Abstract
Purpose
To analyze the distribution of diabetic retinopathy (DR) lesions in an Indian population using ultra-wide field (UWF) fundus imaging.
Methods
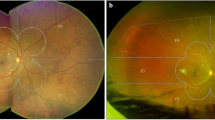
Seven hundred fifteen subjects (1406 eyes) with diabetic retinopathy in India were enrolled in this multicenter, prospective, observational study using UWF pseudocolor imaging with Optos Daytona Plus (Optos plc, Dunfermline, Scotland, UK). Images were transmitted to Doheny Image Reading Center, Los Angeles, CA, for grading. The ETDRS grid was overlaid on stereographic projections of UWF images, and images were graded independently by 2 masked graders. Lesion distribution was graded as predominantly central (PCL) or predominantly peripheral (PPL) according to previous criteria, considering both lesion number and area. An image was graded as PPL if > 50% of the lesion area was seen in at least one peripheral field as compared with the corresponding ETDRS field. Diabetic retinopathy severity was also assessed based on the International Classification of Diabetic Retinopathy (ICDR) grading scale. The main outcome measures were lesion distribution (PPL versus PCL): overall and within specific fields in eyes with various grades of DR.
Results
Lesion distribution was rated to be PPL in 37% of eyes and PCL in 63% of eyes (P < 0.003). The frequency of a PPL distribution varied significantly across all ICDR severity levels, with frequencies of mild non-proliferative DR (NPDR) (30.9%), moderate NPDR (40.3%), severe NPDR (38.5%) and PDR (34.9%), P = 0.005. When assessing which individual fields were rated to show a PPL distribution, the frequency was greatest in field 4 and least in field 7. For any grade of DR, temporal fields showed the greatest PPL frequency, followed in order by the superior, inferior, and nasal fields (P < 0.001). Only 3.5% of eyes showed PPL distribution in all five peripheral fields.
Conclusions
One-third of the UWF images showed a PPL distribution in this cohort with the temporal quadrant having the widest distribution of PPL. As the PPL distribution varied significantly between various grades of DR, UWF imaging may prove to be important for screening of referral warranted retinopathy.




Similar content being viewed by others
References
Early Treatment Diabetic Retinopathy Study Research Group (1991) Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification: ETDRS report number 10. Ophthalmology. 98(suppl):786–806
Early Treatment Diabetic Retinopathy Study Research Group (1991) Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology. 98:823–833
Ghasemi Falavarjani K, Tsui I, Sadda SR (2017) Ultra-wide-field imaging in diabetic retinopathy. Vis Res 139:187–190
Byberg S, Vistisen D, Diaz L, Charles MH, Hajari JN, Valerius M, Juul E, Jørgensen ME, Lund-Andersen H (2019) Optos wide-field imaging versus conventional camera imaging in Danish patients with type 2 diabetes. Acta Ophthalmol 97:815–820
Schwartz SD, Gupta A, Gonzales CR, et al (2005) Peripheral retinal ischemia associated with diffuse diabetic macular edema identified with widefield angiography. Invest Ophthalmol Vis Sci. 46:ARVO E-Abstract 4793
Diabetic Retinopathy Clinical Research Network. (2017) Peripheral diabetic retinopathy (DR) lesions on ultrawide-field fundus images and risk of DR worsening over time. Peripheral_DR_lesions_and_Risk_of_DR_ProgressionV4_0_7_21_17.pdf. Accessed on 12 Dec 2018
Pomerantzeff O (1975) Equator-plus camera. Investig Ophthalmol 14:401–406
Oishi A, Hidaka J, Yoshimura N (2014) Quantification of the image obtained with a wide field scanning ophthalmoscope. Invest Ophthalmol Vis Sci 55:2424–2431
Wessel MM, Aaker GD, Parlitsis G, Cho M, D'Amico DJ, Kiss S (2012) Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 32:785–791
Tan CS, Chew MC, van Hemert J, Singer MA, Bell D, Sadda SR (2015) Measuring the precise area of peripheral retinal non-perfusion using ultra-widefield imaging and its correlation with the ischaemic index. Br J Ophthalmol 100:235–239
Silva PS, Cavallerano JD, Sun JK, Soliman AZ, Aiello LM, Aiello LP (2013) Peripheral lesions identified by mydriatic ultrawide field imaging: distribution and potential impact on diabetic retinopathy severity. Ophthalmology 120:2587–2595
Silva PS, Cavallerano JD, Tolls D et al (2014) Potential efficiency benefits of nonmydriatic ultrawide field retinal imaging in an ocular telehealth diabetic retinopathy program. Diabetes Care 37:50–55
Price LD, Au S, Chong NV (2015) Optomap ultrawide field imaging identifies additional retinal abnormalities in patients with diabetic retinopathy. Clin Ophthalmol 9:527–531
Aiello LP, Odia I, Glassman AR et al (2019) Diabetic Retinopathy Clinical Research Network. Comparison of Early Treatment Diabetic Retinopathy Study standard 7-field imaging with ultrawide-field imaging for determining severity of diabetic retinopathy. JAMA Ophthalmol 137:65–73
Manjunath V, Papastavrou V, Steel DH et al (2015) Wide-field imaging and OCT vs clinical evaluation of patients referred from diabetic retinopathy screening. Eye (Lond) 29:416–423
Silva PS, El-Rami H, Barham R et al (2017) Hemorrhage and/or microaneurysm severity and count in ultrawide field images and EarlyTreatment Diabetic Retinopathy Study photography. Ophthalmology. 124:970–976
Klein R, Meuer SM, Moss SE, Klein BE (1995) Retinal microaneurysm counts and 10-year progression of diabetic retinopathy. Arch Ophthalmol 113:1386–1391
Kohner EM, Sleightholm M (1986) Does microaneurysm count reflect severity of early diabetic retinopathy? Ophthalmology. 93:586–589
Silva PS, Cavallerano JD, Haddad NM et al (2015) Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 122:949–956
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
Resnikoff S, Felch W, Gauthier TM, Spivey B (2012) The number of ophthalmologists in practice and training worldwide: a growing gap despite more than 200,000 practitioners. Br J Ophthalmol 96:783–787
Cheloni R, Gandolfi SA, Signorelli C, Odone A (2019) Global prevalence of diabetic retinopathy: protocol for a systematic review and meta-analysis. BMJ Open 9:e022188
Pandey SK, Sharma V (2018) World diabetes day 2018: battling the emerging epidemic of diabetic retinopathy. Indian J Ophthalmol 66:1652–1653
Alswailmi FK (2018) Global prevalence and causes of visual impairment with special reference to the general population of Saudi Arabia. Pak J Med Sci 34:751–756
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, Chen S-J, Dekker JM, Fletcher A, Grauslund J, Haffner S, Hamman RF, Kamran Ikram M, Kayama T, Klein BEK, Klein R, Krishnaiah S, Mayurasakorn K, O’Hare JP, Orchard TJ, Porta M, Rema M, Roy MS, Sharma T, Shaw J, Taylor H, Tielsch JM, Varma R, Wang JJ, Wang N, West S, Xu L, Yasuda M, Zhang X, Mitchell P, Wong TY, for the Meta-Analysis for Eye Disease (META-EYE) Study Group (2012) Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35:556–564
Gadkari SS, Maskati QB, Nayak BK (2016) Prevalence of diabetic retinopathy in India: the all India ophthalmological society diabetic retinopathy eye screening study 2014. Indian J Ophthalmol 64:38–44
West SK, Klein R, Rodriguez J, Muñoz B, Broman AT, Sanchez R, Snyder R, Proyecto VER (2001) Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care 24:1204–1209
Knickelbein JE, Hasan J, Nussenblatt RB, Sen HN (2016) Delineation of choroidal and retinal lesions in posterior uveitis by multispectral wide-field scanning laser ophthalmoscopy. Retina. 36:2213–2219
Escudero-Sanz I, Navarro R (1999) Off-axis aberrations of a wide-angle schematic eye model. J Opt Soc Am A Opt Image Sci Vis 16:1881–1891
Global Diabetic Retinopathy Project Group, Wilkinson CP, Ferris FL 3rd, Klein RE et al (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 110:1677–1682
Diabetic Retinopathy Clinical Research Network, Elman MJ, Aiello LP, Beck RW et al (2010) Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 117:1064–1077
Nguyen QD, Brown DM, Marcus DM, et al; RISE and RIDE Research Group (2012) Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 119:789–801
Wessel MM, Nair N, Aaker GD, Ehrlich JR, D'Amico DJ, Kiss S (2012) Peripheral retinal ischaemia, as evaluated by ultra-widefield fluorescein angiography, is associated with diabetic macular oedema. Br J Ophthalmol 96:694–698
Kim DY, Kim J-G, Kim YJ, Joe SG, Lee JY (2014) Ultra-widefield fluorescein angiographic findings in patients with recurrent vitreous hemorrhage after diabetic vitrectomy. Invest Ophthalmol Vis Sci 55:7040–7046
Patel RD, Messner LV, Teitelbaum B, Michel KA, Hariprasad SM (2013) Characterization of ischemic index using ultra-widefield fluorescein angiography in patients with focal and diffuse recalcitrant diabetic macular edema. Am J Ophthalmol 155:1038–1044
Silva PS, Cavallerano JD, Tolson AM et al (2015) Real-time ultrawide field image evaluation of retinopathy in a diabetes telemedicine program. Diabetes Care 38:1643–1649
Acknowledgments
The following are members of IRRA Study group: Kim Ramasamy, Jano van Hemert, Yadav NK, Rajeev R Pappuru, Adnan Tufail, Muneesawar Gupta, SriniVas R. Sadda, and Rajiv Raman.
Financial information
AV: none; ARA: none; KR: None; JvH: Optos (E); YNK: none; RRP: none; AT: Allergan, Heidelberg Engineering, Bayer, Novartis, Oxurion, Roche.; MNG: none; SRS: Allergan (C, F), Carl Zeiss Meditec (C,F), Centervue (C), Genentech (C, F), Heidelberg Engineering (C), Iconic (C), NightstarX (C), Novartis (C), Optos (C,F), Oxurion(C), Topcon (C); RR: none.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Aditya Verma and Ahmed Roshdy Alagorie are co-first authors.
This manuscript has not been published/presented in any journal/conference.
Rights and permissions
About this article
Cite this article
Verma, A., Alagorie, A.R., Ramasamy, K. et al. Distribution of peripheral lesions identified by mydriatic ultra-wide field fundus imaging in diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol 258, 725–733 (2020). https://doi.org/10.1007/s00417-020-04607-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04607-w