Abstract
Purpose
Two-year post-operative outcomes of both deep sclerectomy (DS) and trabeculectomy surgery (Trab) augmented with Mitomycin C (MMC) at a single tertiary eye centre.
Methods
Retrospective review of DS + MMC and trabeculectomy + MMC at a single centre between February 2015 and March 2018. Patients with a minimum of 12-month follow-up were included. Post-operative follow-up: day 1, week 1, months 1/3/6/12/18/24. Primary outcomes: changes in intraocular pressure (IOP) and changes in LogMAR visual acuity (BCVA) pre- and post-procedure. Secondary outcomes: changes in number of eye drops, number of follow-up clinic visits, post-operative complications and further surgical interventions. Complete success: IOP ≤ 21 mmHg off all IOP-lowering medications. Qualified success: IOP ≤ 21 mmHg on medication. Failure: IOP > 21 mmHg at 24 months or ≤ 5 mmHg on 2 consecutive follow-up visits after 3 months +/− additional incisional glaucoma surgery +/− loss of light perception. Statistical analysis performed using Microsoft Excel + SPSS.
Results
90 eyes: DS + MMC = 46 eyes, Trab + MMC = 44 eyes. DS + MMC v Trab + MMC: mean pre-op IOP = 19.57 mmHg v 18.89 mmHg, significantly reduced at all post-operative time-points for both groups (p < 0.001). Mean IOP reduction from baseline = 33.94% v 38.39%; > 30% IOP reduction = 54.35% v 68.18%. IOP ≤ 16 mmHg = 82.61% (38/46) v 95.46% (42/44), IOP ≤ 12 mmHg = 52.17% (24/46) v 72.72% (32/44). Complete success = 67.39% v 61.36%, qualified success = 26.09% v 29.55%, failure = 6.52% v 9.09%. Post-op BCVA: no statistically significant differences between two groups (p = 0.09). Mean pre-op drops v post-op drops = 2.98 v 0.38 (DS + MMC; p < 0.001); 2.68 v 0.39 (Trab + MMC; p < 0.001). Further surgical intervention = 13% v 29.55%. Mean number of post-op clinic visits DS + MMC v Trab + MMC = 10.09 v 13.02 (p = 0.005).
Conclusion
Both procedures achieve sustained intraocular pressure and drop reduction at 2 years post-op. DS + MMC has lower complication rates requiring less intervention and significantly fewer clinic visits, which may be an important factor for deciding surgical management of glaucoma patients in the era of Covid-19 to reduce patient/clinician exposure to the virus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Glaucoma is the leading cause of irreversible blindness globally with reduction of intraocular pressure identified as a key strategy for preventing visual loss [1, 2].
UK NICE guidelines NG81 recommend surgical intervention augmented with mitomycin C (MMC) for open-angle glaucoma patients who are either advanced or at risk of progressing to sight loss whilst on two therapeutic pharmacological agents [3]. MMC is an alkylating agent that inhibits DNA replication and, when applied during filtration surgery, helps counter fibroblasts involved in the scarring process at the surgical site, thereby improving the chances of long-term surgical success [4, 5]. However, the use of MMC can be associated with wound leak, hypotony and potentially endophthalmitis [6].
Although augmented trabeculectomy is widely considered to be the gold standard surgical option for managing glaucoma, non-penetrating glaucoma surgery (NPGS) can provide comparable long-term qualified success rates with reduced post-operative complications [7]. Very few studies have compared augmented trabeculectomy with augmented NPGS, with one prospective randomised study and one retrospective longitudinal study demonstrating more favourable outcomes with trabeculectomy at 20 months and 5 years, respectively [8, 9]. A meta-analysis comparing both trabeculectomy and deep sclerectomy (DS) augmented with MMC also showed lower intraocular pressures with trabeculectomy but increased rates of complications, particularly cataract formation, compared to DS [10].
The high level of disease burden posed by glaucoma on publicly funded healthcare services has been further exacerbated by the impact of the recent Covid-19 pandemic, requiring the need to reduce face-to-face contact between clinicians and patients as well as the need to maintain social distancing in clinical areas [11, 12].
This paper explores the 2-year post-operative outcomes of both deep sclerectomy and trabeculectomy surgery augmented with MMC at a single tertiary eye centre. It also assesses the number of post-operative clinic visits required for patients in both groups, which may prove to be a helpful factor when deciding on surgical management in order to reduce the risk from Covid-19 for vulnerable patient groups.
Methods
Retrospective study of patients who underwent deep sclerectomy and trabeculectomy procedures augmented with MMC at St Paul’s Eye Unit, Liverpool (UK) over 3 years between February 2015 and March 2018. Data collection was conducted via electronic patient record searches using PENS, Medisoft and Unity software. Patients with a minimum of 12-month follow-up were included. Post-operative follow-up schedule was day 1, week 1, months 1, 3, 6, 12, 18 and 24. Primary outcomes included changes in intraocular pressure (IOP) and changes in LogMAR visual acuity (BCVA) pre- and post-procedure. Secondary outcomes focused on changes in number of eye drops, number of follow-up clinic visits, post-operative complications and surgical interventions performed post-operatively.
Success was classed as complete, qualified or failure at 2 years post-operatively. Complete success was defined as IOP ≤ 21 mmHg off all intraocular pressure-lowering medications, whereas qualified success was defined as IOP ≤ 21 mmHg on additional intraocular pressure-lowering medication. Number of eyes achieving IOP ≤ 16 mmHg and IOP ≤ 12 mmHg were also noted. Failure was classed as IOP > 21 mmHg at 24 months or ≤ 5 mmHg on 2 consecutive follow-up visits after 3 months or requiring additional incisional glaucoma surgery or loss of perception of light. Post-operative removal of releasable sutures for trabeculectomy cases and bleb manipulation (i.e. massage) were not included as procedures; however, bleb needling was counted as an intervention.
Statistical analysis was performed using Microsoft Excel (Microsoft Corp, Redmond, WA, USA) and SPSS (SPSS Inc., Chicago, IL, USA). Normality of data (age, IOP, BCVA, visual field mean deviation, length of post-operative follow-up, number of drops at each follow-up visit and number of post-operative visits) were examined using the Kolmogorov-Smirnov test. Mixed linear model analysis with Bonferroni correction was used to assess changes in IOP and BCVA at multiple post-operative time-points within each group. The Mann-Whitney U test was used to assess baseline differences in age and number of post-operative clinical visits between surgical groups. The independent T-test was used to assess the difference between lengths of post-operative follow-up between surgical groups. Fisher’s exact test and Pearson chi-squared test were used to assess differences between surgical groups for baseline categorical variables with two, and more than two groups, respectively. Wilcoxon’s matched pairs test was used to assess for differences between numbers of post-operative drops at baseline compared to the last follow-up visit. Kaplan-Meier survival analysis with Log Rank (Mantel-Cox) test was used to determine significance between the two groups. A p value < 0.05 was considered statistically significant. All study conduct adhered to the tenets of the Declaration of Helsinki.
Surgical technique for deep sclerectomy + MMC
A 7-0 vicryl corneal traction suture is placed superiorly followed by creation of a superior fornix-based conjunctival flap; haemostasis is achieved using cautery. A two-thirds thickness 5 × 5 mm limbus-based superficial scleral flap is fashioned and advanced 1 mm into clear cornea. MMC-soaked cellulose sponges are applied posteriorly under the conjunctiva and superficial scleral flaps for a set time period before being removed. Copious irrigation with balanced salt solution follows. A 4 × 4 mm deep scleral flap is created to the level of Schlemm’s canal, which is de-roofed with subsequent removal of the juxta-canalicular fibres at the trabeculo-descemet’s window (TDW). Viscoat™ (sodium hyaluronate and sodium chondroitin sulphate) is injected into the scleral bed, and the deep flap is excised close to the TDW. The superficial scleral flap and conjunctiva are closed tightly with 10-0 vicryl sutures. Subconjunctival steroids and topical antibiotics as well as atropine are instilled at the end of the procedure.
Surgical technique for trabeculectomy + MMC
A 7-0 vicryl corneal traction suture is placed superiorly followed by creation of a superior fornix-based conjunctival flap; haemostasis is achieved using cautery. A 50% thickness 4 × 4 mm limbus-based scleral flap is fashioned, ending 1 mm parallel to the corneoscleral limbus. A crescent blade is used to tunnel into clear cornea. MMC-soaked cellulose sponges are applied posteriorly under the conjunctiva and scleral flap for a set time period before being removed. Copious irrigation with balanced salt solution follows. A paracentesis is performed and the anterior chamber is entered. An ostium is fashioned with a Kelly punch, followed by a peripheral iridectomy. 2 × 10-0 nylon releasable sutures are used to close the scleral flap at the apices. The conjunctiva is closed with 10-0 nylon purse-string sutures at either end of the peritomy as well as a central mattress suture to achieve watertight closure. Subconjunctival steroids and topical antibiotics are given at the end of the procedure.
Results
A total sample size of 90 eyes of 70 patients were analysed, which included 46 eyes of 35 patients in the deep sclerectomy + MMC group and 44 eyes of 35 patients in the trabeculectomy + MMC group. Patient demographics for all variables in both groups are listed in Table 1.
Deep Sclerectomy + MMC Group
Mean length of post-operative follow-up period was 25.29 months with mean number of 10.09 post-operative clinic visits (Table 1).
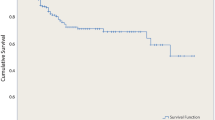
Mean post-operative IOP was significantly reduced at all time-points compared to pre-op (p < 0.001; Fig. 1 and Table 2). Mean reduction of IOP from baseline was 33.94% with 54.35% of eyes achieving > 30% reduction. Thirty-eight of 46 eyes (82.61%) achieved an IOP ≤ 16 mmHg, and 24 of 46 eyes (52.17%) achieved an IOP ≤ 12 mmHg. (Fig. 1 and Table 2)
Except for day 1 post-op (VA = 0.64; p < 0.001) and week 1 (0.35; p = 0.02), there was no significant difference with mean post-operative LogMAR BCVA at all other time-points, which at 24-months = 0.24. 6 cases (13.04%) lost the equivalent of > 2 Snellen lines of VA, however, no cases lost perception of light (Table 2).
Mean number of drops was significantly reduced post-operatively = 0.38 (p < 0.001, Wilcoxon signed rank test) with 73.91% (34 eyes) off all drops (Table 4).
Thirteen eyes (28.26%) had intraoperative perforation of the trabeculo-Descemet’s window, requiring intraoperative surgical iridectomy. Post-operatively 13.04% (6 eyes) had wound leak with two-thirds (4 eyes) being managed with a bandage contact lens and one-third (2 eyes) requiring revision of the scleral flap. Five eyes (10.87%) experienced raised IOP requiring intervention: 2 eyes were managed with laser—× 1 YAG goniopuncture (YAG GP) and × 1 selective laser trabeculoplasty (SLT)—1 eye required revision of scleral flap, 1 eye managed with removal of suture and 1 eye went on to have a CyPass stent (Alcon, Fort Worth, Texas, USA) 20 months post-op. Hence, a total of 13% (6/46 eyes) required post-operative surgical intervention (flap revision, YAG GP, SLT, CyPass). Although incidence of post-operative hypotony was 10.87% (5 eyes) across various time-points, only 2.17% (1 eye) had chronic hypotony with IOP ≤ 5 mmHg at last follow-up. One of 16 phakic eyes (6.25%) required cataract surgery within 24 months (Table 3).
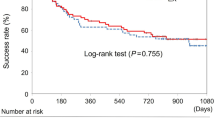
At 24 months post-op, 67.39% were classed as complete success, 26.09% qualified success and 6.52% failure (3 eyes: × 1 IOP > 21 mmHg, × 1 CyPass stent insertion and 1 IOP ≤ 5 mmHg) (Fig. 2 and Table 4).
Trabeculectomy + MMC group
Mean length of post-operative follow-up period was 28.25 months with mean number of 13.02 post-operative clinical visits (Table 1).
Mean post-operative IOP was significantly reduced at all time-points compared to pre-op (p < 0.0001; Fig. 1 and Table 2). Mean reduction of IOP from baseline was 38.39% with 68.18% of eyes achieving > 30% reduction. Forty-two of 44 eyes (95.46%) achieved an IOP ≤ 16 mmHg, and 32 of 44 eyes (72.72%) achieved an IOP ≤ 12 mmHg (Table 2).
LogMAR BCVA was significantly reduced post-operatively at day 1 = 0.52 (p < 0.0001), week 1 = 0.41 (p = 0.001), month 1 = 0.35 (p = 0.016) and month 3 = 0.35(p = 0.021). At all other time-points, there was no significant difference, which at 24 months = 0.25 (p = 0.476). Four cases (10%) lost the equivalent of > 2 Snellen lines of VA; however, no cases lost perception of light.
Mean number of drops was significantly reduced post-operatively = 0.39 (p < 0.001, Wilcoxon signed rank test) with 70.46% (31 eyes) off all drops (Table 4).
Intraoperative complications were limited to haemorrhage requiring AC washout (2.27%; 1 eye) and vitreous to ostium site requiring intraoperative localised anterior vitrectomy (2.27%; 1 eye).
Nineteen eyes (43%) experienced post-operative complications including conjunctival leak in 11.36% (5 eyes) managed initially with BCL but 3 eyes eventually requiring surgical management (bleb revision). Another 13.64% (6 eyes) displayed IOP spikes ranging from 29 to 46 mmHg between day 1 and 6 months post-op; 9.09% demonstrated inflammatory reactions (× 1 iritis, × 1 CMO, × 1 ERM and × 1 cyclitic membrane formation). Three eyes (6.82%) experienced infection (× 1 endophthalmitis, × 1 TASS and × 1 orbital cellulitis), and 4.55% (2 eyes) had post-operative hyphaema. One eye displayed iris obstructing the ostium, which then underwent YAG laser 1 week post-op (Table 3).
Thirteen eyes (29.55%) required further surgery including 11.36% undergoing needling (5 eyes), 11.36% having bleb revision, 4.55% needing conjunctival re-suturing (2 eyes) and 2.27% (1 eye) requiring insertion of a Baerveldt tube 22 months post-op. Incidence of hypotony was 11.36% (5 eyes) with 6.82% (3 eyes) displaying chronic hypotony with IOP ≤ 5 mmHg at last follow-up. Twelve of 30 phakic eyes (40%) required cataract surgery within 24 months.
At 24 months post-op, 61.36% were classed as complete success, 29.55% qualified success and 9.09% failure (4 eyes—× 3 IOP ≤ 5 mmHg and × 1 Baerveldt tube insertion) (Fig. 2 and Table 4).
Inter-group comparison: deep sclerectomy + MMC v trabeculectomy + MMC
There was no statistically significant difference for severity of glaucoma between the two groups, pre-operative VF MD = − 12.73 dB v − 13.35 dB (p = 0.72). There was no statistically significant difference between the two groups for number of pre-operative (2.98 v 2.68; p = 0.2) and post-operative eye drops (0.38 v 0.39; p = 0.9). Although both groups achieved statistically significant lower IOPs across all post-operative time-points, there was no statistically significant difference between the two groups for IOP. Similarly, there was no statistically significant difference for post-operative LogMAR BCVA between the two groups (p = 0.09). For success, there was no statistical difference found between the DS-MMC group v trabeculectomy-MMC group for cumulative survival rates (93.48% v 90.91%) or between complete survival rates (p = 0.481) or qualified survival rates (p = 0.67). However, there was a statistically significant difference between the two groups for number of post-operative clinical visits: 10.09 v 13.02 (p = 0.005).
Discussion
Very few studies have compared augmented DS with augmented trabeculectomy. One prospective randomised study compared augmented viscocanalostomy with augmented trabeculectomy, with more favourable outcomes for IOP and eye drop reduction noted for the latter group, whereas another paper performed a retrospective study comparing augmented DS with augmented trabeculectomy, but their primary outcome measures focused on bleb morphology [8, 13]. However, the numbers used in both these studies were small (total of 50 eyes and 28 eyes, respectively) and with a short follow-up period (20 months and 3 months, respectively). This current study provides a comparison between the two augmented groups with a larger sample size and longer follow-up period. This paper also differs from the other studies by noting differences in the number of post-operative visits between the two groups whilst also assessing IOP < 16 and IOP < 12 mmHg.
Demographics (Table 1)
Although the DS cohort was older with a higher proportion of males, both groups (DS + MMC v trabeculectomy + MMC) had similar pre-operative characteristics with regard to mean IOP (19.59 v 18.89 mmHg), mean BCVA (0.22 v 0.20), mean number of drops (2.98 v 2.68) and glaucoma severity (− 12.73 v − 13.35 dB) with no statistical difference found. Both groups had a similar number of pseudophakic eyes at baseline (30.77% v 29.55%) and a similar incidence of previous glaucoma filtration surgery (10.87 v 13.64%). Whilst the majority of cases in both groups were secondary to POAG and NTG, the trabeculectomy group had twice as many uveitic glaucoma cases (4.35% v 9.09%) and more pigmentary glaucoma cases (0% v 9.09%) as well as a higher rate of pre-existing ocular co-morbidities (39.14% v 47.73%). The DS group had a greater number of cases combined with phacoemulsification compared to the trabeculectomy group (28.26% v 2.27%) (Table 1)
Intraoperatively, consultants performed a significantly lower number of cases in the DS group than in the trabeculectomy group (50% v 72%; p = 0.043). Other differences included the DS group having a higher MMC concentration (0.05%; 78.26% v 63.64%) applied for a longer time (3 min; 71.74% v 65.91%).
Intraocular pressure (Fig. 1 and Table 2)
Post-operatively, both groups achieved statistically significant IOP reductions across all time-points (p < 0.0001) with no statistical significance found between the two groups (p = 0.88). The trabeculectomy group achieved a greater IOP reduction from baseline (33.94% v 38.39%) with a higher proportion of cases having > 30% IOP reduction (54% v 68.18%). More cases in the trabeculectomy group achieved an IOP ≤ 16 mmHg (82.61% v 95.46%) and an IOP ≤ 12 mmHg (52.17% v 72.72%) compared to the DS group. For the trabeculectomy group, these low IOP values are better than other studies focusing on outcomes of augmented trabeculectomy for advanced glaucoma [14]. For the DS group, the proportion of patients achieving these low IOP values are comparable to other studies assessing non-penetrating glaucoma surgery augmented (NPGS) with MMC [15, 16].
Visual acuity (Table 2)
Mean LogMAR BCVA was significantly reduced in the trabeculectomy group across the first 3 months, but there was no significant difference between pre- and post-operative BCVA at 24 months (0.20 v 0.25; p = 0.4). There was no significant difference in pre-and post-operative BCVA for the DS group across all time-points, and there was no statistically significant difference found at 24 months between the two groups (0.24 v 0.25; p = 0.59). Although similar numbers lost > 2 Snellen lines of VA in both groups (13.04% v 10%), no cases lost perception of light. Our trabeculectomy rate of 10% for losing > 2 Snellen lines is lower than the 27% reported by King & Stead 2011, but our DS rate was higher compared to other similar studies for augmented NPGS [14,15,16].
Eye drops
Both groups achieved statistically significant reductions in the number of eye drops pre-and post-surgery, but no significant difference was found between the two groups. The DS group had a slightly higher number of cases that were off all drops at 24 months (73.91% v 70.46%) (Table 4).
Post-operative follow-up
There was a similar post-operative mean follow-up period of time for both groups, but the trabeculectomy group required significantly more post-operative clinical visits (10.09 v 13.02; p = 0.005). This is in keeping with the results found in a nationwide survey of glaucoma specialists in the UK where by 6 months, trabeculectomy patients required a greater number of post-operative follow-up visits compared to patients who underwent deep sclerectomy (9 v 5 visits) [17]. This is a particularly important factor to consider when evaluating availability of clinical resources, improving clinical efficiency in public healthcare systems and reducing the risk of virus exposure during Covid-19.
Complications and further surgery (Table 3)
Intraoperative complications in the DS group were limited to inadvertent perforation of the trabeculo-Descemet’s membrane (28.26%). This is known to be a common complication in the early learning phase of DS but becomes less frequent with increased surgical experience [18]. Hence, the high rate of perforation may be attributable to the fact that nearly half of all DS cases were performed by non-consultant grade and nearly half of the perforations occurred in cases performed by a Fellow (46.15%). However, overall both perforation and non-perforation groups had similar post-operative mean IOPs at 24 months (13.5 mmHg v 13.3 mmHg), similar reduction of IOPs from baseline (35.54% v 33.30%) with a similar number of post-operative eye drops (0.46 v 0.36). The perforation group had worse overall success outcomes (84.62% v 96.97%) and twice as many failures (2 eyes v 1 eye).
When comparing non-perforated DS + MMC eyes (n = 33) v trab + MMC eyes (n = 44), the results reflect the overall findings with both groups displaying significant IOP reductions sustained over all post-operative time-points. However, the trab + MMC group achieves a lower mean IOP reduction from baseline (38.39% v 33.30%) and have a greater proportion of eyes with IOP ≤ 16 mmHg (95.46% v 84.85%) as well as IOP ≤ 12mmHg (72.72% v 51.52%). Both groups have similar BCVA findings post-operatively with a similar number losing > 2 Snellen lines (4 in each group). A significant reduction in mean number of drops was noted between the non-perforated DS + MMC (− 2.55; p < 0.0001) and trab + MMC groups (− 2.29; p < 0.0001) with a similar number of eyes being off all drops at their last visit (70.56% v 72.73%). The non-perforated DS + MMC group experienced greater cumulative success (90.91% v 96.97%) with a lower failure rate (9.09% v 3.03%) and lower incidences of complications compared to the trab + MMC group. The difference in mean number of post-operative clinic visits was again lower in the non-perforated DS + MMC group (13.02 v 10.15).
Intraoperative complications for the trabeculectomy + MMC group included hyphaema requiring anterior chamber washout in 2.27% of cases (1 eye), which was lower than the 8% incidence noted in the Collaborative Initial Glaucoma Treatment Study (CIGTS) [19]. One case had vitreous prolapse at the ostium requiring a localised anterior vitrectomy to be performed. This rare complication of vitreous prolapse during trabeculectomy (< 0.5%) is more likely to occur in eyes with previous trauma, thin sclera, high myopia, lens dislocation, aphakia, pseudoexfoliation (PXF) or other connective tissue disorders [20]. The case in our study was a pseudophakic female with POAG but no other ocular co-morbidities and underwent a re-do trabeculectomy at the same site. The mechanism for vitreous prolapse in this case may possibly be the result of direct trauma to the zonules during ostium creation.
In the trab + MMC group, there were a total of 5 re-do/revisions compared to a total of 4 re-do/revisions in the DS+MMC group. The majority of these in the trab + MMC group were same site operations (4/5) compared to only 1 case in the DS + MMC group. Although both groups achieved a similar IOP reduction from baseline (trab + MMC = 48.3% v DS + MMC = 40.3%), the trab + MMC group had a better success rate (80% v 50%) and failure rate (20% v 25%) compared to the DS + MMC group.
Post-operatively, both DS-MMC and trabeculectomy-MMC groups displayed similar incidences of conjunctival leak (13.04% v 11.36%) with 2 eyes and 3 eyes requiring surgical revision, respectively. These incidences of conjunctival leak are very similar to those reported in other studies looking at augmented deep sclerectomy (13.46%) and augmented trabeculectomy (13.1%) [16, 21]. In our sample, nearly all cases with post-operative conjunctival leaks in both groups received 0.05% concentration of MMC applied for 3 min. Hence, this higher concentration of MMC may have possibly been a contributing factor, which has previously been reported in other studies [22]. Although the incidence of post-operative hypotony was similar across various time-points between the two groups, 10.87% (5 eyes) v 11.36% (5 eyes), only 2.17% (1 eye) in the DS cohort had chronic hypotony with IOP ≤ 5 mmHg at last follow-up compared with 6.82% (3 eyes) in the trabeculectomy cohort, which is lower than 7.86% reported in a large retrospective study evaluating efficacy and safety of trabeculectomy surgery in the UK [23]. Wound leaks post-augmented trabeculectomy, particularly with thin-walled blebs, can lead to bleb-related ocular infections with reported incidence in the literature of endophthalmitis ranging from 2 to 7.5% [24]. The single endophthalmitis case (2.27%) in our trabeculectomy-MMC group was a 53-year-old male uveitic glaucoma patient with no previous history of ocular surgery and had only received 0.025% MMC concentration applied for 3 min during surgery. He was hypotonous for 1 month before undergoing bleb revision and developed endophthalmitis 5 days post-revision. He was treated with intravitreal antibiotics and made a good recovery with a final VA of 0.2 LogMAR and IOP of 10 mmHg on two IOP-lowering agents.
Similar incidences of IOP rise were also noted (10.87% v 13.64%) with cases in the DS-MMC group being managed with laser (YAG goniopuncture + SLT) and 2 eyes requiring surgical intervention (DS revision + CyPass stent insertion) compared to the trabeculectomy-MMC group where 3 cases required needling, 2 requiring revision (one of these had YAG laser to iris plugging the ostium first) and 1 required a Baerveldt tube insertion. Our post-DS-MMC YAG Goniopuncture rate of 2.17% was much lower than the 13–73% reported in other studies [13, 15]. Overall, 5 eyes (11.36%) in the trabeculectomy-MMC group required bleb needling, which is less than the rate of 16–20% reported by two large retrospective studies [23, 25]. The study by O’Brart et al. 2004 noted a 23% post-operative needling rate for their NPGS cases compared to no cases in our DS-MMC group [8]. A reason for this difference may be explained our use of dissolvable vicryl sutures for scleral flap closure compared to nylon sutures being used in the other study, which allow the bleb to continue to form as the sutures dissolve, thus reducing the need for further interventions and clinical visits.
Data from the Advanced Glaucoma Intervention Study (AGIS) showed a 78% risk of developing cataract post-trabeculectomy, with the use of anti-fibrotics not deemed to be a statistically significant factor [26]. Other studies indicate that approximately 50% of patients will require cataract surgery within the first 5 years of trabeculectomy with MMC [27]. For augmented deep sclerectomy, one recent retrospective study reported an incidence of 11.6% for cataract extraction at 3 years [28]. Our study showed 6.25% of phakic patients (1/16 eyes) required cataract surgery within 24 months in the DS-MMC group versus 40% (12/30 eyes) in the trabeculectomy-MMC group. These findings are similar to the results of a meta-analysis focusing on 3 European studies comparing augmented trabeculectomy with augmented DS [10]. Although this was not an outcome that we were primarily investigating, we found this to be an interesting observation when analysing the results and feel it can be of benefit to surgeons deciding on whether to perform combined surgery.
Success (Fig. 2 and Table 4)
At 24 months, the overall cumulative success (complete + qualified) for DS-MMC group was slightly higher than for the trabeculectomy-MMC group (93.48% v 90.91%), though this was not statistically significant (Fig. 2 and Table 4). The trabeculectomy-MMC group also had a slightly higher failure rate (6.52% v 9.09%). Compared to landmark studies such the TVT trial where complete success (IOP < 21 mmHg without medication) was 33% for trabeculectomy at 3 years, our cohort achieved a higher complete success rate (61.36%) and lower failure rate (9.09% v 30.7%) [29]. Our sample also had a similar complete success rate (67.39%) compared to other studies (69–74%) for eyes undergoing deep sclerectomy augmented with MMC [30, 31].
Conclusion
This study demonstrates the effectiveness of both deep sclerectomy and trabeculectomy surgery augmented with MMC in achieving sustained post-operative intraocular pressure reduction over 2 years. Although greater intraocular pressure reduction was achieved with augmented trabeculectomy, patients undergoing augmented deep sclerectomy had a higher success rate for IOP reduction off all medication at 2 years with less severe complications. The deep sclerectomy cohort also required significantly fewer number of post-operative clinic visits compared to those undergoing augmented trabeculectomy and required fewer post-operative interventions in the clinic setting. This is particularly important when considering how to manage glaucoma during the Covid-19 pandemic. Deep sclerectomy cases can also be combined with phacoemulsification without compromising outcomes.
Limitations
The ideal design for a truly comparative study would be a randomised controlled trial. Since this was a retrospective study, we were unable to ensure identical conditions for all our patients and had differences between the demographics/disease characteristics of both groups. With our best efforts, we have tried to report the outcomes for both procedures performed in the same time period. Using statistical tests, we tried to ascertain whether there were any obviously statistically significant differences between the two groups and recorded this in Table 1 (the main statistically significant difference identified being the grade of surgeon). However, the pre-existing clinical differences between the groups do introduce the risk of bias. The numbers of patients at each time-point across the study reduced for both groups compared to the starting total due to patients no longer being alive, not receiving their follow-up on the precise time-point or being lost to follow-up +/− still awaiting an appointment (exacerbated by Covid-related delays in some cases). However, both groups have similar numbers across all time-points.
References
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY (2014) Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 121(11):2081–2090
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, Early Manifest Glaucoma Trial Group (2002) Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma Trial. Arch Ophthalmol. Oct 120(10):1268–1279
National Institute for Health and Care Excellence (2017) Glaucoma: diagnosis and management (NICE Guideline NG81). Available at https://www.nice.org.uk/guidance/ng81. Accessed 15th October 2020.
Khaw PT, Sherwood MB, MacKay SL, Rossi MJ, Schultz G (1992) Five- minute treatments with fluorouracil, floxuridine, and mitomycin have long-term effects on human Tenon's capsule fibroblasts. Arch Ophthalmol 110(8):1150–1154
Wilkins M, Indar A, Wormald R (2005) Intra-operative mitomycin C for glaucoma surgery. Cochrane Database Syst Rev 19(4):CD002897
Singh K, Egbert PR, Byrd S, Budenz DL, Williams AS, Decker JH, Dadzie P (1997) Trabeculectomy with intraoperative 5-fluorouracil vs mitomycin C. Am J Ophthalmol 123(1):48–53
Choudhary A, Wishart PK (2007) Non-penetrating glaucoma surgery augmented with mitomycin C or 5-fluorouracil in eyes at high risk of failure of filtration surgery: long term results. Clin Exp Ophthalmol 35(4):340–347
O’Brart DP, Shiew M, Edmunds B (2004) A randomised, prospective study comparing trabeculectomy with viscocanalostomy with adjunctive antimetabolite usage for the management of open angle glaucoma uncontrolled by medical therapy. Br J Ophthalmol 88(8):1012–1017
Jiang L, Eaves S, Dhillon N, Ranjit P (2018) Postoperative outcomes following trabeculectomy and nonpenetrating surgical procedures: a 5-year longitudinal study. Clin Ophthalmol 12:995–1002
Rulli E, Biagioli E, Riva I, Gambirasio G, De Simone I, Floriani I, Quaranta L (2013) Efficacy and safety of trabeculectomy vs nonpenetrating surgical procedures: a systematic review and meta-analysis. JAMA Ophthalmol 131(12):1573–1582
Husain R, Zhang X, Aung T (2020) Challenges and lessons for managing glaucoma during Covid-19 Pandemic: perspectives from Asia. Ophthalmology. (May 29). https://doi.org/10.1016/j.ophtha.2020.05.042
Jayaram H, Strouthidis N, Gazzard G (2020) The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye (Lond) (May 13). https://doi.org/10.1038/s41433-020-0958-1
Oh LJ, Wong E, Lam J, Clement CI (2017) Comparison of bleb morphology between trabeculectomy and deep sclerectomy using a clinical grading scale and anterior segment optical coherence tomography. Clin Exp Ophthalmol 45(7):701–707
Stead RE, King AJ (2011) Outcome of trabeculectomy with mitomycin C in patients with advanced glaucoma. Br J Ophthalmol 95(7):960–965
Tsagkataki M, Bampouras TM, Choudhary A (2018) Outomes of viscocanalostomy and phaco-viscocanalostomy in patients with advanced glaucoma. Graefes Arch Clin Exp Ophthalmol 256(8):1481–1487
Anand N, Atherley C (2005) Deep sclerectomy augmented with mitomycin. Eye (Lond) 19(4):442–450
Rodriguez-Una I, Azuara-Blanco A, King AJ (2017) Survey of glaucoma surgical preferences and post-operative care in the United Kingdom. Clin Exp Ophthalmol 45(3):232–240
Shaarawy T, Karlen M, Schnyder C, Achache F, Sanchez E, Mermoud A (2001) Five-year results of deep sclerectomy with collagen implant. J Cataract Refract Surg 27:1770–1778
Jampel HD, Musch DC, Gillespie BW, Lichter PR, Wright MM, Guire KE (2005) Collaborative Initial Glaucoma Treatment Study Group. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS). Am J Ophthalmol 140:16–22
Bansal RK, Casper DS, Tsai JC (2015) Intraoperative complications of trabeculectomy. Glaucoma:797–804
Anand N, Arora S, Clowes M (2006) Mitomycin C augmented glaucoma surgery: evolution of filtering bleb avascularity, transconjunctival oozing, and leaks. Br J Ophthalmol 90(2):175–180
Sanders SP, Cantor LB, Dobler AA, Hoop JS (1999) Mitomycin C in higher risk trabeculectomy: a prospective comparison of 0.2-0.4-mg.cc doses. J Glaucoma Jun 8(3):193–198
Kirwan JF, Lockwood AJ, Shah P, Macleod A, Broadway DC, King AJ, AI MN, Agrawal P, Trabeculectomy Outcomes Group Audit Study Group (2013) Trabeculectomy in the 21st century: a multicentre analysis. Ophthalmology 120(12):2532–2539
DeBry PW, Perkins TW, Heatley G, Kaufman P, Brumback LC (2002) Incidence of late-onset bleb related complications following trabeculectomy mitomycin. Arch Ophthalmol 120:297–300
Greenfield DS, Miller MP, Suner IJ, Palmberg PF (1996) Needle elevation of the scleral flap for failing filtration blebs after trabeculectomy with mitomycin C. Am J Ophthalmol 122(2):195–204
The AGIS Investigators (2001) The advanced glaucoma intervention study, 8: risk of cataract formation after trabeculectomy. Arch Ophthalmol 119(12):1771–1779
Palanca-Capistrano AM, Hall J, Cantor LB et al (2009) Long-term outcomes of intraoperative mitomycin C in primary trabeculectomy surgery. Ophthalmology. 116:175–184
Mercieca K, Perumal D, Darcy K, Anand N (2019) Cataract extraction after deep sclerectomy and its effect on intraocular pressure control. Eye (Lond) 33(4):557–563
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL (2009) Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 148:670–684
Anand N, Wechsler D (2012) Deep sclerectomy with mitomycin C in eyes with failed glaucoma surgery and pseudophakia. Eye (Lond) 26(1):70–79
Mercieca K, Steeples L, Anand N (2017) Deep sclerectomy for uveitic glaucoma: long-term outcomes. Eye (Lond). Jul 31(7):1008–1019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This was a retrospective study. For this type of study, formal consent is not required.
Conflict of interest
None of the authors have any competing or financial interests in this work. All authors have contributed significantly and are in agreement with the content of the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of a topical collection on Perspectives on COVID-19.
Rights and permissions
About this article
Cite this article
Dwivedi, R., Somerville, T., Cheeseman, R. et al. Deep sclerectomy and trabeculectomy augmented with Mitomycin C: 2-year post-operative outcomes. Graefes Arch Clin Exp Ophthalmol 259, 1965–1974 (2021). https://doi.org/10.1007/s00417-021-05144-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05144-w