Abstract
Purpose
This study aims to assess the accuracy of three parameters (white-to-white distance [WTW], angle-to-angle [ATA], and sulcus-to-sulcus [STS]) in predicting postoperative vault and to formulate an optimized predictive model.
Methods
In this retrospective study, a cohort of 465 patients (comprising 769 eyes) who underwent the implantation of the V4c implantable Collamer lens with a central port (ICL) for myopia correction was examined. Least absolute shrinkage and selection operator (LASSO) regression and classification models were used to predict postoperative vault. The influences of WTW, ATA, and STS on predicting the postoperative vault and ICL size were analyzed and compared.
Results
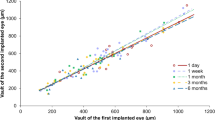
The dataset was randomly divided into training (80%) and test (20%) sets, with no significant differences observed between them. The screened variables included only seven variables which conferred the largest signal in the model, namely, lens thickness (LT, estimated coefficients for logistic least absolute shrinkage of −0.20), STS (−0.04), size (0.08), flat K (−0.006), anterior chamber depth (0.15), spherical error (−0.006), and cylindrical error (−0.0008). The optimal prediction model depended on STS (R2=0.419, RMSE=0.139), whereas the least effective prediction model relied on WTW (R2=0.395, RMSE=0.142). In the classified prediction models of the vault, classification prediction of the vault based on STS exhibited superior accuracy compared to ATA or WTW.
Conclusions
This study compared the capabilities of WTW, ATA, and STS in predicting postoperative vault, demonstrating that STS exhibits a stronger correlation than the other two parameters.



Similar content being viewed by others
References
Sanders DR, Doney K, Poco M, Group ICLiToMS (2004) United States Food and Drug Administration clinical trial of the implantable Collamer lens (ICL) for moderate to high myopia: three-year follow-up. Ophthalmology 111:1683–1692. https://doi.org/10.1016/j.ophtha.2004.03.026
Packer M (2016) Meta-analysis and review: effectiveness, safety, and central port design of the intraocular Collamer lens. Clin Ophthalmol 10:1059–1077. https://doi.org/10.2147/opth.S111620
Nakamura T, Isogai N, Kojima T, Yoshida Y, Sugiyama Y (2018) Implantable Collamer lens sizing method based on swept-source anterior segment optical coherence tomography. Am J Ophthalmol 187:99–107. https://doi.org/10.1016/j.ajo.2017.12.015
Choi KH, Chung SE, Chung TY, Chung ES (2007) Ultrasound biomicroscopy for determining visian implantable contact lens length in phakic IOL implantation. J Refract Surg 23:362–367. https://doi.org/10.3928/1081-597X-20070401-08
Dougherty PJ, Rivera RP, Schneider D et al (2011) Improving accuracy of phakic intraocular lens sizing using high-frequency ultrasound biomicroscopy. J Cataract Refract Surg 37:13–18. https://doi.org/10.1016/j.jcrs.2010.07.014
Kojima T, Yokoyama S, Ito M et al (2012) Optimization of an implantable Collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol 153:632–637, 637 e631. https://doi.org/10.1016/j.ajo.2011.06.031
Wu H, Zhong DJ, Luo DQ et al (2023) Improvement in the ideal range of vault after implantable Collamer lens implantation: a new vault prediction formula. Front Med (Lausanne) 10:1132102. https://doi.org/10.3389/fmed.2023.1132102
Reinstein DZ, Archer TJ, Vida RS, Piparia V, Potter JG (2022) New sizing parameters and model for predicting postoperative vault for the implantable Collamer lens posterior chamber phakic intraocular lens. J Refract Surg 38:272–279. https://doi.org/10.3928/1081597x-20220302-01
Liu CH, Liu S, Zhao YB et al (2022) Development and validation of a nomogram for esophagogastric variceal bleeding in liver cirrhosis: a cohort study in 1099 cases. J Dig Dis 23:597–609. https://doi.org/10.1111/1751-2980.13145
Tang G, Qi L, Sun Z et al (2021) Evaluation and analysis of incidence and risk factors of lower extremity venous thrombosis after urologic surgeries: a prospective two-center cohort study using LASSO-logistic regression. Int J Surg 89:105948. https://doi.org/10.1016/j.ijsu.2021.105948
Yokoyama T, Nakahara S, Kondo H, Miyake Y, Sakamoto T (2022) Novel score for predicting early emergency endovascular therapy in trauma care using logistic LASSO regression. Acute Med Surg 9:e774. https://doi.org/10.1002/ams2.774
Chen X, Ye Y, Yao H et al (2023) Predicting post-operative vault and optimal implantable Collamer lens size using machine learning based on various ophthalmic device combinations. Biomed Eng Online 22:59. https://doi.org/10.1186/s12938-023-01123-w
Reinstein DZ, Archer TJ, Silverman RH, Rondeau MJ, Coleman DJ (2009) Correlation of anterior chamber angle and ciliary sulcus diameters with white-to-white corneal diameter in high myopes using artemis VHF digital ultrasound. J Refract Surg 25:185–194. https://doi.org/10.3928/1081597X-20090201-03
Oh J, Shin HH, Kim JH, Kim HM, Song JS (2007) Direct measurement of the ciliary sulcus diameter by 35-megahertz ultrasound biomicroscopy. Ophthalmology 114:1685–1688. https://doi.org/10.1016/j.ophtha.2006.12.018
Chen Q, Tan W, Lei X et al (2020) Clinical prediction of excessive vault after implantable Collamer lens implantation using ciliary body morphology. J Refract Surg 36:380–387. https://doi.org/10.3928/1081597x-20200513-02
Pei X, Qi D, Liu J et al (2023) Screening marker genes of type 2 diabetes mellitus in mouse lacrimal gland by LASSO regression. Sci Rep 13:6862. https://doi.org/10.1038/s41598-023-34072-4
He N, Wu L, Qi M et al (2016) Comparison of ciliary body anatomy between American Caucasians and ethnic Chinese using ultrasound biomicroscopy. Curr Eye Res 41:485–491. https://doi.org/10.3109/02713683.2015.1024869
Tassignon MJ, Rozema JJ, Dhubhghaill SN (2013) 3D Scheimpflug measurement of posterior chamber plate haptic phakic intraocular lens/crystalline lens gap profile. Acta Ophthalmol 91:e649–e650. https://doi.org/10.1111/aos.12211
Acknowledgements
The authors would like to express their deepest gratitude to all the participants in this study; all the hospital staff, for the coordination and logistic arrangements of this study.
Funding
Supported in part by the State administration of traditional Chinese medicine Science and Technology Department-Zhejiang Provincial Administration of Traditional Chinese Medicine Co-construction Science and Technology Plan under Grant (No. GZY-ZJ-KJ-23086), the Science and Technology Program of Traditional Chinese Medicine in Zhejiang Province (No. 2024ZL617), and the Science and Technology Plan Project of Wenzhou Science and Technology Bureau (No. Y2023809).
Author information
Authors and Affiliations
Contributions
YF.Y. provided the concept and designed this study. J.Z. and FF.L. completed data collection. FF.L. did analysis and interpretation. J.Z. and SY.J. wrote the manuscript. SQ.W., Q.D., G.Y., FJ.B., D.C., XY.Z., and YF.Y. provided critical revision of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Eye Hospital of Wenzhou Medical University (H2023-032-K-30). Written informed consent was obtained from each participant.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 218 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, J., Li, FF., Jiang, SY. et al. Predictability comparison of sizing parameters for postoperative vault after implantable Collamer lens implantation. Graefes Arch Clin Exp Ophthalmol (2024). https://doi.org/10.1007/s00417-024-06408-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00417-024-06408-x