Abstract
Purpose
This review was designed to compare different corneal imaging modalities using artificial intelligence (AI) for the diagnosis of keratoconus (KCN), subclinical KCN (SKCN), and forme fruste KCN (FFKCN).
Methods
A comprehensive systematic search was conducted in scientific databases, including Web of Science, PubMed, Scopus, and Google Scholar based on the PRISMA statement. Two independent reviewers assessed all potential publications on AI and KCN up to March 2022. The Critical Appraisal Skills Program (CASP) 11-item checklist was used to evaluate the validity of the studies. Eligible articles were categorized into three groups (KCN, SKCN, and FFKCN) and included in the meta-analysis. The pooled estimate of accuracy (PEA) was calculated for all selected articles.
Results
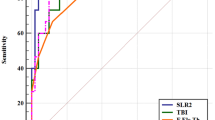
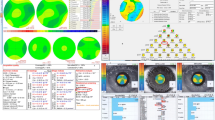
The initial search yielded 575 relevant publications, of which 36 met the CASP quality criteria and were included in the analysis. Qualitative assessment showed that Scheimpflug and Placido combined with biomechanical and wavefront evaluations improved KCN detection (PEA, 99.2, and 99.0, respectively). The Scheimpflug system (92.25 PEA, 95% CI, 94.76–97.51) and a combination of Scheimpflug and Placido (96.44 PEA, 95% CI, 93.13–98.19) had the highest diagnostic accuracy for the detection of SKCN and FFKCN, respectively. The meta-analysis outcomes showed no significant difference between the CASP score and accuracy of the publications (all P > 0.05).
Conclusions
Simultaneous Scheimpflug and Placido corneal imaging methods provide high diagnostic accuracy for early detection of keratoconus. The use of AI models improves the discrimination of keratoconic eyes from normal corneas.




Similar content being viewed by others
References
Vega-Estrada A, Mimouni M, Espla E, del Barrio JA, Alio JL (2019) Corneal epithelial thickness intrasubject repeatability and its relation with visual limitation in keratoconus. Am J Ophthalmol 200:255–262. https://doi.org/10.1016/j.ajo.2019.01.015
Siganos CS, Tsiklis NS, Miltsakakis DG, Georgiadis NS, Georgiadou IN, Kymionis GD, Pallikaris IG (2010) Changing indications for penetrating keratoplasty in Greece, 1982–2006: a multicenter study. Cornea 29:372–374. https://doi.org/10.1097/ICO.0b013e3181bd44a1
Hashemi H, Heydarian S, Yekta A, Ostadimoghaddam H, Aghamirsalim M, Derakhshan A, Khabazkhoob M (2018) High prevalence and familial aggregation of keratoconus in an Iranian rural population: a population-based study. Ophthalmic Physiol Opt 38:447–455. https://doi.org/10.1111/opo.12448
Özalp O, Atalay E, Yıldırım N (2021) Prevalence and risk factors for keratoconus in a university-based population in Turkey. J Cataract Refract Surg 47(12):1524–1529. https://doi.org/10.1097/j.jcrs.0000000000000669
Reeves SW, Ellwein LB, Kim T, Constantine R, Lee PP (2009) Keratoconus in the Medicare population. Cornea 28:40–42. https://doi.org/10.1097/ICO.0b013e3181839b06
Torres Netto EA, Al-Otaibi WM, Hafezi NL, Kling S, Al-Farhan HM, Randleman JB, Hafezi F (2018) Prevalence of keratoconus in paediatric patients in Riyadh, Saudi Arabia. Br J Ophthalmol 102:1436–1441. https://doi.org/10.1136/bjophthalmol-2017-311391
Armstrong BK, Smith SD, Romac Coc I, Agarwal P, Mustapha N, Navon S (2021) Screening for keratoconus in a high-risk adolescent population. Ophthalmic Epidemiol 28:191–197. https://doi.org/10.1080/09286586.2020.1804593
Assiri AA, Yousuf BI, Quantock AJ, Murphy PJ (2005) Incidence and severity of keratoconus in Asir province, Saudi Arabia. Br J Ophthalmol 89:1403–1406. https://doi.org/10.1136/bjo.2005.074955
Hwang S, Lim DH, Chung TY (2018) Prevalence and incidence of keratoconus in South Korea: a nationwide population-based study. Am J Ophthalmol 192:56–64. https://doi.org/10.1016/j.ajo.2018.04.027
Henriquez MA, Hadid M, Izquierdo L Jr (2020) A systematic review of subclinical keratoconus and forme fruste keratoconus. J Refract Surg 36:270–279. https://doi.org/10.3928/1081597x-20200212-03
Ambrósio R Jr, Machado AP, Leão E et al (2022) Optimized artificial intelligence for enhanced ectasia detection using Scheimpflug-based corneal tomography and biomechanical data. Am J Ophthalmol 251:126–142. https://doi.org/10.1016/j.ajo.2022.12.016
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Richardson WS, Wilson MC, Nishikawa J, Hayward RS (1995) The well-built clinical question: a key to evidence-based decisions. ACP J Club 123:A12-13
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P (2007) Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak 7:16. https://doi.org/10.1186/1472-6947-7-16
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Oxman AD, Cook DJ, Guyatt GH, Bass E, Brill-Edwards P, Browman G, Detsky A, Farkouh M, Gerstein H, Haines T (1994) Users’ guides to the medical literature: VI How to use an overview. Jama 272:1367–1371. https://doi.org/10.1001/jama.272.17.1367
Noyes J, Booth A, Flemming K, Garside R, Harden A, Lewin S, Pantoja T, Hannes K, Cargo M, Thomas J (2018) Cochrane Qualitative and Implementation Methods Group guidance series-paper 3: methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J Clin Epidemiol 97:49–58. https://doi.org/10.1016/j.jclinepi.2017.06.020
Alshammari G, Hamad AA, Abdullah ZM, Alshareef AM, Alhebaishi N, Alshammari A, Belay A (2021) Applications of deep learning on topographic images to improve the diagnosis for dynamic systems and unconstrained optimization. Wirel Commun Mob Comput 2021:1–7
Maeda N, Klyce SD, Smolek MK (1995) Neural network classification of corneal topography. Preliminary demonstration. Invest Ophthalmol Vis Sci 36:1327–1335
Kuo BI, Chang WY, Liao TS, Liu FY, Liu HY, Chu HS, Chen WL, Hu FR, Yen JY, Wang IJ (2020) Keratoconus screening based on deep learning approach of corneal topography. Transl Vis Sci Technol 9:53. https://doi.org/10.1167/tvst.9.2.53
Lavric A, Valentin P (2019) KeratoDetect: keratoconus detection algorithm using convolutional neural networks. Comput Intell Neurosci 8162567. https://doi.org/10.1155/2019/8162567
Mohammadpour M, Heidari Z (2021) Orbscan. In: Mohammadpour, M. (eds) Diagnostics in ocular imaging. Springer, Cham, pp 23–63. https://doi.org/10.1007/978-3-030-54863-6_2
Zéboulon P, Debellemanière G, Bouvet M, Gatinel D (2020) Corneal topography raw data classification using a convolutional neural network. Am J Ophthalmol 219:33–39. https://doi.org/10.1016/j.ajo.2020.06.005
Souza MB, Medeiros FW, Souza DB, Garcia R, Alves MR (2010) Evaluation of machine learning classifiers in keratoconus detection from orbscan II examinations. Clinics (Sao Paulo) 65:1223–1228. https://doi.org/10.1590/s1807-59322010001200002
Chan C, Ang M, Saad A, Chua D, Mejia M, Lim L, Gatinel D (2015) Validation of an objective scoring system for forme fruste keratoconus detection and post-LASIK ectasia risk assessment in Asian eyes. Cornea 34:996–1004. https://doi.org/10.1097/ico.0000000000000529
Hernández-Camarena JC, Chirinos-Saldaña P, Navas A, Ramirez-Miranda A, de la Mota A, Jimenez-Corona A, Graue-Hernández EO (2014) Repeatability, reproducibility, and agreement between three different Scheimpflug systems in measuring corneal and anterior segment biometry. J Refract Surg 30:616–621. https://doi.org/10.3928/1081597X-20140815-02
Heidari Z, Hashemi H, Mohammadpour M, Amanzadeh K, Fotouhi A (2021) Evaluation of corneal topographic, tomographic and biomechanical indices for detecting clinical and subclinical keratoconus: a comprehensive three-device study. Int J Ophthalmol 14:228–239. https://doi.org/10.18240/ijo.2021.02.08
Mohammadpour M, Heidari Z (2021) Pentacam. In: Mohammadpour, M. (eds) Diagnostics in ocular imaging. Springer, Cham, pp 65–162. https://doi.org/10.1007/978-3-030-54863-6_3
Malyugin B, Sakhnov S, Izmailova S, Boiko E, Pozdeyeva N, Axenova L, Axenov K, Titov A, Terentyeva A, Zakaraiia T, Myasnikova V (2021) Keratoconus diagnostic and treatment algorithms based on machine-learning methods. Diagnostics (Basel, Switzerland) 11:1993. https://doi.org/10.3390/diagnostics11101933
Abdelmotaal H, Abdou AA, Omar AF, El-Sebaity DM, Abdelazeem K (2021) Pix2pix conditional generative adversarial networks for Scheimpflug camera color-coded corneal tomography image generation. Transl Vis Sci Technol 10:21. https://doi.org/10.1167/tvst.10.7.21
Al-Timemy AH, Mosa ZM, Alyasseri Z, Lavric A, Lui MM, Hazarbassanov RM, Yousefi S (2021) A hybrid deep learning construct for detecting keratoconus from corneal maps. Transl Vis Sci Technol 10:16. https://doi.org/10.1167/tvst.10.14.16
Cao K, Verspoor K, Chan E, Daniell M, Sahebjada S, Baird PN (2021) Machine learning with a reduced dimensionality representation of comprehensive Pentacam tomography parameters to identify subclinical keratoconus. Comput Biol Med 138:104884. https://doi.org/10.1016/j.compbiomed.2021.104884
Cao K, Verspoor K, Sahebjada S, Baird PN (2020) Evaluating the performance of various machine learning algorithms to detect subclinical keratoconus. Transl Vis Sci Technol 9:24. https://doi.org/10.1167/tvst.9.2.24
Feng R, Xu Z, Zheng X, Hu H, Jin X, Chen DZ, Yao K, Wu J (2021) KerNet: a novel deep learning approach for keratoconus and sub-clinical keratoconus detection based on raw data of the Pentacam HR system. IEEE J Biomed Health Inform 25:3898–3910. https://doi.org/10.1109/jbhi.2021.3079430
Moshirfar M, Motlagh MN, Murri MS, Momeni-Moghaddam H, Ronquillo YC, Hoopes PC (2019) Galilei corneal tomography for screening of refractive surgery candidates: a review of the literature, Part II. Med Hypothesis Discov Innov Ophthalmol 8:204–218
Smadja D, Touboul D, Cohen A, Doveh E, Santhiago MR, Mello GR, Krueger RR, Colin J (2013) Detection of subclinical keratoconus using an automated decision tree classification. Am J Ophthalmol 156:237-246.e231. https://doi.org/10.1016/j.ajo.2013.03.034
Mohammadpour M, Heidari Z, Hashemi H, Yaseri M, Fotouhi A (2022) Comparison of artificial intelligence-based machine learning classifiers for early detection of keratoconus. Eur J Ophthalmol 32:1352–1360. https://doi.org/10.1177/11206721211073442
Heidari Z, Jafarzadehpour E, Mohammadpour M, Hashemi H (2022) Best indices of dual Scheimpflug/Placido tomographer for keratoconus detection. Int Ophthalmol. https://doi.org/10.1007/s10792-022-02533-w
Prakash G, Agarwal A, Jacob S, Kumar DA, Agarwal A, Banerjee R (2009) Comparison of fourier-domain and time-domain optical coherence tomography for assessment of corneal thickness and intersession repeatability. Am J Ophthalmol 148:282-290.e282. https://doi.org/10.1016/j.ajo.2009.03.012
Hwang ES, Schallhorn JM, Randleman JB (2020) Utility of regional epithelial thickness measurements in corneal evaluations. Surv ophthalmol 65:187–204. https://doi.org/10.1016/j.survophthal.2019.09.003
Kanellopoulos A, Aslanides I, Asimellis G (2012) Correlation between epithelial thickness in normal corneas, untreated ectatic corneas, and ectatic corneas previously treated with CXL; is overall epithelial thickness a very early ectasia prognostic factor? Clin Ophthalmol 6:789–800. https://doi.org/10.2147/OPTH.S31524
Sella R, Zangwill LM, Weinreb RN, Afshari NA (2019) Repeatability and reproducibility of corneal epithelial thickness mapping with spectral-domain optical coherence tomography in normal and diseased cornea eyes. Am J Ophthalmol 197:88–97. https://doi.org/10.1016/j.ajo.2018.09.008
Ramos JLB, Li Y, Huang D (2009) Clinical and research applications of anterior segment optical coherence tomography–a review. J Clin Exp Ophthalmol 37:81–89. https://doi.org/10.1111/j.1442-9071.2008.01823.x
Han SB, Liu Y-C, Noriega KM, Mehta JS (2016) Applications of anterior segment optical coherence tomography in cornea and ocular surface diseases. J Ophthalmol 2016:4971572. https://doi.org/10.1155/2016/4971572
Fuentes E, Sandali O, El Sanharawi M, Basli E, Hamiche T, Goemaere I, Borderie V, Bouheraoua N, Laroche L (2015) Anatomic predictive factors of acute corneal hydrops in keratoconus: an optical coherence tomography study. Ophthalmology 122:1653–1659. https://doi.org/10.1016/j.ophtha.2015.04.031
Dong Y, Li D, Guo Z, Liu Y, Lin P, Lv B, Lv C, Xie G, Xie L (2022) Dissecting the profile of corneal thickness with keratoconus progression based on anterior segment optical coherence tomography. Front Neurosci 15:804273. https://doi.org/10.3389/fnins.2021.80427347
Kundu G, Shetty R, Khamar P, Mullick R, Gupta S, Nuijts R, Sinha Roy A (2021) Universal architecture of corneal segmental tomography biomarkers for artificial intelligence-driven diagnosis of early keratoconus. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319309
Khaled ML, Helwa I, Drewry M, Seremwe M, Estes A, Liu Y (2017) Molecular and histopathological changes associated with keratoconus. Biomed Res Int 2017:7803029. https://doi.org/10.1155/2017/7803029
Vinciguerra R, Ambrósio R Jr, Elsheikh A, Roberts CJ, Lopes B, Morenghi E, Azzolini C, Vinciguerra P (2016) Detection of keratoconus with a new biomechanical index. J Refract Surg 32:803–810. https://doi.org/10.3928/1081597x-20160629-01
Sedaghat MR, Momeni-Moghaddam H, Ambrósio R Jr, Heidari HR, Maddah N, Danesh Z, Sabzi F (2018) Diagnostic ability of corneal shape and biomechanical parameters for detecting frank keratoconus. Cornea 37:1025–1034. https://doi.org/10.1097/ico.0000000000001639
Yang K, Xu L, Fan Q, Gu Y, Song P, Zhang B, Zhao D, Pang C, Ren S (2020) Evaluation of new Corvis ST parameters in normal, Post-LASIK, Post-LASIK keratectasia and keratoconus eyes. Sci Rep 10:5676. https://doi.org/10.1038/s41598-020-62825-y
Machado AP, Lyra JM, Ambrósio R, Ribeiro G, Araújo LP, Xavier C, Costa E (2011) Comparing machine-learning classifiers in keratoconus diagnosis from ORA examinations. In: Peleg, M., Lavrač, N., Combi, C. (eds) Artificial Intelligence in Medicine. (Lecture Notes in Computer Science) Springer, Berlin Heidelberg New York, pp 90–95. https://doi.org/10.1007/978-3-642-22218-4_12
Pniakowska Z, Jurowski P (2016) Detection of the early keratoconus based on corneal biomechanical properties in the refractive surgery candidates. Indian J Ophthalmol 64:109–113. https://doi.org/10.4103/0301-4738.179725
Ambrósio R Jr, Lopes BT, Faria-Correia F, Salomão MQ, Bühren J, Roberts CJ, Elsheikh A, Vinciguerra R, Vinciguerra P (2017) Integration of Scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection. J Refract Surg 33:434–443. https://doi.org/10.3928/1081597x-20170426-02
Koc M, Aydemir E, Tekin K, Inanc M, Kosekahya P, Kiziltoprak H (2019) Biomechanical analysis of subclinical keratoconus with normal topographic, topometric, and tomographic findings. J Refract Surg 35:247–252. https://doi.org/10.3928/1081597x-20190226-01
Herber R, Pillunat LE, Raiskup F (2021) Development of a classification system based on corneal biomechanical properties using artificial intelligence predicting keratoconus severity. Eye Vis (Lond) 8:21. https://doi.org/10.1186/s40662-021-00244-4
Heidari Z, Mohammadpour M, Hashemi H, Jafarzadehpur E, Moghaddasi A, Yaseri M, Fotouhi A (2020) Early diagnosis of subclinical keratoconus by wavefront parameters using Scheimpflug, Placido and Hartmann-Shack based devices. Int Ophthalmol 40:1659–1671. https://doi.org/10.1007/s10792-020-01334-3
Carvalho LA (2005) Preliminary results of neural networks and zernike polynomials for classification of videokeratography maps. Optom Vis Sci 82:151–158. https://doi.org/10.1097/01.opx.0000153193.41554.a1
Castro-Luna GM, Martínez-Finkelshtein A, Ramos-López D (2020) Robust keratoconus detection with Bayesian network classifier for Placido-based corneal indices. Cont Lens Anterior Eye 43:366–372. https://doi.org/10.1016/j.clae.2019.12.006
de Almeida Jr GC, Guido RC, Neto JS, Rosa JM, Castiglioni L, de Mattos LC, Brandão CC (2021) Corneal Tomography Multivariate Index (CTMVI) effectively distinguishes healthy corneas from those susceptible to ectasia. Biomed Signal Process Control 70:102995. https://doi.org/10.1016/j.bspc.2021.102995
Saad A, Gatinel D (2012) Evaluation of total and corneal wavefront high order aberrations for the detection of forme fruste keratoconus. Invest Ophthalmol Vis Sci 53:2978–2992. https://doi.org/10.1167/iovs.11-8803
Elsawy A, Eleiwa T, Chase C, Ozcan E, Tolba M, Feuer W, Abdel-Mottaleb M, Abou Shousha M (2021) Multidisease deep learning neural network for the diagnosis of corneal diseases. Am J Ophthalmol 226:252–261. https://doi.org/10.1016/j.ajo.2021.01.018
Ruiz Hidalgo I, Rozema JJ, Saad A, Gatinel D, Rodriguez P, Zakaria N, Koppen C (2017) Validation of an objective keratoconus detection system implemented in a Scheimpflug tomographer and comparison with other methods. Cornea 36:689–695. https://doi.org/10.1097/ico.0000000000001194
Abdelmotaal H, Mostafa MM, Mostafa ANR, Mohamed AA, Abdelazeem K (2020) Classification of color-coded Scheimpflug camera corneal tomography images using deep learning. Transl Vis Sci Technol 9:30. https://doi.org/10.1167/tvst.9.13.30
Chen X, Zhao J, Iselin KC, Borroni D, Romano D, Gokul A, McGhee CNJ, Zhao Y, Sedaghat MR, Momeni-Moghaddam H, Ziaei M, Kaye S, Romano V, Zheng Y (2021) Keratoconus detection of changes using deep learning of colour-coded maps. BMJ Open Ophthalmol 6:e000824. https://doi.org/10.1136/bmjophth-2021-000824
Issarti I, Consejo A, Jiménez-García M, Hershko S, Koppen C, Rozema JJ (2019) Computer aided diagnosis for suspect keratoconus detection. Comput Biol Med 109:33–42. https://doi.org/10.1016/j.compbiomed.2019.04.024
Lopes BT, Ramos IC, Salomão MQ, Canedo ALC, Ambrósio R Jr (2015) Horizontal pachymetric profile for the detection of keratoconus. Rev Bras Oftalmol 74:382–385. https://doi.org/10.5935/0034-7280.20150080
Lopes BT, Ramos IC, Salomão MQ, Guerra FP, Schallhorn SC, Schallhorn JM, Vinciguerra R, Vinciguerra P, Price FW Jr, Price MO, Reinstein DZ, Archer TJ, Belin MW, Machado AP, Ambrósio R Jr (2018) Enhanced tomographic assessment to detect corneal ectasia based on artificial intelligence. Am J Ophthalmol 195:223–232. https://doi.org/10.1016/j.ajo.2018.08.005
Hidalgo IR, Rodriguez P, Rozema JJ, Dhubhghaill SN, Zakaria N, Tassignon M-J, Koppen C (2016) Evaluation of a machine-learning classifier for keratoconus detection based on Scheimpflug tomography. Cornea 35:827–832. https://doi.org/10.1097/ico.0000000000000834
Xie Y, Zhao L, Yang X, Wu X, Yang Y, Huang X, Liu F, Xu J, Lin L, Lin H, Feng Q, Lin H, Liu Q (2020) Screening candidates for refractive surgery with corneal tomographic-based deep learning. JAMA ophthalmol 138:519–526. https://doi.org/10.1001/jamaophthalmol.2020.0507
Saad A, Gatinel D (2010) Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci 51:5546–5555. https://doi.org/10.1167/iovs.10-5369
Zéboulon P, Debellemanière G, Gatinel D (2020) Unsupervised learning for large-scale corneal topography clustering. Sci Rep 10:16973. https://doi.org/10.1038/s41598-020-73902-7
Bessho K, Maeda N, Kuroda T, Fujikado T, Tano Y, Oshika T (2006) Automated keratoconus detection using height data of anterior and posterior corneal surfaces. Jpn J Ophthalmol 50:409–416. https://doi.org/10.1007/s10384-006-0349-6
Accardo PA, Pensiero S (2002) Neural network-based system for early keratoconus detection from corneal topography. J Biomed Inform 35:151–159. https://doi.org/10.1016/s1532-0464(02)00513-0
Saika M, Maeda N, Hirohara Y, Mihashi T, Fujikado T, Nishida K (2013) Four discriminant models for detecting keratoconus pattern using Zernike coefficients of corneal aberrations. Jpn J Ophthalmol 57:503–509. https://doi.org/10.1007/s10384-013-0269-1
Kamiya K, Ayatsuka Y, Kato Y, Shoji N, Mori Y, Miyata K (2021) Diagnosability of keratoconus using deep learning with Placido disk-based corneal topography. Front Med (Lausanne) 8:724902. https://doi.org/10.3389/fmed.2021.724902
Maeda N, Klyce SD, Smolek MK, Thompson HW (1994) Automated keratoconus screening with corneal topography analysis. Invest Ophthalmol Vis Sci 35:2749–2757
Arbelaez MC, Versaci F, Vestri G, Barboni P, Savini G (2012) Use of a support vector machine for keratoconus and subclinical keratoconus detection by topographic and tomographic data. Ophthalmology 119:2231–2238. https://doi.org/10.1016/j.ophtha.2012.06.005
Chandapura R, Salomão MQ, Ambrósio R Jr, Swarup R, Shetty R, Sinha Roy A (2019) Bowman’s topography for improved detection of early ectasia. J Biophotonics 12:e201900126. https://doi.org/10.1002/jbio.201900126
Elsawy A, Abdel-Mottaleb M (2021) A novel network with parallel resolution encoders for the diagnosis of corneal diseases. IEEE Trans Biomed Eng 68:3671–3680. https://doi.org/10.1109/tbme.2021.3082152
Yousefi S, Yousefi E, Takahashi H, Hayashi T, Tampo H, Inoda S, Arai Y, Asbell P (2018) Keratoconus severity identification using unsupervised machine learning. PLoS One 13:e0205998. https://doi.org/10.1371/journal.pone.0205998
Kamiya K, Ayatsuka Y, Kato Y, Fujimura F, Takahashi M, Shoji N, Mori Y, Miyata K (2019) Keratoconus detection using deep learning of colour-coded maps with anterior segment optical coherence tomography: a diagnostic accuracy study. BMJ Open 9:e031313. https://doi.org/10.1136/bmjopen-2019-031313
Shi C, Wang M, Zhu T, Zhang Y, Ye Y, Jiang J, Chen S, Lu F, Shen M (2020) Machine learning helps improve diagnostic ability of subclinical keratoconus using Scheimpflug and OCT imaging modalities. Eye Vis (Lond) 7:48. https://doi.org/10.1186/s40662-020-00213-3
Karimi A, Meimani N, Razaghi R, Rahmati SM, Jadidi K, Rostami M (2018) Biomechanics of the healthy and keratoconic corneas: a combination of the clinical data, finite element analysis, and artificial neural network. Curr Pharm Des 24:4474–4483. https://doi.org/10.2174/1381612825666181224123939
Castro-Luna G, Jiménez-Rodríguez D, Castaño-Fernández AB, Pérez-Rueda A (2021) Diagnosis of subclinical keratoconus based on machine learning techniques. J Clin Med 10:4281. https://doi.org/10.3390/jcm10184281
Temstet C, Sandali O, Bouheraoua N, Hamiche T, Galan A, El Sanharawi M, Basli E, Laroche L, Borderie V (2015) Corneal epithelial thickness mapping using Fourier-domain optical coherence tomography for detection of form fruste keratoconus. J Cataract Refract Surg 41:812–820. https://doi.org/10.1016/j.jcrs.2014.06.043
Dos Santos VA, Schmetterer L, Stegmann H, Pfister M, Messner A, Schmidinger G, Garhofer G, Werkmeister RM (2019) CorneaNet: fast segmentation of cornea OCT scans of healthy and keratoconic eyes using deep learning. Biomed Opt Express 10:622–641. https://doi.org/10.1364/boe.10.000622
Hwang ES, Perez-Straziota CE, Kim SW, Santhiago MR, Randleman JB (2018) Distinguishing highly asymmetric keratoconus eyes using combined Scheimpflug and spectral-domain OCT analysis. Ophthalmology 125:1862–1871. https://doi.org/10.1016/j.ophtha.2018.06.020
Issarti I, Consejo A, Jiménez-García M, Kreps EO, Koppen C, Rozema JJ (2020) Logistic index for keratoconus detection and severity scoring (Logik). Comput Biol Med 122:103809. https://doi.org/10.1016/j.compbiomed.2020.103809
Author information
Authors and Affiliations
Contributions
Conceptualization: Hassan Hashemi, Farideh Doroodgar, and Zahra Heidari; methodology: Zahra Heidari and Mehdi Khabazkhoob; literature search and data analysis: Zahra Heidari and Mehdi Khabazkhoob; writing—original draft preparation: Zahra Heidari; review and editing: all authors; supervision: Hassan Hashemi. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
An ethics statement is not applicable because this study is based exclusively on published literature.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has not been presented at any meeting.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hashemi, H., Doroodgar, F., Niazi, S. et al. Comparison of different corneal imaging modalities using artificial intelligence for diagnosis of keratoconus: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 262, 1017–1039 (2024). https://doi.org/10.1007/s00417-023-06154-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06154-6