Abstract
Purpose
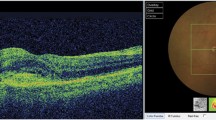
To characterize retinoschisis in a large series using spectral domain optical coherence tomography (SD-OCT), including rates of schisis detachment and macular involvement in cases of peripheral retinoschisis.
Methods
In this retrospective, cross-sectional, descriptive study, consecutive patients with diagnosis of retinoschisis in at least one eye were identified using billing codes between January 2012 and May 2021. Charts were reviewed to verify diagnosis of retinoschisis or schisis detachment. SD-OCT and clinical examination was used to identify frequency of macular schisis, peripheral schisis, and schisis detachment, and characteristics of retinoschisis including frequency of inner and outer wall breaks, distribution of layers split, and location of involvement of peripheral pathology. SD-OCT images of insufficient quality were excluded from the pertinent analysis.
Results
281 eyes of 191 patients were included. 195 (69.4%) eyes had peripheral retinoschisis, 15 (5.3%) had schisis detachment, 66 (23.5%) had macular retinoschisis alone, and 5 (1.8%) had combined macular and peripheral retinoschisis. Of the eyes without macular retinoschisis, 7.0% had schisis detachment. Of the remainder, 4 (2.1%) had inner wall breaks, and 24 (12.3%) had outer wall breaks. In eyes with peripheral retinoschisis, splitting occurred in the outer plexiform layer in 58.9%, the retinal nerve fiber layer in 8.9%, a combination of layers in 26.8%, and indeterminate in 5.4%. Location of peripheral involvement was inferotemporal in 58.5%, superotemporal in 14.1%, temporal in 13.7%, and inferior in 12.2%.
Conclusion
SD-OCT helped to identify the presence of schisis detachment and breaks, confirmed diagnosis in challenging cases, and demonstrated the layer of splitting within the neurosensory retina. This series represents the largest such study to date.



Similar content being viewed by others
References
Byer NE (1968) Clinical study of senile retinoschisis. Arch Ophthalmol (Chicago, Ill : 1960) 79:36–44. https://doi.org/10.1001/archopht.1968.03850040038012
Byer NE (2002) Perspectives on the management of the complications of senile retinoschisis. Eye 16:359–364. https://doi.org/10.1038/sj.eye.6700191
Byer NE (1986) Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology 93:1127–1137. https://doi.org/10.1016/s0161-6420(86)33601-7
Foos RY (1970) Senile retinoschisis. Relationship to cystoid degeneration. Trans - Am Acad Ophthalmol Otolaryngol Am Acad Ophthalmol Otolaryngol 74:33–51
Straatsma BR, Foss RY (1973) Typical and reticular degenerative retinoschisis. Am J Ophthalmol 75:551–575. https://doi.org/10.1016/0002-9394(73)90809-x
Xue K, Muqit MMK, Ezra E, Charles SJ, Yorston D, Mitra A, Patel CK (2017) Incidence, mechanism and outcomes of schisis retinal detachments revealed through a prospective population-based study. Br J Ophthalmol 101:1022–1026. https://doi.org/10.1136/bjophthalmol-2016-309750
Jeroudi AM, Shah V, Blinder KJ, Shah GK (2017) Management of degenerative retinoschisis-associated retinal detachment. Ophthalmology Retina 1:266–271. https://doi.org/10.1016/j.oret.2017.01.012
Clemens S, Busse H, Gerding H, Hoffmann P (1995) Treatment guidelines in various stages of senile retinoschisis. Klin Monatsbl Augenheilkd 206:83–91. https://doi.org/10.1055/s-2008-1035409
Sauer CG, Gehrig A, Warneke-Wittstock R, Marquardt A, Ewing CC, Gibson A, Lorenz B, Jurklies B, Weber BH (1997) Positional cloning of the gene associated with X-linked juvenile retinoschisis. Nat Genet 17:164–170. https://doi.org/10.1038/ng1097-164
Yu J, Ni Y, Keane PA, Jiang C, Wang W, Xu G (2010) Foveomacular schisis in juvenile X-linked retinoschisis: an optical coherence tomography study. Am J Ophthalmol 149:973-978.e972. https://doi.org/10.1016/j.ajo.2010.01.031
Hoerauf H, Joachimmeyer E, Laqua H (2001) Senile schisis detachment with posterior outer layer breaks. Retina 21:602–612. https://doi.org/10.1097/00006982-200112000-00007
Rachitskaya AV, Yuan A, Singh RP, Sears JE, Schachat AP (2017) Optical coherence tomography of outer retinal holes in senile retinoschisis and schisis-detachment. Br J Ophthalmol 101:445–448. https://doi.org/10.1136/bjophthalmol-2016-308551
Huang NT, Georgiadis C, Gomez J, Tang PH, Drayna P, Koozekanani DD, van Kuijk F, Montezuma SR (2020) Comparing fundus autofluorescence and infrared imaging findings of peripheral retinoschisis, schisis detachment, and retinal detachment. Am J Ophthalmol Case Rep 18:100666. https://doi.org/10.1016/j.ajoc.2020.100666
Buch H, Vinding T, Nielsen NV (2007) Prevalence and long-term natural course of retinoschisis among elderly individuals: the Copenhagen City Eye Study. Ophthalmology 114:751–755. https://doi.org/10.1016/j.ophtha.2006.08.039
Watzke RC, Folk JC, Lauer AK (2013) Foveal involvement by acquired retinoschisis: long-term visual outcomes. Retina 33:606–612. https://doi.org/10.1097/IAE.0b013e3182695a6f
Eibenberger K, Sacu S, Rezar-Dreindl S, Pöcksteiner J, Georgopoulos M, Schmidt-Erfurth U (2017) Monitoring retinoschisis and non-acute retinal detachment by optical coherence tomography: morphologic aspects and clinical impact. Acta Ophthalmol 95:710–716. https://doi.org/10.1111/aos.13424
Yeoh J, Rahman W, Chen FK, da Cruz L (2012) Use of spectral-domain optical coherence tomography to differentiate acquired retinoschisis from retinal detachment in difficult cases. Retina 32:1574–1580. https://doi.org/10.1097/IAE.0b013e3182411d90
Ip M, Garza-Karren C, Duker JS, Reichel E, Swartz JC, Amirikia A, Puliafito CA (1999) Differentiation of degenerative retinoschisis from retinal detachment using optical coherence tomography. Ophthalmology 106:600–605. https://doi.org/10.1016/s0161-6420(99)90123-9
Ho VY, Wehmeier JM, Shah GK (2016) Wide-field infrared imaging: a descriptive review of characteristics of retinoschisis, retinal detachment, and schisis detachments. Retina 36:1439–1445. https://doi.org/10.1097/iae.0000000000000963
Thanos A, Todorich B, Pasadhika S, Khundkar T, Xu D, Jain A, Ung C, Faia LJ, Capone A Jr, Williams GA, Yonekawa Y, Sarraf D, Wolfe JD (2019) Degenerative peripheral retinoschisis: observations from ultra-widefield fundus imaging. Ophthalmic Surg Lasers Imaging Retina 50:557–564. https://doi.org/10.3928/23258160-20190905-04
Nadelmann JB, Gupta MP, Kiss S, Askin G, Chan RVP, Papakostas T, D’Amico DJ, Orlin A (2019) Ultra-widefield autofluorescence imaging of retinal detachment compared to retinoschisis. Ophthalmic Surg Lasers Imaging Retina 50:550–556. https://doi.org/10.3928/23258160-20190905-03
Palma-Carvajal F, Figueroa-Vercellino JP, Salazar Á, González H, Giralt J (2019) Multimodal imaging in senile retinoschisis. Journal francais d’ophtalmologie 42:800–802. https://doi.org/10.1016/j.jfo.2018.12.016
Funding
This study was funded by the Retina Research and Development Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the Institutional Review Board of St. Luke’s Hospital in Chesterfield, Missouri, USA, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not needed for this study as it was retrospective and observational in nature.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jalalizadeh, R.A., Smith, B.T. Characterization and diagnosis of retinoschisis and schisis detachments using spectral domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 261, 375–380 (2023). https://doi.org/10.1007/s00417-022-05801-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05801-8