Abstract
Purpose
The aim of this study was to use the Ocular Trauma Score (OTS) to review and analyze all the open globe injuries (OGIs) that presented to Brooke Army Medical Center (BAMC) from July 2011 to March 2017, and whether or not the OTS can be used to predict enucleation or evisceration.
Methods
Retrospective chart review was performed through the medical record systems at BAMC for all OGIs from July 2011 to March 2017. This study was not performed on wartime patients. The primary outcome measures were the variables in the OTS and need for enucleation or evisceration.
Results
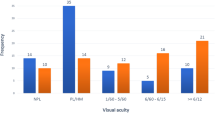
A total of 126 OGIs in 125 patients were identified from July 2011 to March of 2017. A lower calculated OTS was negatively associated with the outcome variables. A total of 25 cases resulted in enucleation or evisceration (19.8%). Of these, 17 underwent enucleation and 8 underwent evisceration. The average OTS for all eyes was 37.15, and the average OTS for eyes resulting in enucleation or evisceration was 22. Retinal detachment (RD), afferent pupillary defect (APD), globe rupture, globe perforation, and presenting visual acuity (VA) were all found to be statistically significant risk factors in patients who underwent enucleation or evisceration.
Conclusions
The present study shows that the OTS and the OTS pre-operative variables can help predict the likelihood that an OGI will ultimately result in enucleation or evisceration. Our study shows that the OTS is a valuable tool to use when evaluating OGI and can help in evidence-based counseling.

Similar content being viewed by others
References
Page RD, Gupta S, Jenkins T, Karcioglu Z (2016) Risk factors for poor outcomes in patients with open-globe injuries. Clin Ophthalmol 10:1461–1466
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD (2002) The ocular trauma score (OTS). Ophthalmol Clin N Am 15(2):163–165
Bauza A, Emami P, Soni N et al (2013) A 10-year review of assault-related open-globe injuries at an urban hospital. Graefes Arch Clin Exp Ophthalmol 251:653–659
Savar A, Andreoli MT, Koek CE, Andreoli CM (2009) Enucleation for open globe injury. Am J Ophthalmol 147(4):595–600
Knyazer B, Bilenko N, Levy J et al (2013) Open globe eye injury characteristics and prognostic factors in southern Israel: a retrospective epidemiologic review of 10 years experience. Isr Med Assoc J 15(3):158–156
Thack AB, Johnson AJ, Carroll RB et al (2008) Severe eye injuries in the war in Iraq. 2003-2005. Ophthalmology. 115(2):377–382
Cillino S, Casuccio A, Di Pace F, Pillitteri F, Cillino G (2008) A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol. https://doi.org/10.1186/1471-2415-8-6
Schmidt GW, Broman AT, Hindman HB, Grant MP (2008) Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 115(1):202–209
Agrawal R, Ho SW, Teoh S (2013) Pre-operative variables affecting final visual outcome with a critical review of ocular trauma classification for posterior open globe (zone III) injury. Indian J Ophthalmol 61(10):541–545
Agrawal R, Wei HS, Teoh S (2012) Predictive factors for final outcome of severely traumatized eyes with no light perception. BMC Ophthalmol. https://doi.org/10.1186/1471-2415-12-16
Andreoli MT, Andreoli CM (2012) Surgical rehabilitation of the open globe injury patient. Am J Ophthalmol 153(5):856–860
McAlinden C, Saldanha M, Laws D.(2013) Evisceration for management of ocular trauma. BMJ Case Rep ; 2013: bcr 2013201235
Ababneh OH, AboTaleb EA, Abu Ameerh MA, Yousef YA (2015) Enucleation and evisceration at a tertiary care hospital in a developing country. BMC Ophthalmol 15:120
Plestina-Borjan I, Medvidovic-Grubisic M, Zuljan I et al (2010) Wartime open globe eye injuries. Graefes Arch Clin Exp Ophthalmol 248(3):305–312
Zheng C, Wu AY (2013) Enucleation versus evisceration in ocular trauma: a retrospective review and study of current literature. Orbit. 32(6):356–361
Yousef SJ, Jones LS, Kidwell ED (2012) Enucleation and evisceration: 20 years of experience. Orbit. 31(4):211–215
Toit ND, Mustak H, Cook C (2015) Visual outcomes in patients with open globe injuries compared to predicted outcomes using the Ocular Trauma Scoring system. Int J Ophthalmol 8(6):1229–1233
Acknowledgments
Kurt Edwards, COL, USA, MD
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the office of the Institutional Review Board (IRB), Department of Clinical Investigations at BAMC, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
The study was granted a waiver of informed consent by the IRB board at BAMC as it involved no more than minimal risk to the individuals and their privacy. The data is Health Insurance Portability and Accountability Act (HIPAA) compliant. Demographic and clinical data from the initial examination, surgical charts, and follow-up visits were recorded in a de-identified database.
Disclaimer
The authors report no financial disclosures. The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of the Brooke Army Medical Center, the US Army Medical Department, the US Army Office of the Surgeon General, the Department of the Air Force, the Department of the Army or the Department of Defense, or the US Government.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: Military Health System Research Symposium August 2017, Kissimmee Fl (poster), Excelsior Surgical Society October 2017, San Diego, CA (oral presentation)
Rights and permissions
About this article
Cite this article
Brundridge, W., Reed, D., Santamaria, J. et al. Open globe trauma in a military hospital: a review of the Ocular Trauma Score to help predict enucleation or evisceration. Graefes Arch Clin Exp Ophthalmol 257, 1789–1793 (2019). https://doi.org/10.1007/s00417-019-04356-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04356-5