://doi.org/10.1186/s13728-014-0020-7
Coco M, Buscemi A, Perciavalle V et al (2019) Cognitive deficits and white matter alterations in highly trained scuba divers. Front Psychol 10:2376. https://doi.org/10.3389/fpsyg.2019.02376
Culic VC, Van Craenenbroeck E, Muzinic NR et al (2014) Effects of scuba diving on vascular repair mechanisms. Undersea Hyperb Med 41:97–104
Dellanoce C, Cozzi L, Zuddas S, Pratali L, Accinni R (2014) Determination of different forms of aminothiols in red blood cells without washing erythrocytes. Biomed Chromatogr 28:327–331. https://doi.org/10.1002/bmc.3056
Dikalov SI, Polienko YF, Kirilyuk I (2018) Electron paramagnetic resonance measurements of reactive oxygen species by cyclic hydroxylamine spin probes. Antioxid Redox Signal 28:1433–1443. https://doi.org/10.1089/ars.2017.7396
Elia A, Gennser M, Harlow PS, Lees MJ (2021) Physiology, pathophysiology and (mal)adaptations to chronic apnoeic training: a state-of-the-art review. Eur J Appl Physiol 121:1543–1566. https://doi.org/10.1007/s00421-021-04664-x
Faeh D, Chiolero A, Paccaud F (2006) Homocysteine as a risk factor for cardiovascular disease: should we (still) worry about? Swiss Med Wkly 136:745–756
Feng N, Huke S, Zhu G, Tocchetti CG et al (2015) Constitutive BDNF/TrkB signaling is required for normal cardiac contraction and relaxation. Proc Natl Acad Sci USA 112:1880–1885. https://doi.org/10.1073/pnas.1417949112
Fitz-Clarke JR (2018) Breath-Hold Diving Compr Physiol 8:585–630. https://doi.org/10.1002/cphy.c160008
Freiberger JJ, Derrick BJ, Natoli MJ et al (2016) (1985) Assessment of the interaction of hyperbaric N2, CO2, and O2 on psychomotor performance in divers. J Appl Physiol 121:953–964. https://doi.org/10.1152/japplphysiol.00534.2016
Gasier HG, Demchenko IT, Tatro LG, Piantadosi CA (2017) S-nitrosylation of GAD65 is implicated in decreased GAD activity and oxygen-induced seizures. Neurosci Lett 653:283–287. https://doi.org/10.1016/j.neulet.2017.05.067
Gelfand R, Lambertsen CJ, Strauss R, Clark JM, Puglia CD (1983) Human respiration at rest in rapid compression and at high pressures and gas densities. J Appl Physiol Respir Environ Exerc Physiol 54:290–303. https://doi.org/10.1152/jappl.1983.54.1.290
Giacon TA, Bosco G, Vezzoli A et al (2022) Oxidative stress and motion sickness in one crew during competitive offshore sailing. Sci Rep 12(1):1142. https://doi.org/10.1038/s41598-022-05219-6
Gieseg SP, Baxter-Parker G, Lindsay A (2018) Neopterin, Inflammation, and Oxidative Stress: What Could We Be Missing? Antioxidants (Basel) 7. https://doi.org/10.3390/antiox7070080
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 126:131–138. https://doi.org/10.1016/0003-2697(82)90118-x
Grover CA, Grover DH (2014) Albert Behnke: nitrogen narcosis. J Emerg Med 46:225–227. https://doi.org/10.1016/j.jemermed.2013.08.080
Guiard BP, David DJ, Deltheil T et al (2008) Brain-derived neurotrophic factor-deficient mice exhibit a hippocampal hyperserotonergic phenotype. Int J Neuropsychopharmacol 11:79–92. https://doi.org/10.1017/S1461145707007857
Gulyaeva NV (2017) Interplay between brain BDNF and glutamatergic systems: a brief state of the evidence and association with the pathogenesis of depression. Biochemistry (mosc) 82:301–307. https://doi.org/10.1134/S0006297917030087
Hegarthy M, Waller DA (2005). Individual Differences in Spatial Abilities. In: Priti Shah and Akira Miyake (ed) The Cambridge Handbook of Visuospatial Thinking , Cambridge University Press pp. 121 – 169. https://doi.org/10.1017/CBO9780511610448.005
Hobbs M, Kneller W (2011) Anxiety and psychomotor performance in divers on the surface and underwater at 40 m. Aviat Space Environ Med 82:20–5. https://doi.org/10.3357/asem.2869.2011
Kaludercic N, Mialet-Perez J, Paolocci N, Parini A, Di Lisa F (2014a) Monoamine oxidases as sources of oxidants in the heart. J Mol Cell Cardiol 73:34–42. https://doi.org/10.1016/j.yjmcc.2013.12.032
Kaludercic N, Carpi A, Nagayama T et al (2014b) Monoamine oxidase B prompts mitochondrial and cardiac dysfunction in pressure overloaded hearts. Antioxid Redox Signal 20:267–280. https://doi.org/10.1089/ars.2012.4616
Karakaya H, Aksu S, Egi SM, Aydin S, Uslu A (2021) Effects of hyperbaric nitrogen narcosis on cognitive performance in recreational air SCUBA Divers: an auditory event-related brain potentials study. Ann Work Expo Health 65:505–515. https://doi.org/10.1093/annweh/wxaa132
Kim J, Lee S, Kang S et al (2017) Brain-derived neurotropic factor and GABAergic transmission in neurodegeneration and neuroregeneration. Neural Regen Res 12:1733–1741. https://doi.org/10.4103/1673-5374.217353
Kirkland PJ, Mathew D, Modi P, Cooper JS (2021) Nitrogen narcosis in diving. Treasure Island (FL), StatPearls Publishing, StatPearls
Kowianski P, Lietzau G, Czuba E et al (2018) BDNF: a key factor with multipotent impact on brain signaling and synaptic plasticity. Cell Mol Neurobiol 38:579–593. https://doi.org/10.1007/s10571-017-0510-4
Kuppers E, Beyer C (2001) Dopamine regulates brain-derived neurotrophic factor (BDNF) expression in cultured embryonic mouse striatal cells. NeuroReport 12:1175–1179. https://doi.org/10.1097/00001756-200105080-00025
Lafere P, Balestra C, Hemelryck W, Guerrero F, Germonpre P (2016) Do environmental conditions contribute to narcosis onset and symptom severity? Int J Sports Med 37:1124–1128. https://doi.org/10.1055/s-0042-110573
Lafere P, Hemelryck W, Germonpre P, Matity L, Guerrero F & Balestra C. (2019). Early detection of diving-related cognitive impairment of different nitrogen-oxygen gas mixtures using critical flicker fusion frequency. Diving Hyperb Med 49, 119–126. https://doi.org/10.28920/dhm49.2.119-126
Leblhuber F, Steiner K, Fuchs D (2019) Treatment of patients with geriatric depression with repetitive transcranial magnetic stimulation. J Neural Transm (vienna) 126:1105–1110. https://doi.org/10.1007/s00702-019-02037-5
Lindholm P (2009) Lundgren CE (2009) The physiology and pathophysiology of human breath-hold diving. J Appl Physiol 106:284–292. https://doi.org/10.1152/japplphysiol.90991.2008
Maes M, Mihaylova I, Kubera M, Ringel K (2012) Activation of cell-mediated immunity in depression: association with inflammation, melancholia, clinical staging and the fatigue and somatic symptom cluster of depression. Prog Neuropsychopharmacol Biol Psychiatry 36:169–175. https://doi.org/10.1016/j.pnpbp.2011.09.006
Martin JL, Finsterwald C (2011) Cooperation between BDNF and glutamate in the regulation of synaptic transmission and neuronal development. Commun Integr Biol 4(1):14–6. https://doi.org/10.4161/cib.4.1.13761
Massaad CA, Klann E (2011) Reactive oxygen species in the regulation of synaptic plasticity and memory. Antioxid Redox Signal 14:2013–2054. https://doi.org/10.1089/ars.2010.3208
Mattson MP (2008) Glutamate and neurotrophic factors in neuronal plasticity and disease. Ann N Y Acad Sci 1144:97–112. https://doi.org/10.1196/annals.1418.005
McKnight JC, Mulder E, Ruesch A et al (2021) When the human brain goes diving: using near-infrared spectroscopy to measure cerebral and systemic cardiovascular responses to deep, breath-hold diving in elite freedivers. Philos Trans R Soc Lond B Biol Sci 376:20200349. https://doi.org/10.1098/rstb.2020.0349
McLeod M, Bennett PB, Cooper RL (1988) Rat brain catecholamine release at 1, 10, 20, and 100 ATA heliox, nitrox, and trimix. Undersea Biomed Res 15:211–221
Meyer H (1899) Zur theorie der alkoholnarkose, Naunyn-Schmiedebergs Arch. Pharmakol 42:109–118
Miranda M, Morici JF, Zanoni MB, Bekinschtein P (2019) Brain-derived neurotrophic factor: a key molecule for memory in the healthy and the pathological brain. Front Cell Neurosci 13:363. https://doi.org/10.3389/fncel.2019.00363
Miyake A, Friedman NP, Emerson MJ, Witzki AH, Howerter A, Wager TD (2000) The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: a latent variable analysis. Cogn Psychol 41:49–100. https://doi.org/10.1006/cogp.1999.0734
Miyake A, Rettinger DA, Friedman NP et al (2001) Visuospatial working memory, executive functioning and spatial abilities. How are they related? J Exp Psychol Gen 130:621–640. https://doi.org/10.1037//0096-3445.130.4.621
Moon RE, Cherry AD, Stolp BW, Camporesi EM (2009) Pulmonary gas exchange in diving. J Appl Physiol (1985) 106:668–677. https://doi.org/10.1152/japplphysiol.91104.2008
Morabito C, Bosco G, Pilla R et al (2011) Effect of pre-breathing oxygen at different depth on oxidative status and calcium concentration in lymphocytes of scuba divers. Acta Physiol (oxf) 202:69–78. https://doi.org/10.1111/j.1748-1716.2010.02247.x
Mrakic-Sposta S, Gussoni M, Montorsi M, Porcelli S, Vezzoli A (2014) A quantitative method to monitor reactive oxygen species production by electron paramagnetic resonance in physiological and pathological conditions. Oxid Med Cell Longev 2014:306179. https://doi.org/10.1155/2014/306179
Mrakic-Sposta S, Vezzoli A, Rizzato A et al (2019) Oxidative stress assessment in breath-hold diving. Eur J Appl Physiol 119:2449–2456. https://doi.org/10.1007/s00421-019-04224-4
Mrakic-Sposta S, Vezzoli A, D'Alessandro F et al (2020) Change in Oxidative Stress Biomarkers During 30 Days in Saturation Dive: A Pilot Study. Int J Environ Res Public Health 17. https://doi.org/10.3390/ijerph17197118
Mrakic-Sposta S, Montorsi M, Porcelli S et al (2022) A. Effects of Prolonged Exposure to Hypobaric Hypoxia on Oxidative Stress: Overwintering in Antarctic Concordia Station. Oxid Med Cell Longev. 2022 Apr 30;2022:4430032. https://doi.org/10.1155/2022/4430032
Niu X, Watts VL, Cingolani OH et al (2012) Cardioprotective effect of beta-3 adrenergic receptor agonism: role of neuronal nitric oxide synthase. J Am Coll Cardiol 59:1979–1987. https://doi.org/10.1016/j.jacc.2011.12.046
Oliveira MS, Tanaka LY, Antonio EL et al (2020) Hyperbaric oxygenation improves redox control and reduces mortality in the acute phase of myocardial infarction in a rat model. Mol Med Rep 21:1431–1438. https://doi.org/10.3892/mmr.2020.10968
Overton CE, Lipnick RL (1991) Studies of Narcosis. Chapman and Hall, London
Ozden TA, Uzun H, Bohloli M et al (2004) The effects of hyperbaric oxygen treatment on oxidant and antioxidants levels during liver regeneration in rats. Tohoku J Exp Med 203:253–265. https://doi.org/10.1620/tjem.203.253
Paolocci N, Biondi R, Bettini M et al (2001) Oxygen radical-mediated reduction in basal and agonist-evoked NO release in isolated rat heart. J Mol Cell Cardiol 33:671–679. https://doi.org/10.1006/jmcc.2000.1334
Patrician A, Gasho C, Spajic B et al (1985) (2021) Case studies in physiology: breath-hold diving beyond 100 meters-cardiopulmonary responses in world-champion divers. J Appl Physiol 130:1345–1350. https://doi.org/10.1152/japplphysiol.00877.2020
Patrician A, Dujic Z, Spajic B, Drvis I, Ainslie PN (2021) Breath-hold diving—the physiology of diving deep and returning. Front Physiol 12:639377. https://doi.org/10.3389/fphys.2021.639377
Petroff OA (2002) GABA and glutamate in the human brain. Neuroscientist 8:562–573. https://doi.org/10.1177/1073858402238515
Piispanen WW, Lundell RV, Tuominen LJ, Räisänen-Sokolowski AK (2021) Assessment of Alertness and Cognitive Performance of Closed Circuit Rebreather Divers With the Critical Flicker Fusion Frequency Test in Arctic Diving Conditions. Front Physiol 12: 722915. https://doi.org/10.3389/fphys.2021.722915
Predovan D, Berryman N, Lussier M et al (2021) Assessment of the Relationship Between Executive Function and Cardiorespiratory Fitness in Healthy Older Adults. Front Psychol 12:742184. https://doi.org/10.3389/fpsyg.2021.742184
Querido AL (2017) Diving and antidepressants. Diving Hyperb Med 47:253–6. https://doi.org/10.28920/dhm47.4.253-256
Ranapurwala SI, Bird N, Vaithiyanathan P, Denoble PJ (2014) Scuba diving injuries among divers alert network members 2010–2011. Diving Hyperb Med 44:79–85
Rocco M, Pelaia P, Di Benedetto P et al (2019) Inert gas narcosis in scuba diving, different gases different reactions. Eur J Appl Physiol 119:247–255. https://doi.org/10.1007/s00421-018-4020-y
Rostain JC, Lavoute C (2016) Neurochemistry of pressure-induced nitrogen and metabolically inert gas narcosis in the central nervous system. Compr Physiol 6:1579–1590. https://doi.org/10.1002/cphy.c150024
Rostain JC, Lavoute C, Risso JJ, Vallee N, Weiss M (2011) A review of recent neurochemical data on inert gas narcosis. Undersea Hyperb Med 38:49–59
Rothman SM, Mattson MP (2013) Activity-dependent, stress-responsive BDNF signaling and the quest for optimal brain health and resilience throughout the lifespan. Neuroscience 239:228–240. https://doi.org/10.1007/s10571-017-0510-4
Tetzlaff K, Lemaitre F, Burgstahler C, Luetkens JA, Eichhorn L (2021) Going to extremes of lung physiology-deep breath-hold diving. Front Physiol 12:710429. https://doi.org/10.3389/fphys.2021.710429
Turle N, Saget A, Zouani B, Risso JJ (1998) Neurochemical studies of narcosis: a comparison between the effects of nitrous oxide and hyperbaric nitrogen on the dopaminergic nigro-striatal pathway. Neurochem Res 23:997–1003. https://doi.org/10.1023/a:1021040607207
Unsworth IP (1966) Inert gas narcosis—an introduction. Postgrad Med J 42:378–385
Vallee N, Rostain JC (1985) Risso JJ (2009) How can an inert gas counterbalance a NMDA-induced glutamate release? J Appl Physiol 107:1951–1958. https://doi.org/10.1152/japplphysiol.00097.2009
Vann R, Lang M (2011) Recreational diving fatalities. Undersea Hyperb Med 38:257–260
Vann RD, Butler FK, Mitchell SJ, Moon RE (2011) Decompression illness. Lancet 377:153–164. https://doi.org/10.1016/S0140-6736(10)61085-9
Vezzoli A, Dellanoce C, Mrakic-Sposta S et al (2016) Oxidative stress assessment in response to ultraendurance exercise: thiols redox status and ROS production according to duration of a competitive race. Oxid Med Cell Longev 2016:6439037. https://doi.org/10.1155/2016/6439037
Williams SN, Undieh AS (2009) Dopamine D1-like receptor activation induces brain-derived neurotrophic factor protein expression. NeuroReport 20:606–610. https://doi.org/10.1097/WNR.0b013e32832a0a98
Yang ZJ, Camporesi C, Yang X et al (2002) Hyperbaric oxygenation mitigates focal cerebral injury and reduces striatal dopamine release in a rat model of transient middle cerebral artery occlusion. Eur J Appl Physiol 87:101–107. https://doi.org/10.1007/s00421-002-0601-9
Zhang S, Takeda Y, Hagioka S et al (2004) The close relationship between decreases in extracellular GABA concentrations and increases in the incidence of hyperbaric oxygen-induced electrical discharge. Acta Med Okayama 58(2):91–95. https://doi.org/10.18926/AMO/32101
Zhang XY, Chen DC, Tan YL et al (2015) The interplay between BDNF and oxidative stress in chronic schizophrenia. Psychoneuroendocrinology 51:201–208. https://doi.org/10.1016/j.psyneuen.2014.09.029
Acknowledgements
The authors would like to thank FIPSAS (Federazione Italiana Pesca Sportiva e Attività Subacquee, Rome Italy), Centro di Medicina Iperbarica ATIP, Padova, Italy, for supply of the hyperbaric chamber, Italy, and for the kind technical assistance of A. Fontana. The authors would like to thank also all the divers for participating in this study: A.Z.; L.B.; A.M.; M.G.; M.T.; G.G.
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement. This study was part of the "BIRD 2020" project, funded by the DSB-University of Padova and the E-Heart project founded by the Dan Europe Foundation. N.P. is funded by the National Institute of Health (R01 HL1369180).
Author information
Authors and Affiliations
Contributions
All experiments were performed at the University of Padova (Padova, Italy) and National Research Council (Milano, Italy). TAG contributed to the study design, data collection, and drafting of the manuscript; NP contributed to drafting and critical review of the manuscript; SMS contributed to the study design, data analysis, interpretation, and drafting of the manuscript; AV contributed to the data analysis, interpretation, and critical review of the manuscript; CD contributed to data analysis. MP, JA, DC, EMC, and GG contributed to the study design and critical review of the manuscript. N D'A contributed to the study design, data analysis, and critical review of the manuscript. GB contributed to the study design, data interpretation, and critical review of the manuscript. GB and SMS confirmed that the study objectives and procedures were honestly disclosed. All the authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no competing interests.
Additional information
Communicated by Guido Ferretti.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bosco, G., Giacon, T.A., Paolocci, N. et al. Dopamine/BDNF loss underscores narcosis cognitive impairment in divers: a proof of concept in a dry condition. Eur J Appl Physiol 123, 143–158 (2023). https://doi.org/10.1007/s00421-022-05055-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-022-05055-6