Abstract
Background
Deep anterior lamellar keratoplasty (DALK) has a much lower incidence of immunologic reactions than penetrating keratoplasty (PK) for patients with keratoconus. However, it is unclear whether DALK is better on refractive outcomes than PK, due to its high postoperative myopia.
Methods
We retrospectively studied the clinical records of keratoconus patients who underwent PK, DALK, or predescemetic DALK (pre-DALK, DALK with residual stroma) between June 2004 and September 2008. The main outcome measures included refractive sphere, manifest cylinder, corneal power, keratometric astigmatism, and best-corrected visual acuity (BCVA) at the latest visit and the methods of visual correction. Postoperative manifest refractions and topography data were compared at postoperative 3, 5, 7, and 9 years among the three groups. Additionally, the final BCVA and the methods of vision correction were compared.
Results
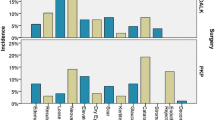
A total of 172 subjects (172 eyes) screened out of 207 keratoconus patients underwent PK (79 eyes), DALK (68 eyes), or pre-DALK (25 eyes). Postoperative myopic refractive sphere increased in all groups, but the most obvious increase was noted in the pre-DALK group. At the 9-year follow-up, both the pre-DALK group (−6.5 ± 1.7 D) and DALK group (−6.1 ± 1.8 D) had higher myopic refractive sphere than the PK group (−5.0 ± 1.5 D, p < 0.05). Postoperative myopic manifest astigmatism progressively increased in 5 years, but there were no differences among the groups. The progressive increases in postoperative corneal power were recorded in all groups, with the highest one in the pre-DALK group and the lowest in the PK group. At the 9-year follow-up, both the pre-DALK (49.8 ± 2.7 D) and DALK (48.8 ± 2.1 D) groups had higher corneal power than the PK group (47.3 ± 2.0 D); meanwhile, the corneal power was higher in the pre-DALK group than the DALK group (p < 0.05). No differences were noted with respect to keratometric astigmatism among the groups. Mean LogMAR BCVA was 0.12 ± 0.12 in the DALK group, 0.17 ± 0.10 in the pre-DALK group, and 0.1 ± 0.11 in the PK group (p = 0.325) at 9 years after surgery. Moreover, the methods of achieving BCVA seem to be similar among the treatment groups.
Conclusions
Although DALK has a slightly higher degree of myopic refraction than PK, DALK and PK have comparable visual acuity outcomes and similar methods of vision correction. DALK is recommended for the treatment of keratoconus.
Similar content being viewed by others
References
Zadnik K, Barr JT, Edrington TB et al (1998) Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci 39:2537–6
Pramanik S, Musch DC, Sutphin JE et al (2006) Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology 113:1633–1638
Bahar I, Kaiserman I, Srinivasan S et al (2008) Comparison of three different techniques of corneal trabsplantation for keratoconus. Am J Ophthalmol 146:905–912
Jaycock PD, Jones MN, Males J et al (2008) Outcomes of same-sizing versus oversizing donor trephines in keratoconic patients undergoing first penetrating keratoplasty. Ophthalmology 115:268–275
Javadi MA, Feizi S, Yazdani S et al (2010) Deep anterior lamellar keratoplasty versus penetrating keratoplasty for keratoconus: a clinical trial. Cornea 29:365–371
Fontana L, Parente G, Tassinari G (2007) Clinical outcomes after deep anterior lamellar keratoplasty using the big-bubble technique in patients with keratoconus. Am J Ophthalmol 143:117–124
Feizi S, Javadi M, Kanavi MR (2012) Recurrent keratoconus in a corneal graft after deep anterior lamellar keratoplasty. J Ophthalmol Vis Res 7:328–331
Kim KH, Choi SH, Ahn K et al (2011) Comparison of refractive changes after deep anterior lamellar keratoplasty and penetrating keratoplasty for keratoconus. Jpn J Ophthalmol 55:93–97
Watson SL, Ramsay A, Dart JK et al (2004) Comparison of deep lamellar keratoplasty and penetrating keratoplasty in patients with keratoconus. Ophthalmology 111:1676–1682
Huang T, Zhang X, Wang Y et al (2012) Outcomes of deep anterior lamellar keratoplasty using the big-bubble technique in various corneal diseases. Am J Ophthalmol 154:282–289
Vail A, Gore SM, Bradley BA et al (1996) Clinical and surgical factors infliencing corneal graft survival, visual acuity, and astigmatism. Corneal transplant follow-up study collaborators. Ophthalmology 103:41–49
Busin M, Mönks T, al-Nawaiseh I (1998) Different suturing techniques variously affect the regularity of postkeratoplasty astigmatism. Ophthalmology 105:1200–1205
Kagaya F, Tomidokoro A, Tanaka S et al (2002) Fourier series harmonic analysis of corneal topography following suture removal after penetrating keratoplasty. Cornea 21:256–259
Javadi MA, Feizi S, Rastegarpour A (2011) Effect of vitreous length and trephine size disparity on post-DALK refractive status. Cornea 30:419–423
Skeens HM, Holland EJ (2010) Large-diameter penetrating keratoplasty: indications and outcomes. Cornea 29:296–301
Patal SV, Malta JB, Banitt MR et al (2009) Recurrent ectasia in corneal grafts and outcomes of repeat keratoplasty for keratoconus. Br J Ophthalmol 93:191–197
de Toledo JA, de la Paz MF, Barraquer RI, Barraquer J (2003) Long-term progression of astigmatism after penetrating keratoplasty for keratoconus: evidence of late recurrence. Cornea 22:317–323
Han DC, Mehta JS, Por YM et al (2009) Comparison of outcomes of lamellar keratoplasty and penetrating keratoplasty in keratoconus. Am J Ophthalmol 148:744–751
Cheng YY, Visser N, Schouten JS et al (2011) Endothelial cell loss and visual outcome of deep anterior lamellar keratoplasty versus penetrating keratoplasty: a randomized multicenter clinical trial. Ophthalmology 118:302–309
Bourges JL, Savoldelli, Dighiero P et al (2003) Recurrence of keratoconus characteristics: a clinical and histologic follow-up analysis of donor grafts. Ophthalmology 110:1920–1925
Szczotka-Flynn L, McMahon TT, Lass JH et al (2004) Late-stage progressive corneal astigmatism after penetrating keratoplasty for keratoconus. Eye Contact Lens 30:105–110
Kremer I, Eagle RC, Rapuano CJ, Laibson PR (1995) Histologic evidence of recurrent keratoconus seven years after keratoplasty. Am J Ophthalmol 119:511–512
Bechrakis N, Blom ML, Stark WJ, Green WR (1994) Recurrent keratoconus. Cornea 13:73–77
Abelson MB, Collin HB, Gillette TE, Dohlman CH (1980) Recurrent keratoconus after keratoplasty. Am J Ophthalmol 90:672–676
Edwards M, Mcghee CN, Dean S (2001) The genetics of keratoconus. Clin Exp Ophthalmol 29:345–351
Acknowledgement
Publication of this article was supported by the Natural Science Foundation of China (NO.81371065). The roles of funding organization included data collection and analysis. None of the authors have any financial interests to disclose. Involved in design and conduct of the study (T.H.); collection (T.H., Y.H., M.G., C.H., H.Z.); management (T.H.); analysis (T.H., Y.H.); interpretation of the data (T.H., M.G., C.H.); preparation of the manuscript (T.H., Y.H., C.H.); review (T.H., Y.H., H.Z.); and approval of the manuscript (T.H., Y.H., M.G., C.H., H.Z.). The corresponding author Ting Huang has full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. The study protocol was approved by the Ethics Committee of Zhongshan Ophthalmic Center (Guangzhou, China) and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Conflict of interest
The authors declare that they have no competing interests.
Financial support
Natural Science Foundation of China (NO.81371065)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, T., Hu, Y., Gui, M. et al. Comparison of refractive outcomes in three corneal transplantation techniques for keratoconus. Graefes Arch Clin Exp Ophthalmol 253, 1947–1953 (2015). https://doi.org/10.1007/s00417-015-3091-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3091-2