Abstract
Purpose
To evaluate the impact of postponed care attributed to coronavirus disease (COVID-19) pandemic lockdowns on visual acuity and the number of anti-VEGF injections in patients with retinal vein occlusion (RVO).
Methods
A multicenter, retrospective study of consecutive RVO patients previously treated with anti-VEGF injections, which compared data from pre- (2019) and during (2020) COVID-19 lockdown period.
Results
A total of 814 RVO patients with a mean age of 72.8 years met the inclusion criteria. Of them, 439 patients were assessed in 2019 and 375 in 2020. There was no significant difference between the COVID-19 and pre-COVID-19 period in terms of baseline and final BCVA (p = 0.7 and 0.9 respectively), but there was a significantly reduced mean number of anti-VEGF injections during the COVID-19 period (5.0 and. 5.9 respectively, p < 0.01), with a constant lower ratio of injections per patient. A noticeable decline was found during March–May (p < 0.01) in 2020. Baseline BCVA (0.69, p < 0.01) and the number of injections (− 0.01, p = 0.01) were predictors of final BCVA.
Conclusions
In a large cohort of RVO patients, during 2020 lockdowns imposed due to the COVID-19 pandemic, a significant reduction in the annual number of anti-VEGF injections was noted. The postponed care did not result in a significant impact on the final BCVA. Baseline BCVA and the number of annual injections serve as predictors for final BCVA in RVO patients.

Similar content being viewed by others
Introduction
Retinal vein occlusion (RVO) is the second leading cause of retinal vascular vision loss after diabetic retinopathy [1,2,3]. Several risk factors were reported by previous studies to be associated with RVO, including advanced age, hypertension, and other cardiovascular risk factors such as diabetes mellitus, hyperlipidemia, and smoking [4,5,6]. RVO can be classified as central retinal vein occlusion (CRVO) and branch retinal vein occlusion (BRVO). RVO causes an increased retinal vascular permeability due to upregulation of vascular endothelial growth factor (VEGF) expression [7], which leads to several complications, including macular edema (ME) and macular ischemia [2]. The gold standard treatment for ME caused by RVO is intravitreal injections of anti-VEGF [7,8,9]. Currently, two anti-VEGF agents are FDA approved for this purpose, ranibizumab and aflibercept. Bevacizumab is used as well but on an off-label basis. Studies report no statistically significant visual acuity (VA) disparity between groups treated with different drugs [8, 10]. There are three RVO treatment regimens: fixed monthly injections, treat and extend (TE), and pro re nata (PRN). Each strategy has benefits and downsides, and today, the choice of regimen is subjected to ophthalmologists' discretion [11]. It is agreeable by most ophthalmologists to start treatment with a loading dose of 3 monthly injections in order to achieve visual stability [8, 11].
In 2020, several lockdowns were applied by governments to reduce the coronavirus (COVID-19) spreadment. Quarantines disrupted routine, non-emergency medical care and limited it to the urgent one. At the same time, for their part, patients tried to avoid exposure to the virus by delaying and avoiding elective visits [12]. During that period, patients received a reduced number of injections and less frequent medical follow-ups, which was associated with adverse outcomes in patients with RVO [13].
The purpose of this study is to investigate the impact of postponed care secondary to COVID-19 in patients with RVO, by evaluating the change in the best-corrected visual acuity (BCVA) and the number of injections during this period.
Methods
A retrospective, multi-center, observational study of consecutive patients with RVO seen by retina specialists between 1.1.2019 and 31.12.2020 at the ophthalmology departments of Meir Medical Center, Kfar Saba, Israel, and Tel Aviv Sourasky Medical Center, Tel Aviv, Israel. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of the mentioned above medical centers.
Cases were identified by electronic medical records (EMR) of each department. The inclusion criteria were the presence of RVO, defined by a characteristic appearance on the clinical examination and auxiliary tests. The findings on the clinical exam consisted of flame-shaped retinal hemorrhages, cotton wool spots, exudates, retinal edema, dilated tortuous veins, venous collaterals formation, or vascular sheathing. Cystoid macular edema, hyperreflective foci, and/or subretinal fluid were present on OCT exam and delayed filling of the occluded retinal vein with varying degrees of capillary nonperfusion, blockage from intraretinal hemorrhages, and macular edema — on fluorescein angiography [2, 14]. All included patients received a loading dose of three monthly injections of bevacizumab in both periods, followed by further anti-VEGF treatment (ranibizumab, aflibercept, or bevacizumab) according to the response and had follow-up during 1st and last quarters of 2019 or 2020. Since the variance between eyes is usually less than that between subjects, the overall variance of a sample of measurements combined from both eyes is likely to underestimate the true variance. Therefore, if both eyes met the inclusion criteria, the right eye was selected [15].
Exclusion criteria were high myopia of above 6 diopters, history of retinal detachment, central serous chorioretinopathy, diabetic retinopathy, macular telangiectasias, tractional and degenerative lamellar macular holes, age-related macular degeneration, central or branch retinal artery occlusion, optic neuropathy of any kind, visually significant cataract, endophthalmitis, or retinal dystrophies.
Data collected included demographics, type of RVO (CRVO or BRVO), the best-corrected visual acuity (BCVA), type of anti-VEGF injection, dates of anti-VEGF injections, and clinic visits. BCVA was assessed at the first (Q1) and last (Q4) quarters of each year. Anti-VEGF injections per patient for each month were calculated as the total of injections per month divided by the total of patients.
BCVA was recorded and reported in the Snellen fraction, which was converted into logarithm of the minimal angle of resolution (log MAR) values for statistical analysis.
Statistical analysis
All data collected in the study was extracted using the MD-Clone software and was inserted into an electronic database via Microsoft Excel 2013 (Microsoft Corporation). Statistical analyses were performed using Minitab software, version 17 (Minitab Inc, State College, PA). Results were expressed as mean ± SD, median (range), or N (%). For the comparison of continuous and categorical data at the final visit versus baseline, the paired T-test and McNemar’s test were used, respectively. To compare continuous and categorical data between non-paired groups, the Student’s T and chi-square tests were used, respectively. A P-value of less than 0.05 was considered statistically significant.
Results
A total of 814 eyes of 814 patients met the inclusion criteria and were included in this study. Of them, 439 were assessed in 2019 and 375 in 2020. Patients’ baseline characteristics of before (2019) and during (2020) COVID-19 period are shown in Table 1. Forty-eight percent of the patients included in the study were females and the mean age was 72.8 years. There was no statistically significant difference between 2019 and 2020 while comparing patients’ mean age and gender (p = 0.1, 0.4, respectively).
Table 2 depicts the baseline (Q1) and final (Q4) BVCA of the patients in both 2019 and 2020. In 2019, Q1 mean BCVA of patients was 0.58 logMAR (20/76), while Q4 mean BCVA was 0.51 logMAR (20/64) (p < 0.01). In 2020, the mean baseline BCVA was 0.57 logMAR (20/74) and the mean final BCVA was 0.51 logMAR (20/64) (p < 0.01). There was no significant difference between patients in 2019 and 2020 in baseline and final BCVA (p = 0.7, p = 0.9 respectively).
Table 3 shows the deterioration of visual acuity as Snellen letters lost. As much as 79.5% of patients were stable and lost 0–5 Snellen letters in 2019 while only 72.3% in 2020 (p = 0.01). Thirty-three patients (7.5%) and 53 patients (14.1%) lost 5–10 Snellen letters in 2019 and 2020, respectively (p < 0.01). There was an insignificant difference between the patients that lost more than 10 Snellen letters before (2019) and during (2020) the COVID-19 pandemic (p = 0.79).
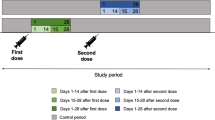
During 2020 and the pandemic period, the mean number of anti-VEGF injections per patient was 5.0, significantly reduced from the 5.9 of 2019 (p < 0.01). Figure 1 presents the trends in the ratio of anti-VEGF injections per patient, per month, as a comparison between 2019 and 2020. A significant difference is seen during most of the year, and mainly during March through May, reaching a ratio of 0.41 in 2020 vs 0.67 in 2019 (p < 0.01). Figure 2 depicts the gap with its CI (confidence intervals) between injections index of each year per month, with a corresponding significant higher gap in March, April, and May.
Table 4 shows the outcome of the multiple regression analysis with baseline BCVA, age, gender, period of injections (2019 or 2020), and the number of injections as potential predictors of final BCVA. Baseline BCVA (0.69, p < 0.01) and the number of injections (− 0.01, p = 0.01) were significant predictors of final BCVA, as opposed to age, gender, and year that were not (p = 0.07, 0.84, 0.99 respectively). Betas represent the proportion each predictor influences on final BCVA.
Table 5 demonstrates type of anti VEGF used during the follow-up period. All included patients initially treated with bevacizumab in both 2019 and 2020. Switch is subjected to retina specialist decision and is possible only if there decrease in visual acuity or worsening in OCT parameters such as increase in macular thickness. Thus, the bevacizumab group is the responsive group and the rest represent the non-responsive patients.
Discussion
On March 2020, at the beginning of the COVID-19 pandemic, the Israeli government imposed the first national lockdown as an attempt to control the rising morbidity. During that period, patients’ medical care was limited to emergency care only; elective activity was suspended, including intravitreal anti-VEGF injections [16]. A study from the USA showed that during the COVID-19 period, ophthalmology had an 81% reduction in patient volume, thus becoming one of the most impacted by the pandemic specialty. Similarly, Stone L et al. reported that 39.6% of retina patients’ appointments were delayed during the lockdown, with an even higher proportion in the RVO population achieving up to 45.6% [17]. The study from Italy noted a 53.6% reduction in intravitreal injections during COVID-19 quarantine [18]. In the current study, we aimed to investigate the impact of the postponed care of RVO patients on the number of received injections and BCVA. The data from 2019 was collected and compared with the same period of 2020. Our study showed that during 2020, the total annual number of injections administered to patients was significantly lower than in 2019, with a mean number of 5.0 and 5.9 correspondingly (p < 0.01). These results are consistent with the other reports of the pandemic period [17, 19]. The most noticeable reduction was during the first national lockdown (March to May 2020). The number of injections was found to be a significant predictor of the final BCVA in the multiple regression analysis, with a linear correlation between the number of injections and letters gained. For every annual injection administrated to a patient, approximately one letter was gained. These results correlate with previous studies that investigated the association between a number of annual intravitreal injections and final BCVA, for both CRVO-related and BRVO-related ME [20].
Indeed, in this study, the diminished medical care of patients attributed to the COVID-19 pandemic had caused the patients a certain vision loss, as higher rates of patients from 2020 lost 5–10 Snellen letters than of patients from 2019 (14.1% versus 7.5%, p < 0.01) and fewer patients maintained their vision (72.3% vs. 79.5%, p = 0.01). These results are in accordance with other studies that investigated the impact of delayed follow-up due to COVID-19 on VA of patients with RVO [17, 21, 22]. However, we found no statistical difference in BCVA outcomes between patients from 2019 to 2020, suggesting that in a large cohort, with a study period of 1 year and a reduction of 0.9 annual injections, the vision loss is not clinically significant.
After the national lockdown was over in May and the limitations were gradually removed, patients started to return to the clinics and to their original treatment regimen, reaching their original number of injections at the end of the year. Accordingly, the visual acuity of most patients improved throughout the year. The improvement we found was similar while comparing patients from 2019 to 2020, which supports that a single delay for a few months in treatment for previously treated RVO patients after their first year of treatment may not result in a significant visual loss for most patients and can be compensated by returning to the original treatment regimen.
In our multiple regression model, baseline BCVA was also found to be a predictor for final BCVA, as previously reported [23,24,25]. In their study, Kim et al. concluded that baseline BCVA is among the predictors for BCVA outcomes at 6 months, in both CRVO and BRVO patients [26]. Moreover, Koh Y et al. showed that baseline BCVA is the most important prognostic factor for visual outcome in younger patients [27].
Limitations
The retrospective nature of this study is its main limitation, as it can only suggest an association and not causation. No data regarding type of venous occlusion and OCT details was included in this study. In addition, the lack of data on the canceled medical follow-ups including ocular complications and the number of missed injections did not allow calculation of the time gaps created in patients’ treatment regimens due to the COVID-19 pandemic restrictions.
Conclusions
In this large cohort of RVO patients, during 2020 and the lockdowns imposed due to the COVID-19 pandemic, we found a significant reduction in the annual number of anti-VEGF injections administrated to patients. The postponed care did not result in a significant impact on final BCVA outcomes. Baseline BCVA and the number of annual injections may serve as predictors for final BCVA.
References
Yau JWY, Lee P, Wong TY, Best J, Jenkins A (2008) Retinal vein occlusion: an approach to diagnosis, systemic risk factors and management. Intern Med J 38:904–910
Ip M, Hendrick A (2019) Retinal vein occlusion review. Asia-Pacific Journal of Ophthalmology 7:40–45
Laouri M, Chen E, Looman M, Gallagher M (2011) The burden of disease of retinal vein occlusion: review of the literature. Eye 25:981–988
Klein R, Klein BE, Moss SE, Meuer SM (2008) The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc 98:133–141
Song P, Xu Y, Zha M, Zhang Y, Rudan I (2019) Global epidemiology of retinal vein occlusion: a systematic review and meta-analysis of prevalence, incidence, and risk factors. J Glob Health 9:010427
Bucciarelli P, Passamonti SM, Gianniello F, Artoni A, Martinelli I (2017) Thrombophilic and cardiovascular risk factors for retinal vein occlusion. Eur J Intern Med 44:44–48
Kornhauser T, Schwartz R, Goldstein M, Neudorfer M, Loewenstein A, Barak A (2016) Bevacizumab treatment of macular edema in CRVO and BRVO: long-term follow-up. (BERVOLT study: Bevacizumab for RVO long-term follow-up). Graefe’s archive for clinical and experimental ophthalmology 254:835–844
Schmidt-Erfurth U, Garcia-Arumi J, Gerendas BS et al (2019) Guidelines for the management of retinal vein occlusion by the European Society of Retina Specialists (EURETINA). Ophthalmologica 242:123–162
Grzybowski A, Markeviciute A, Zemaitiene R (2021) Treatment of macular edema in vascular retinal diseases: a 2021 update. J Clin Med 10(22):5300. https://doi.org/10.3390/jcm10225300
Sangroongruangsri S, Ratanapakorn T, Wu O, Anothaisintawee T, Chaikledkaew U (2018) Comparative efficacy of bevacizumab, ranibizumab, and aflibercept for treatment of macular edema secondary to retinal vein occlusion: a systematic review and network meta-analysis. Expert Rev Clin Pharmacol 11:903–916
Campa C, Alivernini G, Bolletta E, Parodi MB, Perri P (2016) Anti-VEGF therapy for retinal vein occlusions. Curr Drug Targets 17:328–336
Borrelli E, Sacconi R, Querques L et al (2020) Taking the right measures to control COVID-19 in ophthalmology: the experience of a tertiary eye care referral center in Italy. Eye 34:1175–1176
Bulut MN, Sönmez HS, Gökçe G et al (2021) The impact of delayed anti-vascular endothelial growth factor treatment for retinal diseases during the COVID-19 lockdown. Photodiagn Photodyn Ther 35:102449
Jaulim A, Ahmed B, Khanam T, Chatziralli IP (2013) Branch retinal vein occlusion: epidemiology, pathogenesis, risk factors, clinical features, diagnosis, and complications. An update of the literature Retina 33:901–910
Armstrong RA (2013) Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic & physiological optics: the journal of the British College of Ophthalmic Opticians (Optometrists) 33:7–14
Lim HB, Tan T-E, Fenner BJ et al (2021) Clinical operational considerations and responses to lockdown and reopening in the COVID-19 pandemic: experience of a tertiary ophthalmology centre in Singapore. Eye. https://doi.org/10.1038/s41433-021-01566-2
Stone LG, Grinton ME, Talks JS (2021) Delayed follow-up of medical retina patients due to COVID-19: impact on disease activity and visual acuity. Graefe’s Archive for Clinical and Experimental Ophthalmology 259:1773–1780
Borrelli E, Grosso D, Vella G et al (2020) Impact of COVID-19 on outpatient visits and intravitreal treatments in a referral retina unit: let’s be ready for a plausible “rebound effect.” Graefe’s Archive for Clinical and Experimental Ophthalmology 258:2655–2660
Stone LG, Devenport A, Stratton IM, Talks JS (2020) Macula service evaluation and assessing priorities for anti-VEGF treatment in the light of COVID-19. Graefe’s Archive for Clinical and Experimental Ophthalmology 258:2639–2645
Ciulla T, Pollack JS, Williams DF (2020) Visual acuity outcomes and anti-VEGF therapy intensity in macular oedema due to retinal vein occlusion: a real-world analysis of 15 613 patient eyes. Br J Ophthalmol 105:1696–1704
Song W, Singh RP, Rachitskaya A, v. (2021) The effect of delay in care among patients requiring intravitreal injections. Ophthalmology Retina 5:975–980
Naravane A, Mundae R, Zhou Y et al (2021) Short term visual and structural outcomes of anti-vascular endothelial growth factor (anti-VEGF) treatment delay during the first COVID-19 wave: a pilot study. PLoS One 16:e0247161
Damato RJ, Miller NR, Fine SL et al (1991) The effect of age and initial visual acuity on the systemic and visual prognosis of central retinal vein occlusion Prognosis of central retinal vein occlusion. Aust N Z J Ophthalmol 19:119–122
Nagasato D, Muraoka Y, Osaka R et al (2020) Factors associated with extremely poor visual outcomes in patients with central retinal vein occlusion. Sci Rep 10:19667
Scott IU, VanVeldhuisen PC, Oden NL et al (2011) Baseline predictors of visual acuity and retinal thickness outcomes in patients with retinal vein occlusion: standard care versus corticosteroid for retinal vein occlusion study report. Ophthalmology 118:345–352
Kim SJ, Yoon YH, Kim HK et al (2015) Baseline predictors of visual acuity and retinal thickness in patients with retinal vein occlusion. J Korean Med Sci 30:475–482
Koh Y-Y, Lai C-C, Wu W-C et al (2020) Baseline clinical features predict visual outcome in young patients with central retinal vein occlusion. Graefe’s Archive for Clinical and Experimental Ophthalmology 258:1367–1377
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by RS, OS, EG, OT, and SS. The first draft of the manuscript was written by RC and was reviewed and edited by AA and GR with the supervision of AL. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with animals or human participants performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cohen, R., Shor, R., Segal, O. et al. Postponed care due to COVID-19 lockdown impact on visual acuity of retinal vein occlusion patients: a large cohort. Graefes Arch Clin Exp Ophthalmol 261, 43–48 (2023). https://doi.org/10.1007/s00417-022-05755-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05755-x