Abstract
Purpose
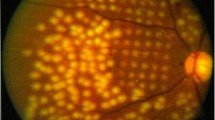
To assess the effect of switching to brolucizumab from aflibercept on eyes with type 1 macular neovascularization (MNV) and polypoidal choroidal vasculopathy (PCV) at 18 months.
Methods
This study was a retrospective, observational case series that included 19 eyes of 19 patients with type 1MNV and 23 eyes of 22 patients with PCV. We compared the injection intervals, visual acuity, total lesion size, and the number of polypoidal lesions between baseline and 18 months. The correlations between the data including treatment interval, total lesion size, and the number of polyps were also assessed.
Results
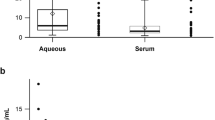
Treatment intervals were significantly extended; from 7.4 ± 1.4 weeks to 11.6 ± 2.6 weeks for type 1 MNV, p < 0.001; from 6.9 ± 1.3 to 11.7 ± 3.1 weeks for PCV, p < 0.001. In type 1 MNV eyes, strong correlation was found between total lesion size and brolucizumab injection intervals (r = − 0.81; p = 0.0002) and moderate correlation was found between treatment frequency with aflibercept and that with brolucizumab (r = 0.76; p = 0.040). In PCV eyes, we found strong correlation between the number of polyps and brolucizumab treatment frequency (r = − 0.81; p = 0.0016) and moderate correlation between total lesion size and brolucizumab treatment interval (r = − 0.48; p = 0.034). Intraocular inflammation occurred in 2 of 19 eyes (10.3%) with type 1 MNV and 5 of 23 eyes (21.7%) with PCV.
Conclusion
The properties to extend brolucizumab injection intervals might be the smaller lesion size and lower aflibercept frequency for type 1 MNV and the smaller number of polyps and the smaller size of lesion for PCV.



Similar content being viewed by others
References
Traine PG, Pfster IB, Zandi S et al (2019) Long term outcome of intravitreal afibercept treatment for neovascular age-related macular degeneration using a “treat-and-extend” regimen. Ophthalmol Retina 3:393–399. https://doi.org/10.1016/j.oret.2019.01.018
DeCroos FC, Reed D, Adam MK et al (2017) Treat-and-extend therapy using afibercept for neovascular age-related macular degeneration: a prospective clinical trial. Am J Ophthalmol 180:142–150. https://doi.org/10.1016/j.ajo.2017.06.002
Ohji M, Takahashi K, Okada AA et al (2020) Efcacy and safety of intravitreal afibercept treat and-extend regimens in exudative age-related macular degeneration: 52- and 96-week fndings from ALTAIR: a randomized controlled trial. Adv Ther 37:1173–1187. https://doi.org/10.1007/s12325-020-01236-x
Nguyen QD, Das A, Do DV et al (2020) Brolucizumab: evolution through preclinical and clinical studies and the implications for the management of neovascular age-related macular degeneration. Ophthalmology 127(7):963–976. https://doi.org/10.1016/j.ophtha.2019.12.031
Hussain RM, Neal A, Yannuzzi NA et al (2021) Brolucizumab for persistent macular fluid in neovascular age-related macular degeneration after prior anti-VEGF treatments. Ther Adv Ophthalmol 13:25158414211055964. https://doi.org/10.1177/25158414211055964
Boltz A, Radunsky K, Weingessesl B et al (2022) Brolucizumab for pre-treated patients with choroidal neovascularization and signs of tachyphylaxis to afibercept and bevacizumab. Graefes Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s00417-022-05634-5
Ota H, Takeuchi J, Nakano Y et al (2022) Switching from afibercept to brolucizumab for the treatment of refractory neovascular age-related macular degeneration. Jpn J Ophthalmol. https://doi.org/10.1007/s10384-022-00908-1
Haensli C, Pfister IB, Garweg JG (2021) Switching to brolucizumab in neovascular age-related macular degeneration incompletely responsive to ranibizumab or aflibercept: real-life 6 month outcomes. J Clin Med 10(12):2666. https://doi.org/10.3390/jcm10122666
Spaide RF, Jaffe GJ, Sarraf D et al (2020) Consensus nomenclature for reporting neovascular age-related macular degeneration data: Consensus on Neovascular Age-Related Macular Degeneration Nomenclature Study Group. Ophthalmology 127(5):616–636. https://doi.org/10.1016/j.ophtha.2019.11.004
Freund KB, Zweifel SA, Engelbert M (2010) Do we need a new classification for choroidal neovascularization in age-related macular degeneration? Retina 30(9):1333–1349. https://doi.org/10.1097/IAE.0b013e3181e7976b
Koh A, Lee WK, Chen LJ et al (2012) EVEREST study: efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina 32(8):1453–1464. https://doi.org/10.1097/IAE.0b013e31824f91e8
Fujita A, Kataoka K, Takeuchi J et al (2020) Diagnostic characteristics of polypoidal choroidal vasculopathy based on B-scan swept-source optical coherence tomography angiography and its interrater agreement compared with indocyanine green angiography. Retina 40(12):2296–2303. https://doi.org/10.1097/IAE.0000000000002760
Tamashiro T, Tanaka K, Itagaki K et al (2022) Subfoveal choroidal thickness after brolucizumab therapy for neovascular age-related macular degeneration: a short-term multicenter study. Graefes Arch Clin Exp Ophthalmol. https://doi.org/10.1007/s00417-021-05517-1
Fukuda Y, Sakurada Y, Matsubara M et al (2021) Comparison of outcomes between 3 monthly brolucizumab and aflibercept injections for polypoidal choroidal vasculopathy. Biomedicines 9(9):1164. https://doi.org/10.3390/biomedicines9091164
Yamazaki T, Koizumi H, Yamagishi T et al (2012) Subfoveal choroidal thickness after ranibizumab therapy for neovascular age-related macular degeneration: 12-month results. Ophthalmology 119:1621–1627. https://doi.org/10.1016/j.ophtha.2012.02.022
Koizumi H, Kano M, Yamamoto A et al (2015) Short-term changes in choroidal thickness after afibercept therapy for neovascular age-related macular degeneration. Am J Ophthalmol 159(627–633):e621. https://doi.org/10.1016/j.ajo.2014.12.025
Kikushima W, Sakurada Y, Yoneyama S et al (2017) Incidence and risk factors of retreatment after three-monthly afibercept therapy for exudative age-related macular degeneration. Sci Rep 7:44020. https://doi.org/10.1038/srep44020
Morimoto M, Matsumoto H, Mimura K et al (2017) Two-year results of a treat-and-extend regimen with aflibercept for polypoidal choroidal vasculopathy. Graefes Arch Clin Exp Ophthalmol 255:1891–1897. https://doi.org/10.1007/s00417-017-3718-6
Ellabban AA, Tsujikawa A, Ogino K et al (2012) Choroidal thickness after intravitreal ranibizumab injections for choroidal neovascularization. Clin Ophthalmol 6:837–844. https://doi.org/10.2147/OPTH.S30907
Heier JS, Brown DM, Chong V et al (2012) Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 119(12):2537–2548. https://doi.org/10.1016/j.ophtha.2012.09.006
Martin DF, Maguire MG, Fine SL et al (2012) Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology 119(7):1388–1398. https://doi.org/10.1016/j.ophtha.2012.03.053
Rosenfeld PJ, Brown DM, Heier JS et al (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355(14):1419–1431. https://doi.org/10.1056/NEJMoa054481
Brown DM, Kaiser PK, Michels M et al (2006) Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 355(14):1432–1444. https://doi.org/10.1056/NEJMoa062655
Kuehlewein L, Bansal M, Lenis TL et al (2015) Optical coherence tomography angiography of type 1 neovascularization in age-related macular degeneration. Am J Ophthalmol 160(4):739-748.e2. https://doi.org/10.1016/j.ajo.2015.06.030
Xu D, Davila JP, Rahimi M et al (2018) Long-term progression of type 1 neovascularization in age-related macular degeneration using optical coherence tomography angiography. Am J Ophthalmol 187:10–20. https://doi.org/10.1016/j.ajo.2017.12.005
Matsumoto H, Hoshino J, Mykai R et al (2021) Short-term outcomes of intravitreal brolucizumab for treatment-naïve neovascular age-related macular degeneration with type 1 choroidal neovascularization including polypoidal choroidal vasculopathy. Sci Rep 11(1):6759. https://doi.org/10.1038/s41598-021-86014-7
Haug SJ, Hien DL, Uludag G et al (2020) Retinal arterial occlusive vasculitis following intravitreal brolucizumab administration. Am J Ophthalmol Case Rep 31(18):100680. https://doi.org/10.1016/j.ajoc.2020.100680
Baumal CR, Spaide RF, Vajzovic L et al (2020) Retinal vasculitis and intraocular inflammation after intravitreal injection of brolucizumab. Ophthalmology 127(10):1345–1359. https://doi.org/10.1016/j.ophtha.2020.04.017
Monés J, Srivastava SK, Jaffe GJ et al (2021) Risk of inflammation, retinal vasculitis, and retinal occlusion-related events with brolucizumab: post hoc review of HAWK and HARRIER. Ophthalmology 128(7):1050–1059. https://doi.org/10.1016/j.ophtha.2020.11.011
Baumal CR, Bodaghi B, Singer M et al (2021) Expert opinion on management of intraocular inflammation, retinal vasculitis, and vascular occlusion after brolucizumab treatment. Ophthalmol Retina 5(6):519–527. https://doi.org/10.1016/j.oret.2020.09.020
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of the Institutional Review Board of the University of Toyama and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ueda-Consolvo, T., Tanigichi, A., Numata, A. et al. Switching to brolucizumab from aflibercept in age-related macular degeneration with type 1 macular neovascularization and polypoidal choroidal vasculopathy: an 18-month follow-up study. Graefes Arch Clin Exp Ophthalmol 261, 345–352 (2023). https://doi.org/10.1007/s00417-022-05793-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05793-5