Abstract
Purpose
To compare performance data of adolescents collected with five different bicycle spiroergometry protocols and to assess the necessity for establishing standard values for each protocol.
Methods
One-hundred-twenty adolescents completed two bicycle spiroergometries within 14 days. One of the two tests was performed based on our institutional weight-adapted protocol (P0). The other test was performed based on one out of four exercise protocols widely used for children and adolescents (P1, 2, 3 or 4) with 30 persons each. The two tests were performed in a random order. Routine parameters of cardiopulmonary exercise tests (CPET) such as VO2peak, maximum power, O2 pulse, OUES, VE/VCO2 slope as well as ventilatory and lactate thresholds were investigated. Agreement between protocols was evaluated by Bland–Altman analysis, coefficients of variation (CV) and intra-class correlation coefficients (ICC).
Results
None of the CPET parameters were significantly different between P0 and P1, 2, 3 or 4. For most of the parameters, low biases between P0 and P1–P4 were found and 95% confidence intervalls were narrow. CV and ICC values largely corresponded to well-defined analytical goals (CV < 10% and ICC > 0.9). Only maximal power (Pmax) showed differences in size and drift of the bias depending on the length of the step duration of the protocols.
Conclusion
Comparability between examination protocols has been shown for CPET parameters independent on step duration. Protocol-dependent standard values do not appear to be necessary. Only Pmax is dependent on the step duration, but in most cases, this has no significant influence on the fitness assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiopulmonary exercise testing (CPET) is the gold standard for determining aerobic fitness in medicine. It provides information describing the function of respiratory, cardiocirculatory, neuromuscular, blood, and metabolic systems, as well as limits of exercise tolerance and thus is useful in the diagnosis, management, and prognosis of diseases and sports medicine issues (Cooper et al. 2014). Since the physiological responses to exercise change during growth and development, appropriate pediatric reference values seem essential for adequate interpretation of CPET.
Two recent reviews have described significant heterogeneity between examination protocols (e.g., step duration and increment) and suggested adjustment for body size or weight (Blais et al. 2015; Pianosi et al. 2017). The authors pointed out that the quality criterion of comparability is not met due to the large number of different applied protocols. Therefore, recommendations conclude that each protocol needs its own set of reference values (Paridon et al. 2006).
VO2peak in adolescents and adults seems to be a robust variable that is normally independent of the exercise protocol (Armstrong and McManus 2017; Sheehan et al. 1987; Welsman et al. 2005). Nevertheless, there is lacking information about the comparability of parameters in the submaximal range. These values become increasingly important in pediatric performance diagnostics since achievable maximum values depend on the motivation of the test subject.
Testing duration represents the variable with the largest consensus in the literature. A plethora of different studies has indicated an optimum duration for a maximal cardiopulmonary exercise test of 8–12 min for adolescents and adults (Buchfuhrer et al. 1983; Hebestreit 2004; Myers et al. 1989; Takken et al. 2017; Whipp et al. 1981; Yoon et al. 2007).
The objective of this study was therefore to examine performance data collected with different bicycle spiroergometry protocols and to assess the necessity for establishing standard values for each protocol. Furthermore, the test efficiency of each examination protocol was evaluated in terms of required duration of the spiroergometry.
Methods
One-hundred-twenty adolescents (14–18 years) of both genders (60 males, 60 females) completed two bicycle spiroergometries with measurement of lactate until subjective exhaustion. The median interval between the two examinations was 9 days and ranged between 2 and 14 days. One of the two tests was performed considering a weight-adapted 1-min protocol of Windhaber and Schober (P0) developed and applied in the testing entity of sports medicine at the Department of Paediatric and Adolescent Surgery, Medical University of Graz. The other test was performed applying one of the exercise protocols widely used for children and adolescents [Godfrey–Protocol (P1) cited in Hebestreit (Hebestreit et al. 2002)], stress protocols recommended by the sports association (P2 and P3) or the protocol of Rost and Hollmann (P4) cited in Hebestreit (Hebestreit et al. 2002). Details of the different protocols are summarized in Table 1.
The participants were divided into 4 groups of 30 subjects each (15 males, 15 females). Group 1 was investigated with protocols P0 and P1, group 2 with protocols P0 and P2, group 3 with protocols P0 and P3 and group 4 with protocols P0 and P4. The order in which the two tests were performed was randomly assigned.
Conditions of participation were no infectious disease at least 14 days before the respective examination date, no chronic illness, ban on sports the day before and on the examination day and a light meal 2–3 h before the test.
CPET was performed in the upright position with a cycle ergometer (Excalibur Sport®, Lode B.V., Groningen, The Netherlands). Minute ventilation (VE), O2 uptake (VO2) and CO2 production (VCO2) were measured with a calibrated respiratory gas analysis system (Oxycon Pro®, Carl Reiner GmbH, Vienna, Austria). Heartrate was measured by continuous twelve-lead electrocardiography (Cardinal Health™ electrocardiography, Dublin, Ireland). Lactate levels were obtained collecting 20 μl blood of the earlobe prior to the test and at the end of each step (Biosen C_line®, EKF Diagnostics for life, Cardiff, UK).
All tests were supervised by a physician of sports medicine and a biomedical scientist. The participants were verbally encouraged to continue the investigation until exhaustion, as the participants were unable to maintain the required cadence of more than 60 revolutions per minute (rpm). A respiratory exchange rate (RER) > 1.10 was used as criterion to determine that VO2peak represents a physiological peak workload (Armstrong and van Mechelen 2008; Mezzani et al. 2009, 2003). All subjects included in the study had a RER above 1.10.
Informed written consent was obtained from all athletes and their legal guardians. The investigation conforms to the Code of Ethics of the World Medical Association (Declaration of Helsinki). The study was approved by the institutional review board (EK 30–187 ex 17/18). Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Measured and calculated parameters
We have selected parameters that should be part of a routine CPET as per the latest recommendations (Paridon et al. 2006). Additionally, submaximal parameters and slopes were added as previously published (Dallaire et al. 2017).
Maximal values
Maximal Heart Rate (HRmax) was defined as the highest heart rate achieved during exercise and expressed in bpm. Maximal Power (Pmax) is presented as Watt per bodyweight (W/kg). In case of incomplete step duration, the maximal work rate was calculated by linear extrapolation based on time. Peak oxygen uptake (VO2peak) was defined as the average value over the last 30 s prior to termination of the test and is expressed in ml/kg/min. O2 pulse was measured as VO2/HR and expressed in ml/beat.
Ventilatory and lactate thresholds
Ventilatory threshold (VT) was estimated according to the V-slope method (Beaver et al. 1986). The individual anaerobic lactate threshold (IAT) was defined as the VO2 value at the intersection point of the tangent to the lactate curve at the point of lactate maximum with the abscissa (time axis), as previously described in the literature (Pessenhofer et al. 1990; Schwaberger et al. 1985). Two- and 4-mmol thresholds were calculated as described by Mader (Mader and Heck 1986). All thresholds were expressed as values of VO2 in ml/kg/min.
Slopes
From gas exchange measurements (VE, VO2, VCO2), slopes were calculated using standard linear regression as described in the literature (Cooper et al. 2014; Sun et al. 2012). VE versus VCO2 (dVE/dVCO2) was calculated as the slope obtained by linear regression analysis of VE (l/min) versus VCO2 (ml/min).
Oxygen uptake efficiency slope (OUES) was calculated by a linear least square regression of the VO2 (ml/min) versus the common logarithm of VE (l/min) under consideration of all available measurement points (Baba et al. 1996).
Duration of test time
The duration of test time is expressed in minutes. For each protocol, the percentage of performed tests in the target range of 8–12 min is given.
Statistics
Descriptive statistics are presented as absolute and relative frequencies for categorical data and as means and standard deviations (SD) or medians and ranges for continuous data. For performance data, agreement between different protocols was evaluated by Bland–Altman analysis, coefficients of variation (CV) and intra-class correlation coefficients (ICC) for every group separately. For the Bland–Altman analysis, 95% confidence intervals (CI) for the bias (difference in parameters between P0 and the corresponding protocol) as well as the upper and lower limits of agreement are presented. The CV was calculated as SD of the bias (P0 minus other protocols, respectively) divided by the mean of the protocols and is presented as a percentage, i.e., CV * 100. This calculation of the CV is commonly used in sport medicine e.g., in Tompuri et al. 2016. The ICC and its 95% CI were assessed by a two-way random model (ICC [2,1] concept). Differences in performance data between the protocols were analyzed by pairwise Wilcoxon rank-rum tests due to non-normally distributed differences. Test durations of the protocols were compared by a paired t-test. The statistical analysis was performed with SAS software (version 9.4; SAS Institute, Inc). Statistical significance was set to α = 5%.
Results
Anthropometric characteristics
The mean age of the 120 participants was 15.7 years (range: 14–18 years). The anthropometric characteristics are presented in Table 2. All values were within national references. There were no differences between the groups.
Maximal values, thresholds and slopes
The mean, standard deviation, median, and range of parameters measured with P0 and with the protocol selected for the corresponding group 1–4 are shown in Table 3 for comparison. There were no statistically significant differences of the measurement results between P0 and P1, 2, 3 or 4. Details on biases, 95% CIs, bounds, CV- and ICC-values are presented in Table 4.
Differences in maximal values
The biases of HRmax between P0 and P1–P4 were approximately 1 beat/min with a 95% CI of − 3 to 3 beats/min. CV values were between 2 and 3% and ICC values were between 0.81 and 0.89.
The biases of VO2 peak were < 1 ml/kg/min, with a 95% CI from − 1.8 to 1.4 ml/kg/min. CV values were approximately 6% and ICC values were between 0.83 and 0.95.
The biases of O2 pulse were < 0.5 ml/beat, with a 95% CI from − 0.7 to 0.5 ml/beat. CV values were between 5 and 6% and ICC values ranged from 0.95 to 0.99.
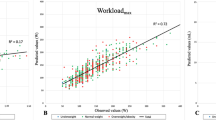
Although the differences in Pmax were also not statistically significant, there were differences in the size and drift of the bias depending on the length of the step duration of the protocols. In group 1, when comparing the protocols P0 and P1, both with a step duration of 1 min but different increments, the bias was 0.0 with a 95% CI of − 0.1 to 0.1 W/kg. In group 2, the average power measured with P0 was 0.4 W/kg higher (95% CI 0.3–0.5) than the power measured with P2 with step duration of 2 min, which corresponds to 9.4% of maximum power. In group 3, comparing P0 with P3 with a step duration of 3 min, the average power was 0.5 W/kg higher with P0 (95% CI 0.4–0.6), which corresponds to 11.5% of maximum power. In group 4, the average power measured with P0 was 0.3 W/kg higher (95% CI 0.2–0.4) than the power measured with P4 with step duration of 2 min, which corresponds to 7.7% of maximum power. CV values of all groups were similar at approximately 6%, with an ICC of 0.74–0.9.
Differences in thresholds
The smallest biases occurred with VT. Here, the biases of VO2 were approximately 0.2 ml/kg/min with a 95% CI of − 1 to 1 ml/kg/min. CV values were approximately 6% and ICC values were between 0.87 and 0.97. There was also no change in bias and CV depending on the length of the step duration.
At lactate thresholds, the biases of VO2 were between − 1.8 and 1.2 ml/kg/min with CV between 6 and 17%. Paradoxically, the highest CV values (13% at the 2-mmol threshold and 17% at the 4-mmol threshold) were found in group 1 comparing P0 to P1, despite both protocols apply the same step duration. The lowest CV values (6–9%) with ICC 0.95–0.97 at all thresholds were found in the comparison of P0 to P3, which have the biggest difference in the step duration.
Differences in Slopes
The biases of OUES were small at -3% to -1% in all groups. CV values of OUES were < 10% and the ICC values ranged between 0.91 and 0.96.
The biases of VE/VCO2 slope were from − 4% to 7%. CV values were < 10% in group 3 and 4, and > 10% in group 1 and 2.
Test duration and target range
The mean test duration was 11.0 (1.9) minutes for P0, 12.3 (2.6) minutes for P1, 16.0 (2.7) minutes for P2, 17.1 (3.5) minutes for P3 and 13.8 (1.7) minutes for P4. These differences were statistically significant (P0 vs. P1 p < 0.002; P0 vs. P2, P3 and P4 p < 0.001, respectively). The mean time saved was 4 min per examination for P0. While 70% of the examinations with P0 were in the target range of 8–12 min, this rate was 43% for P1, 13% for P2 and P4 and 3% for P3. Detailed information concerning the test duration is shown in Tables 5 and 6.
Discussion
The goal of this study was to compare performance data collected with different bicycle spiroergometry protocols in adolescents. Results of our study applying different protocols seem to be comparable. The differences of most parameters examined in this investigation were within the biological range of variation.
Comparability of maximal and submaximal values
For most of the parameters, we found low biases between P0 and P1-P4 and the 95% CIs were narrow.
The low biases for VO2peak with < 1 ml/kg/min (with a 95% CI of − 1.8 to 1.4 ml/kg/min) are consistent with other studies showing that the VO2peak is independent of exercise protocols in children (Armstrong and McManus 2017; Figueroa-Colon et al. 2000; Sheehan et al. 1987; Welsman et al. 2005), healthy adults (American Thoracic and American College of Chest 2003), heart failure patients (Bensimhon et al. 2008; Corra et al. 2006), and wheelchair users (Leicht et al. 2013).
Information about the comparability of values in submaximal ranges such as lactate or ventilatory thresholds and slopes is lacking in the literature.
Baba et al. have examined the differences between two treadmill protocols in children and adolescents aged 8–18 years (Baba et al. 1999b). With OUES bounds of − 18% to 17% their findings were in line with our data. In a further study, the authors stated that OUES is independent of duration, intensity of exercise tests and motivation (Baba et al. 1999a). Despite these similarities, the limits of agreement to VT were lower in our study (− 20 to 19%) compared to Baba and coworkers (− 31 to 31%).
Kullmer examined adult athletes with different protocols with step durations of 2 and 3 min on the bicycle ergometer. Similar to our data, VO2 at IAT were comparable in the protocols (Kullmer 1987).
These findings were also verified by Carta et al. investigating the differences between 1- and 3-min step protocols in adults. They also found no significant difference of VO2 observed at anaerobic threshold (Carta et al. 1991).
Variability of maximal and submaximal values
CV and ICC values in our study largely corresponded to well-defined analytical goals (CV < 10% and ICC > 0.9). Such criteria are commonly used in sport and exercise science (Atkinson and Nevill 1998).
Our results obtained with different protocols are consistent with the values for biological variability on reliability and reproducibility tests performed with repeated testing using the same protocols (American Thoracic and American College of Chest 2003; Armstrong and McManus 2017; Baba et al. 1999a; Johnston et al. 2005; Katch et al. 1982; Keteyian et al. 2010; Tompuri et al. 2016).
The repeatability of VO2peak and HRmax was examined by Jonsthon and colleagues in healthy children who performed two exercise tests with the same protocol 3 to 7 days apart (Johnston et al. 2005). Bias, bounds and CV values were in line with our investigation with different protocols.
In a statement on cardiopulmonary exercise testing by the American Thoracic Society (ATS) and American College of Chest Physicians (ACCP), the reproducibility of variables measured during CPET with repeated tests with the same protocol is given with CV values of 4–8% for HRmax, 4–9% of VO2peak, 4–14% for O2 pulse and 9–13% for VT (American Thoracic and American College of Chest 2003). The CV values in our investigation met these criteria for all these parameters.
CV values of Pmax were between 5.7 and 6.5% in all groups and therefore correspond to the CV value of approximately 6%, which is generally stated for ergometry (Haber 2001).
CV values of the OUES were below 10% corresponding to data published by others (Keteyian et al. 2010; Meyer et al. 1997). CV values of VE/VCO2 slope were between 8–14%, and therefore slightly higher than described in the literature with 5% in patients with heart failure (Keteyian et al. 2010).
Particularities of maximal power and lactate thresholds
As the only one of the investigated parameters, Pmax showed a dependence of size and drift of the bias on the length of the step duration. The drift can be explained by the fact that Pmax is not the physically measured value, but that the wattage in the last step is only fully valid when the step is completed according to its intended duration. If the stage duration is incomplete, the maximum wattage is calculated by linear extrapolation based on time (Haber 2001). This calculation mode therefore leads to a certain degree of inaccuracy in the evaluation of the achieved Pmax in examinations with different step length. In our opinion, the observed differences between tests with a step duration of 1 and 2 or 3 min do not seem to have a significant influence on the fitness assessment in most cases, as the range for normal values in adolescents is relatively wide [14]. Kullmer who examined the difference in Pmax between protocols with 2- and 3-min step durations, also concluded that the difference had no effect on the assessment of individual performance capacity (Kullmer 1987).
In our opinion, caution is warranted when Pmax values are close to the upper or lower limit of the standard value. In these cases, the step duration with which the standard values were created should be considered, otherwise the fitness level could be misjudged. Individual performance follow-up should also only be done with a protocol of the same step duration.
As for the CV values at the lactate thresholds, paradoxically, the best CV at all thresholds were found in group 3 comparing a 1-min (P0) to a 3-min (P3) step duration. The highest CVs were found at the 2- and 4-mmol threshold compared to P1, which is known to be the protocol with the same step duration as P0 (13% at the 2 mmol threshold and 17% at the 4 mmol threshold). These results showed that VO2 at lactate thresholds can be stable parameters, even when comparing protocols with different step durations. However, compliance with the preconditions before the test (at least 1 day of sports rest and light meal 2–3 h before the test to ensure full carbohydrate stores) is essential for good comparability (Kullmer 1987).
Target range and efficiency regarding test duration
We have evaluated the rate of examination reaching the target range of 8–12 min and the temporal efficiency of five examination protocols.
The time target was chosen based on recent recommendations (Buchfuhrer et al. 1983; Hebestreit 2004; Myers et al. 1989; Takken et al. 2017; Whipp et al. 1981; Yoon et al. 2007). The protocols P2, P3 and P4 were largely outside this target range. Although there were statistically significant differences in the duration of examination between these protocols and P0, this had no effect on the comparability of the parameters investigated. This is consistent with current evidence suggesting that CPET should take between 7 and 26 min to establish valid VO2peak values (Bishop et al. 1998; Midgley et al. 2008). Studies on the comparability of other CPET parameters with different durations of examination were not found.
Concerning time efficiency, P0 is clearly the favorite with an average time saving of 4 min. The resulting benefit corresponds to approximately 25% less time needed for the examination.
Conclusion
Comparability between examination protocols with step duration of 1 to 3 min is given for CPET parameters independent of step duration and increments. Protocol-dependent standard values do not appear to be necessary. However, it is recommended that the same protocol should be used for follow-up examinations of the same subject. Only Pmax depends on the step duration, but in most cases, this has no substantial influence on the fitness assessment. When Pmax values are close to the upper or lower limit of the standard value, the step duration with which the standard values were created should be considered, otherwise the fitness level could be misjudged. The extent to which these statements also apply to the comparison with ramp protocols and protocols with a step duration longer than 3 min are subject for further investigations. Concerning time efficiency, P0 is beneficial compared to other protocols.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Change history
24 May 2021
OA funding note is missing. Funding note should be Open access funding provided by Medical University of Graz.
Abbreviations
- CPET:
-
Cardiopulmonary exercise testing
- CV:
-
Coefficient of variation
- IAT:
-
Individual anaerobic threshold
- ICC:
-
Intra class correlation
- HRmax:
-
Maximal heart rate
- OUES:
-
Oxygen uptake efficiency slope
- P 0–4:
-
Protocol 0–4
- Pmax:
-
Maximal power
- RER:
-
Respiratory exchange ratio
- Rpm:
-
Revolutions per minute
- VCO2 :
-
CO2 production
- VE:
-
Minute ventilation
- VO2 :
-
Oxygen uptake
- VO2peak:
-
Peak oxygen uptake
- VT:
-
Ventilatory threshold
- W/kg:
-
Watt per kilogram body weight
References
American Thoracic S, American College of Chest P (2003) ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167:211–277. https://doi.org/10.1164/rccm.167.2.211
Armstrong N, McManus AM (2017) Aerobic fitness. In: Armstrong N, van Mechelen W (eds) Oxford textbook of children’s sport and exercise medicine, vol 1. Oxford University Press, Oxford, pp 161–178
Armstrong N, van Mechelen W (2008) Aerobic fitness. In: Armstrong N, van Mechelen W (eds) Paediatric exercise science and medicine, vol 1, 2nd edn. Oxford University Press, Oxford, pp 97–105. https://doi.org/10.1093/med/9780199232482.001.0001
Atkinson G, Nevill AM (1998) Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med 26:217–238. https://doi.org/10.2165/00007256-199826040-00002
Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, Tauchi N, Nishibata K (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28:1567–1572. https://doi.org/10.1016/s0735-1097(96)00412-3
Baba R, Kubo N, Morotome Y, Iwagaki S (1999a) Reproducibility of the oxygen uptake efficiency slope in normal healthy subjects. J Sports Med Phys Fitness 39:202–206
Baba R, Nagashima M, Nagano Y, Ikoma M, Nishibata K (1999b) Role of the oxygen uptake efficiency slope in evaluating exercise tolerance. Arch Dis Child 81:73–75. https://doi.org/10.1136/adc.81.1.73
Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol (1985) 60:2020–2027. https://doi.org/10.1152/jappl.1986.60.6.2020
Bensimhon DR et al (2008) Reproducibility of peak oxygen uptake and other cardiopulmonary exercise testing parameters in patients with heart failure (from the Heart Failure and A Controlled Trial Investigating Outcomes of exercise traiNing). Am J Cardiol 102:712–717. https://doi.org/10.1016/j.amjcard.2008.04.047
Bishop D, Jenkins DG, Mackinnon LT (1998) The effect of stage duration on the calculation of peak VO2 during cycle ergometry. J Sci Med Sport 1:171–178. https://doi.org/10.1016/s1440-2440(98)80012-1
Blais S, Berbari J, Counil FP, Dallaire F (2015) A systematic review of reference values in pediatric cardiopulmonary exercise testing. Pediatr Cardiol 36:1553–1564. https://doi.org/10.1007/s00246-015-1205-6
Buchfuhrer MJ, Hansen JE, Robinson TE, Sue DY, Wasserman K, Whipp BJ (1983) Optimizing the exercise protocol for cardiopulmonary assessment. J Appl Physiol Respir Environ Exerc Physiol 55:1558–1564. https://doi.org/10.1152/jappl.1983.55.5.1558
Carta P, Aru G, Barbieri MT, Mele M (1991) Bicycle ergometry exercise tests: a comparison between 3 protocols with an increasing load. Med Lav 82:56–64
Cooper DM, Leu SY, Galassetti P, Radom-Aizik S (2014) Dynamic interactions of gas exchange, body mass, and progressive exercise in children. Med Sci Sports Exerc 46:877–886. https://doi.org/10.1249/MSS.0000000000000180
Corra U, Mezzani A, Bosimini E, Giannuzzi P (2006) Prognostic value of time-related changes of cardiopulmonary exercise testing indices in stable chronic heart failure: a pragmatic and operative scheme. Eur J Cardiovasc Prev Rehabil 13:186–192. https://doi.org/10.1097/01.hjr.0000189807.22224.54
Dallaire F, Wald RM, Marelli A (2017) The role of cardiopulmonary exercise testing for decision making in patients with repaired tetralogy of fallot. Pediatr Cardiol 38:1097–1105. https://doi.org/10.1007/s00246-017-1656-z
Figueroa-Colon R, Hunter GR, Mayo MS, Aldridge RA, Goran MI, Weinsier RL (2000) Reliability of treadmill measures and criteria to determine VO2max in prepubertal girls. Med Sci Sports Exerc 32:865–869. https://doi.org/10.1097/00005768-200004000-00021
Haber P (2001) Die Ergometrie. In: Haber P (ed) Leitfaden zur medizinischen Trainingsberatung. Springer, Vienna, pp 248–264
Hebestreit H (2004) Exercise testing in children—what works, what doesn’t, and where to go? Paediatr Respir Rev 5(Suppl A):S11-14. https://doi.org/10.1016/s1526-0542(04)90002-4
Hebestreit H, Ferrari R, Lawrenz WJMH, Jüngst B-K (2002) Ergometrie im Kindes- und Jugendalter. In: Lawrenz W, Hebestreit H (eds) Kinder- und Jugendsportmedizin, vol 1. Georg Thieme Verlag, Stuttgart, pp 72–85
Johnston KN, Jenkins SC, Stick SM (2005) Repeatability of peak oxygen uptake in children who are healthy Pediatr. Phys Ther 17:11–17. https://doi.org/10.1097/01.pep.0000154340.43505.91
Katch VL, Sady SS, Freedson P (1982) Biological variability in maximum aerobic power. Med Sci Sports Exerc 14:21–25. https://doi.org/10.1249/00005768-198201000-00004
Keteyian SJ, Brawner CA, Ehrman JK, Ivanhoe R, Boehmer JP, Abraham WT (2010) Investigators P-HT Reproducibility of peak oxygen uptake and other cardiopulmonary exercise parameters: implications for clinical trials and clinical practice. Chest 138:950–955. https://doi.org/10.1378/chest.09-2624
Kullmer K, Mücke E (1987) Sportmedizin Kursbestimmung Vergleichende Untersuchung zum Einfluß der Belastungsdauer bei der Fahrradergometrie auf Leistungsfähigkeit Herz-Kreislaufgrößen und Hormone. Springer, Berlin. https://doi.org/10.1007/978-3-642-72571-5
Leicht CA, Tolfrey K, Lenton JP, Bishop NC, Goosey-Tolfrey VL (2013) The verification phase and reliability of physiological parameters in peak testing of elite wheelchair athletes. Eur J Appl Physiol 113:337–345. https://doi.org/10.1007/s00421-012-2441-6
Mader A, Heck H (1986) A theory of the metabolic origin of “anaerobic threshold.” Int J Sports Med 7(Suppl 1):45–65
Meyer K, Westbrook S, Schwaibold M, Hajric R, Peters K, Roskamm H (1997) Short-term reproducibility of cardiopulmonary measurements during exercise testing in patients with severe chronic heart failure. Am Heart J 134:20–26. https://doi.org/10.1016/s0002-8703(97)70102-9
Mezzani A, Corra U, Bosimini E, Giordano A, Giannuzzi P (2003) Contribution of peak respiratory exchange ratio to peak VO2 prognostic reliability in patients with chronic heart failure and severely reduced exercise capacity. Am Heart J 145:1102–1107. https://doi.org/10.1016/S0002-8703(03)00100-5
Mezzani A et al (2009) Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 16:249–267. https://doi.org/10.1097/HJR.0b013e32832914c8
Midgley AW, Bentley DJ, Luttikholt H, McNaughton LR, Millet GP (2008) Challenging a dogma of exercise physiology: does an incremental exercise test for valid VO 2 max determination really need to last between 8 and 12 minutes? Sports Med 38:441–447. https://doi.org/10.2165/00007256-200838060-00001
Myers J, Walsh D, Buchanan N, Froelicher VF (1989) Can maximal cardiopulmonary capacity be recognized by a plateau in oxygen uptake? Chest 96:1312–1316. https://doi.org/10.1378/chest.96.6.1312
Paridon SM et al (2006) Clinical stress testing in the pediatric age group: a statement from the American Heart Association Council on Cardiovascular Disease in the Young. Committee Atheroscler Hypertens Obes Youth Circ 113:1905–1920. https://doi.org/10.1161/CIRCULATIONAHA.106.174375
Pessenhofer H, Sauseng N, Schwaberger G (1990) Use of simple mathematical models in sports medicine performance diagnosis. Biomed Tech (Berl) 35(Suppl 2):195–196. https://doi.org/10.1515/bmte.1990.35.s2.195
Pianosi PT, Liem RI, McMurray RG, Cerny FJ, Falk B, Kemper HC (2017) Pediatric exercise testing: value and implications of peak oxygen uptake. Children (Basel). https://doi.org/10.3390/children4010006
Schwaberger G, Pessenhofer H, Schmid P (1985) Relevance of lactate determination in sports medicine. Wien Med Wochenschr 135:234–235, 238–241
Sheehan JM, Rowland TW, Burke EJ (1987) A comparison of four treadmill protocols for determination of maximum oxygen uptake in 10- to 12-year-old boys. Int J Sports Med 8:31–34. https://doi.org/10.1055/s-2008-1025636
Sun XG, Hansen JE, Stringer WW (2012) Oxygen uptake efficiency plateau: physiology and reference values. Eur J Appl Physiol 112:919–928. https://doi.org/10.1007/s00421-011-2030-0
Takken T, Bongers BC, van Brussel M, Haapala EA, Hulzebos EHJ (2017) cardiopulmonary exercise testing in pediatrics. Ann Am Thorac Soc 14:S123–S128. https://doi.org/10.1513/AnnalsATS.201611-912FR
Tompuri TT, Lintu N, Soininen S, Laitinen T, Lakka TA (2016) Comparison between parameters from maximal cycle ergometer test first without respiratory gas analysis and thereafter with respiratory gas analysis among healthy prepubertal children. Appl Physiol Nutr Metab 41:624–630. https://doi.org/10.1139/apnm-2015-0355
Welsman J, Bywater K, Farr C, Welford D, Armstrong N (2005) Reliability of peak VO(2) and maximal cardiac output assessed using thoracic bioimpedance in children. Eur J Appl Physiol 94:228–234. https://doi.org/10.1007/s00421-004-1300-5
Whipp BJ, Davis JA, Torres F, Wasserman K (1981) A test to determine parameters of aerobic function during exercise. J Appl Physiol Respir Environ Exerc Physiol 50:217–221. https://doi.org/10.1152/jappl.1981.50.1.217
Yoon BK, Kravitz L, Robergs R (2007) VO2max, protocol duration, and the VO2 plateau. Med Sci Sports Exerc 39:1186–1192. https://doi.org/10.1249/mss.0b13e318054e304
Acknowledgements
None declared.
Funding
Open access funding provided by Medical University of Graz.
Author information
Authors and Affiliations
Contributions
JW conceptualized and designed the study, performed the measurements, and wrote the manuscript. MS, KK and AW performed the measurements and critically reviewed the manuscript. MH and RR performed the statistics and critically reviewed the manuscript. GS and CC wrote the manuscript. PS critically reviewed the manuscript. HT enabled the investigations and critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Consent to participate
Informed written consent was obtained from all athletes and their legal guardians.
Consent to publication
Not applicable. All data were published anonymously.
Ethical approval information
The study has been approved by the local ethics committee (EK 30-187 ex 17/18).
Additional information
Communicated by Philip D Chilibeck.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Windhaber, J., Steinbauer, M., Holter, M. et al. Bicycle spiroergometry: comparison of standardized examination protocols for adolescents: is it necessary to define own standard values for each protocol?. Eur J Appl Physiol 121, 1783–1794 (2021). https://doi.org/10.1007/s00421-021-04601-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-021-04601-y