Abstract
Purpose
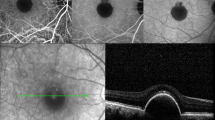
Our purpose was to determine the effectiveness of vitrectomy in resolving the macular retinoschisis in an eye with glaucomatous optic neuropathy and also to determine the natural course of macular retinoschisis.
Methods
This was a retrospective case series of patients who were diagnosed with macular retinoschisis and glaucomatous optic neuropathy. Fourteen eyes of 13 patients were studied. Patients with high myopia, vitreomacular traction syndrome, and the pit macular syndrome were excluded.
Results
There were three men and ten women, and 12 had unilateral and one had bilateral macular retinoschisis. Vitrectomy was performed for a serous retinal detachment, macular hole, or severe visual loss in five eyes. The mean follow-up time was 68.8 months in these five eyes, and the macular retinoschisis was resolved and the best-corrected visual acuity (BCVA) at the final visit was significantly improved in all eyes (P = 0.007). However, two of these fiv e eyes developed a macular hole and required a second vitrectomy. Of the nine eyes without treatment with a mean follow-up time of 29.0 months, the BCVA at the final visit remained unchanged from the baseline BCVA in all eyes. The macular retinoschisis was resolved or reduced in three eyes without treatment.
Conclusions
Vitrectomy was effective for the resolution of macular retinoschisis in eyes with glaucomatous optic neuropathy and serous retinal detachment or macular hole or severe reduction of the BCVA. Macular retinoschisis can be resolved without a reduction of the BCVA in some cases without treatment.



Similar content being viewed by others
References
Sobol WM, Blodi CF, Folk JC et al (1990) Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology 97:1539–1542
Takano M, Kishi S (1999) Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 128:472–476
Gaucher D, Haouchine B, Tadayoni R et al (2007) Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 143:455–462
Fujimoto M, Hangai M, Suda K et al (2010) Features associated with foveal retinal detachment in myopic macular retinoschisis. Am J Ophthalmol 150:863–870
Yoshikawa T, Nishimura T, Minamino K et al (2013) A long-term follow-up of peripapillary retinoschisis with optic disc hypoplasia. Int Ophthalmol 33:425–428
Hotta K, Hotta J (2004) Retinoschisis with macular retinal detachment associated with vitreomacular traction syndrome. Retina 24:307–309
Yamada N, Kishi S (2005) Tomographic features and surgical outcomes of vitreomacular traction syndrome. Am J Ophthalmol 139:112–117
Duker JS, Kaiser PK, Binder S et al (2013) The international Vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619
Inoue M, Itoh Y, Rii T et al (2015) Macular retinoschisis associated with glaucomatous optic neuropathy in eyes with normal intraocular pressure. Graefes Arch Clin Exp Ophthalmol 253:1447–1456
Takashina S, Saito W, Noda K et al (2013) Membrane tissue on the optic disc may cause macular schisis associated with a glaucomatous optic disc without optic disc pits. Clin Ophthalmol 7:883–887
Zhao M, Li X (2011) Macular retinoschisis associated with normal tension glaucoma. Graefes Arch Clin Exp Ophthalmol 249:1255–1258
Farjad H, Besada E, Frauens BJ (2010) Peripapillary schisis with serous detachment in advanced glaucoma. Optom Vis Sci 87:205–217
Mavrikakis E, Lam WC (2011) Macular schisis and detachment secondary to large optic nerve head cup: a newly recognized syndrome amenable to vitrectomy. Acta Ophthalmol 89:95–96
Hollander DA, Barricks ME, Duncan JL et al (2005) Macular schisis detachment associated with angle-closure glaucoma. Arch Ophthalmol 123:270–272
Lee EJ, Kim TW, Kim M et al (2014) Peripapillary retinoschisis in glaucomatous eyes. PLoS One 9:e90129
Bayraktar S, Cebeci Z, Kabaalioglu M et al (2016) Peripapillary Retinoschisis in glaucoma patients. J Ophthalmol 2016:1612720
van der Schoot J, Vermeer KA, Lemij HG (2017) Transient Peripapillary Retinoschisis in glaucomatous eyes. J Ophthalmol 2017:1536030
Hwang YH, Kim YY, Kim HK et al (2014) Effect of peripapillary retinoschisis on retinal nerve fibre layer thickness measurement in glaucomatous eyes. Br J Ophthalmol 98:669–674
Zumbro DS, Jampol LM, Folk JC et al (2007) Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol 144:70–74
Krivoy D, Gentile R, Liebmann JM et al (1996) Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol 114:165–170
Katome T, Mitamura Y, Hotta F et al (2013) Swept-source optical coherence tomography identifies connection between vitreous cavity and retrobulbar subarachnoid space in patient with optic disc pit. Eye 27:1325–1326
Taiel-Sartral M, Mimoun G, Glacet-Bernard A et al (1996) Vitrectomy-laser-gas for treating optic disk pits complicated by serous macular detachment. J Fr Ophtalmol 19:603–609
García-Arumí J, Guraya BC, Espax AB et al (2004) Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefes Arch Clin Exp Ophthalmol 242:819–826
Rayat JS, Rudnisky CJ, Waite C et al (2015) Long-term outcomes for optic disc pit maculopathy after vitrectomy. Retina 35:2011–2017
Acknowledgments
The authors thank Professor Yoshinori Mitamura, Dr. Yoshifumi Okamoto, and Dr. Eiichi Yukawa for helpful advice and data collection, and Professor Emeritus Duco Hamasaki of the Bascom Palmer Eye Institute for discussions and manuscript revision. All members became a part of Japan Clinical Retina Study (J-CREST) group and researched.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Yoshikawa, T., Yamanaka, C., Kinoshita, T. et al. Macular retinoschisis in eyes with glaucomatous optic neuropathy: Vitrectomy and natural course. Graefes Arch Clin Exp Ophthalmol 256, 281–288 (2018). https://doi.org/10.1007/s00417-017-3855-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3855-y