Abstract
Purpose
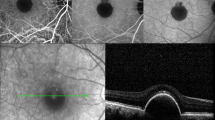
To investigate the outcomes of embedding lamellar hole-associated epiretinal proliferation (LHEP) into retinal cleavage for the surgical treatment of degenerative lamellar macular hole (LMH).
Methods
We retrospectively reviewed the medical records of 34 consecutive eyes of degenerative LMH patients who underwent vitrectomy with LHEP embedding and who were followed up for at least 12 months. Best-corrected visual acuity (BCVA), central retinal thickness (CRT), and macular structure preoperatively and at the final follow-up were compared.
Results
The mean (±SD) follow-up period was 30.0 ± 17.7 months. Twelve patients (35.3%) were men, and the mean age was 69.6 ± 10.1 years. Twenty-three eyes (67.6%) underwent simultaneous cataract surgery. BCVA was significantly improved at the final visit, from 0.31 ± 0.25 logarithm of the minimum angle of resolution units to 0.10 ± 0.25 (P < 0.01). This improvement in mean BCVA at the final postoperative visit occurred regardless of whether the eyes underwent simultaneous cataract surgery, from 0.30 ± 0.26 preoperatively to 0.04 ± 0.16 (P < 0.01) in the “with cataract surgery” group and from 0.32 ± 0.26 preoperatively to 0.21 ± 0.35 (P < 0.05) in the “without cataract surgery” group. CRT was also significantly improved at the final visit, from 123.2 ± 42.6 μm preoperatively to 191.2 ± 42.6 μm (P < 0.01). External limiting membrane and ellipsoid zone defects were detected in 17 (50.0%) and 15 (44.1%) eyes, respectively, but these were resolved in 10 (58.8%) and 7 (46.7%) eyes, respectively, at the final visit. No intraoperative or postoperative complications were observed.
Conclusions
Embedding LHEP may be an effective and safe procedure to treat degenerative LMH.





Similar content being viewed by others
References
Gass JD (1975) Lamellar macular hole: a complication of cystoid macular edema after cataract extraction: a clinicopathologic case report. Trans Am Ophthalmol Soc 73:231–250. https://doi.org/10.1001/archopht.1976.03910030391008
Duker JS, Kaiser PK, Binder S et al (2013) The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 120:2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Witkin AJ, Ko TH, Fujimoto JG et al (2006) Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology 113:388–397. https://doi.org/10.1016/j.ophtha.2005.10.047
Lai TT, Chen SN, Yang CM (2016) Epiretinal proliferation in lamellar macular holes and full-thickness macular holes: clinical and surgical findings. Graefes Arch Clin Exp Ophthalmol 254:629–638. https://doi.org/10.1007/s00417-015-3133-9
Dell'omo R, Virgili G, Rizzo S et al (2017) Role of lamellar hole-associated epiretinal proliferation in lamellar macular holes. Am J Ophthalmol 175:16–29. https://doi.org/10.1016/j.ajo.2016.11.007
Govetto A, Dacquay Y, Farajzadeh M et al (2016) Lamellar macular hole: two distinct clinical entities? Am J Ophthalmol 164:99–109. https://doi.org/10.1016/j.ajo.2016.02.008
Zampedri E, Romanelli F, Semeraro F et al (2017) Spectral-domain optical coherence tomography findings in idiopathic lamellar macular hole. Graefes Arch Clin Exp Ophthalmol 255:699–707. https://doi.org/10.1007/s00417-016-3545-1
Frisina R, Zampedri E, Marchesoni I et al (2016) Lamellar macular hole in high myopic eyes with posterior staphyloma: morphological and functional characteristics. Graefes Arch Clin Exp Ophthalmol 254:2141–2150. https://doi.org/10.1007/s00417-016-3371-5
Lai TT, Yang CM (2018) Lamellar hole-associated epiretinal proliferation in lamellar macular hole and full-thickness macular hole in high myopia. Retina 38:1316–1323. https://doi.org/10.1097/IAE.0000000000001708
Gaudric A, Aloulou Y, Tadayoni R, Massin P (2013) Macular pseudoholes with lamellar cleavage of their edge remain pseudoholes. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2012.10.021
Hirano M, Morizane Y, Kimura S et al (2018) Assessment of lamellar macular hole and macular pseudohole with a combination of en face and radial B-scan optical coherence tomography imaging. Am J Ophthalmol 188:29–40. https://doi.org/10.1016/j.ajo.2018.01.016
Purtskhvanidze K, Balken L, Hamann T et al (2018) Long-term follow-up of lamellar macular holes and pseudoholes over at least 5 years. Graefes Arch Clin Exp Ophthalmol 256:1067–1078. https://doi.org/10.1007/s00417-018-3972-2
Figueroa MS, Govetto A, Steel DH et al (2018) Pars plana vitrectomy for the treatment of tractional and degenerative lamellar macula holes: functional and anatomical results. Retina. https://doi.org/10.1097/IAE.0000000000002326
Choi WS, Merlau DJ, Chang S (2018) Vitrectomy for macular disorders associated with lamellar macular hole epiretinal proliferation. Retina 38:664–669. https://doi.org/10.1097/IAE.0000000000001591
Ko J, Kim GA, Lee SC et al (2016) Surgical outcomes of lamellar macular holes with and without lamellar hole-associated epiretinal proliferation. Acta Ophthalmol 95:e221. https://doi.org/10.1111/aos.13245
Parolini B, Schumann RG, Cereda MG et al (2011) Lamellar macular hole: a clinicopathologic correlation of surgically excised epiretinal membranes. Invest Ophthalmol Vis Sci 52:9074–9083. https://doi.org/10.1167/iovs.11-8227
Itoh Y, Levison AL, Kaiser PK et al (2015) Prevalence and characteristics of hyporeflective preretinal tissue in vitreomacular interface disorders. Br J Ophthalmol 100:399–404. https://doi.org/10.1136/bjophthalmol-2015-306986
Shiraga F, Takasu I, Fukuda K et al (2013) Modified vitreous surgery for symptomatic lamellar macular hole with epiretinal membrane containing macular pigment. Retina 33:1263–1269. https://doi.org/10.1097/IAE.0b013e31828bcb61
Shiode Y, Morizane Y, Takahashi K et al (2018) Embedding of lamellar hole-associated epiretinal proliferation combined with internal limiting membrane inversion for the treatment of lamellar macular hole: a case report. BMC Ophthalmol 18:257. https://doi.org/10.1186/s12886-018-0926-8
Schumann RG, Compera D, Schaumberger MM et al (2015) Epiretinal membrane characteristics correlate with photoreceptor layer defects in lamellar macular holes and macular pseudoholes. Retina 35:727–735. https://doi.org/10.1097/IAE.0000000000000375
Michalewska Z, Michalewski J, Odrobina D et al (2010) Surgical treatment of lamellar macular holes. Graefes Arch Clin Exp Ophthalmol 248:1395–1400. https://doi.org/10.1007/s00417-010-1400-3
Pang CE, Spaide RF, Freund KB (2014) Epiretinal proliferation seen in association with lamellar macular holes: a distinct clinical entity. Retina 34:1513–1523. https://doi.org/10.1097/IAE.0000000000000163
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J (2010) Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 117:2018–2025. https://doi.org/10.1016/j.ophtha.2010.02.011
Shiode Y, Morizane Y, Matoba R et al (2017) The role of inverted internal limiting membrane flap in macular hole closure. Invest Ophthalmol Vis Sci 58:4847–4855. https://doi.org/10.1167/iovs.17-21756
Tadayoni R, Paques M, Massin P et al (2001) Dissociated optic nerve fiber layer appearance of the fundus after idiopathic epiretinal membrane removal. Ophthalmology 108:2279–2283
Alkabes M, Salinas C, Vitale L et al (2011) En face optical coherence tomography of inner retinal defects after internal limiting membrane peeling for idiopathic macular hole. Invest Ophthalmol Vis Sci 52:8349–8355. https://doi.org/10.1167/iovs.11-8043
Michels RG (1982) A clinical and histopathologic study of epiretinal membranes affecting the macula and removed by vitreous surgery. Trans Am Ophthalmol Soc 80:580–656
Guidry C, Bradley KM, King JL (2003) Tractional force generation by human müller cells: growth factor responsiveness and integrin receptor involvement. Invest Ophthalmol Vis Sci 44:1355–1363. https://doi.org/10.1167/iovs.02-0046
Qiao H, Hisatomi T, Sonoda KH et al (2005) The characterisation of hyalocytes: the origin, phenotype, and turnover. Br J Ophthalmol 89:513–517. https://doi.org/10.1136/bjo.2004.050658
Kohno RI, Hata Y, Kawahara S et al (2009) Possible contribution of hyalocytes to idiopathic epiretinal membrane formation and its contraction. Br J Ophthalmol 93:1020–1026. https://doi.org/10.1136/bjo.2008.155069
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethics committees of Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Kurashiki Medical Center, Takasu Eye Clinic, and Inoue Eye Clinic and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Online Resource 1
.mp4 After core vitrectomy, lamellar hole-associated epiretinal proliferation (LHEP) was centripetally peeled from the retina using microforceps but was left attached to the edge of the LMH. Next, brilliant blue-assisted ILM peeling was performed around the LMH in a circumferential manner. The LHEP was gently massaged centripetally over the LMH so that the LHEP was embedded into the retinal cleavage of the LMH. If the area of the LHEP was larger than that of the LMH, the LHEP was trimmed to fit the size of the retinal cleavage. Fluid-air exchange was performed at the end of surgery (MOV 316729 kb)
Rights and permissions
About this article
Cite this article
Takahashi, K., Morizane, Y., Kimura, S. et al. Results of lamellar macular hole-associated epiretinal proliferation embedding technique for the treatment of degenerative lamellar macular hole. Graefes Arch Clin Exp Ophthalmol 257, 2147–2154 (2019). https://doi.org/10.1007/s00417-019-04425-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04425-9