Abstract
Purpose
To assess how eye axes and multifocal intraocular lens (MIOL) centration may impact the light distortion index (LDI) and ocular scatter index (OSI).
Methods
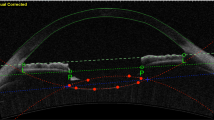
Fifty-eight subjects implanted with the trifocal MIOL Q-Flex M 640PM or Liberty 677MY (Medicontur) were included in this retrospective analysis. The following variables were collected with the Pentacam Wave (Oculus) considering the vertex normal as the coordinates center: chord-mu to the center of the pupil, chord-alpha to the geometrical center of the cornea, and chord-MIOL to the center of the diffractive ring. These measurements were correlated with OSI (HD Analyzer, Visiometrics) and LDI (light distortion analyzer, CEORLab).
Results
Chord-MIOL centroid was 0.12 mm at 62°, chord-mu was 0.09 mm at 174°, and chord-alpha was 0.38 mm at 188°. A relationship was found between OSI and LDI, rho = 0.58, p < 0.0005). No relationships were found between chord-mu or chord-alpha and the LDI or OSI, neither for the total magnitude, nor the decomposition in orthogonal components (p > 0.05). The LDI was significantly correlated with the temporal centration of the MIOL versus the vertex normal (rho = 0.32, p = 0.02).
Conclusions
As opposed to what has been previously described, the temporal centration of the MIOL was related to a decrease in the LDI. Future studies with extreme values of the included variables are required to establish cut-offs for considering these variables as exclusion criteria in the implantation of a MIOL.



Similar content being viewed by others
References
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2021) What we have learnt from 30 years living with positive dysphotopsia after intraocular lens implantation?: a review. Expert Rev Ophthalmol 16:1–10. https://doi.org/10.1080/17469899.2021.1917997
Kim EC, Na K-S, Kim HS, Hwang HS (2020) How does the world appear to patients with multifocal intraocular lenses?: a mobile model eye experiment. Bmc Ophthalmol 20:180. https://doi.org/10.1186/s12886-020-01446-5
Alba-Bueno F, Vega F, Millán MS (2014) Halos y lentes intraoculares multifocales: origen e interpretación. Arch Soc Esp Oftalmol 89:397–404. https://doi.org/10.1016/j.oftal.2014.01.002
Alba-Bueno F, Garzón N, Vega F et al (2017) Patient-perceived and laboratory-measured halos associated with diffractive bifocal and trifocal intraocular lenses. Curr Eye Res 43:1–8. https://doi.org/10.1080/02713683.2017.1379541
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2021) Long-term efficacy, visual performance and patient reported outcomes with a trifocal intraocular lens: a six-year follow-up. J Clin Medicine 10:2009. https://doi.org/10.3390/jcm10092009
Mendicute J, Kapp A, Lévy P et al (2016) Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg 42:203–210. https://doi.org/10.1016/j.jcrs.2015.11.037
Liu X, Xie L, Huang Y (2018) Comparison of the visual performance after implantation of bifocal and trifocal intraocular lenses having an identical platform. J Refract Surg 34:273–280. https://doi.org/10.3928/1081597x-20180214-01
Győry JF, Srinivasan S, Madár E, Balla L (2021) Long-term performance of a diffractive–refractive trifocal IOL with centralized diffractive rings: 5-year prospective clinical trial. J Cataract Refr Surg 47:1258–1264. https://doi.org/10.1097/j.jcrs.0000000000000670
Ison M, Scott J, Apel J, Apel A (2021) Patient expectation, satisfaction and clinical outcomes with a new multifocal intraocular lens. Clin Ophthalmol 15:4131–4140. https://doi.org/10.2147/opth.s327424
Modi S, Lehmann R, Maxwell A et al (2021) Visual and patient-reported outcomes of a diffractive trifocal intraocular lens compared with those of a monofocal intraocular lens. Ophthalmology 128:197–207. https://doi.org/10.1016/j.ophtha.2020.07.015
Monaco G, Gari M, Censo FD et al (2017) Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg 43:737–747. https://doi.org/10.1016/j.jcrs.2017.03.037
Negishi K, Hayashi K, Kamiya K et al (2019) Nationwide prospective cohort study on cataract surgery with multifocal intraocular lens implantation in Japan. Am J Ophthalmol 208:133–144. https://doi.org/10.1016/j.ajo.2019.07.019
Woodward MA, Randleman JB, Stulting RD (2009) Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg 35:992–997. https://doi.org/10.1016/j.jcrs.2009.01.031
de Vries NE, Webers CAB, Touwslager WRH et al (2011) Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg 37:859–865. https://doi.org/10.1016/j.jcrs.2010.11.032
Espaillat A, Coelho C, Batista MJM, Perez O (2021) Predictors of photic phenomena with a trifocal IOL. Clin Ophthalmol Auckl N Z 15:495–503. https://doi.org/10.2147/opth.s282469
Karhanová M, Marešová K, Pluháček F et al (2013) The importance of angle kappa for centration of multifocal intraocular lenses. Cesk Slov Oftalmol 69:64–68
Prakash G, Prakash DR, Agarwal A et al (2011) Predictive factor and kappa angle analysis for visual satisfactions in patients with multifocal IOL implantation. Eye 25:1187–1193. https://doi.org/10.1038/eye.2011.150
Holladay JT (2019) Apparent chord mu and actual chord mu and their clinical value. J Cataract Refract Surg 45:1198–1199. https://doi.org/10.1016/j.jcrs.2019.03.029
Rodríguez-Vallejo M, Piñero DP, Fernández J (2018) Avoiding misinterpretations of kappa angle for clinical research studies with Pentacam. J Optometry 12:71–73. https://doi.org/10.1016/j.optom.2018.03.003
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2019) Prediction of visual acuity and contrast sensitivity from optical simulations with multifocal intraocular lenses. J Refract Surg 35:789–795. https://doi.org/10.3928/1081597x-20191024-01
Artal P, Benito A, Pérez GM et al (2011) An objective scatter index based on double-pass retinal images of a point source to classify cataracts. Plos One 6:e16823. https://doi.org/10.1371/journal.pone.0016823.g002
Kohnen T, Suryakumar R (2021) Measures of visual disturbance in patients receiving extended depth-of-focus or trifocal intraocular lenses. J Cataract Refr Surg 47:245–255. https://doi.org/10.1097/j.jcrs.0000000000000364
Ferreira-Neves H, Macedo-de-Araújo R, Rico-del-Viejo L et al (2015) Validation of a method to measure light distortion surrounding a source of glare. J Biomed Opt 20:075002–075002. https://doi.org/10.1117/1.jbo.20.7.075002
Armstrong RA (2013) Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthal Physl Opt 33:7–14. https://doi.org/10.1111/opo.12009
Qi Y, Lin J, Leng L et al (2018) Role of angle κ in visual quality in patients with a trifocal diffractive intraocular lens. J Cataract Refract Surg 44:949–954. https://doi.org/10.1016/j.jcrs.2018.05.026
Cervantes-Coste G, Tapia A, Corredor-Ortega C et al (2022) The influence of angle alpha, angle kappa, and optical aberrations on visual outcomes after the implantation of a high-addition trifocal IOL. J Clin Medicine 11:896. https://doi.org/10.3390/jcm11030896
Garzón N, García-Montero M, López-Artero E et al (2020) Influence of angle κ on visual and refractive outcomes after implantation of a diffractive trifocal intraocular lens. J Cataract Refr Surg 46:721–727. https://doi.org/10.1097/j.jcrs.0000000000000156
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2018) Biometric factors associated with the visual performance of a high addition multifocal intraocular lens. Curr Eye Res 43:998–1005. https://doi.org/10.1080/02713683.2018.1478981
Luo J, Liu Y, Wang F et al (2021) Effect of the kappa angle on depth of focus after implantation of the TECNIS Symfony intraocular lens. Int Ophthalmol 41:2513–2520. https://doi.org/10.1007/s10792-021-01809-x
Fu Y, Kou J, Chen D et al (2019) Influence of angle kappa and angle alpha on visual quality after implantation of multifocal intraocular lenses. J Cataract Refract Surg 45:1258–1264. https://doi.org/10.1016/j.jcrs.2019.04.003
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2018) From presbyopia to cataracts: a critical review on dysfunctional lens syndrome. J Ophthalmol 2018:1–10. https://doi.org/10.1155/2018/4318405
Wang R, Long T, Gu X, Ma T (2020) Changes in angle kappa and angle alpha before and after cataract surgery. J Cataract Refr Surg 46:365–371. https://doi.org/10.1097/j.jcrs.0000000000000063
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2020) Pupil diameter in patients with multifocal intraocular lenses. J Refract Surg 36:750–756. https://doi.org/10.3928/1081597x-20200813-01
Qin M, Ji M, Zhou T et al (2022) Influence of angle alpha on visual quality after implantation of extended depth of focus intraocular lenses. Bmc Ophthalmol 22:82. https://doi.org/10.1186/s12886-022-02302-4
Hashemi H, KhabazKhoob M, Yazdani K et al (2010) Distribution of angle kappa measurements with orbscan II in a population-based survey. J Refract Surg 26:966–971. https://doi.org/10.3928/1081597x-20100114-06
Reinstein DZ, Archer TJ, Rowe EL et al (2021) Distribution of pupil offset and angle kappa in a refractive surgery preoperative population of 750 myopic, emmetropic, and hyperopic eyes. J Refract Surg 37:49–58. https://doi.org/10.3928/1081597x-20201109-01
Wang L, de Souza RG, Weikert MP, Koch DD (2019) Evaluation of crystalline lens and intraocular lens tilt using a swept-source optical coherence tomography biometer. J Cataract Refract Surg 45:35–40. https://doi.org/10.1016/j.jcrs.2018.08.025
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2020) Patient selection to optimize near vision performance with a low-addition trifocal lens. J Optometry 13:50–58. https://doi.org/10.1016/j.optom.2019.06.003
Tandogan T, Son HS, Choi CY et al (2017) Laboratory evaluation of the influence of decentration and pupil size on the optical performance of a monofocal, bifocal, and trifocal intraocular lens. J Refract Surg 33:808–812. https://doi.org/10.3928/1081597x-20171004-02
Kimura S, Morizane Y, Shiode Y et al (2017) Assessment of tilt and decentration of crystalline lens and intraocular lens relative to the corneal topographic axis using anterior segment optical coherence tomography. Plos One 12:e0184066. https://doi.org/10.1371/journal.pone.0184066
Fernández J, Burguera N, Rocha-de-Lossada C et al (2022) A new approach for detecting patients complaining of dysphotopsia after multifocal intraocular lens implantation due to non-optical reasons. In: 26th ESCRS Winter Meeting, Portugal. Available at: https://wintermeeting.2022.escrs.org/programme/. Accessed 5 March 2023
Mahr MA, Simpson MJ, Erie JC (2020) Angle alpha orientation and magnitude distribution in a cataract surgery population. J Cataract Refr Surg 46:372–377. https://doi.org/10.1097/j.jcrs.0000000000000066
Meng J, Du Y, Wei L et al (2021) Distribution of angle α and angle κ in a population with cataract in Shanghai. J Cataract Refr Surg 47:579–584. https://doi.org/10.1097/j.jcrs.0000000000000490
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Research, Almería Center, Torrecárdenas Hospital Complex, and conducted in adherence with the tenets of the Declaration of Helsinki. For this type of study, formal consent is not required.
Conflict of interest
Dr. Fernández is a consultant to Medicontur. The remaining authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fernández, J., Burguera, N., Rocha-de-Lossada, C. et al. Influence of a multifocal intraocular lens centration and eye angles on light distortion and ocular scatter index. Graefes Arch Clin Exp Ophthalmol 261, 2291–2299 (2023). https://doi.org/10.1007/s00417-023-06028-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06028-x