Abstract
Valproate is the most effective medication for generalised epilepsies, and several specific epilepsy syndromes. For some people, it will be the only medication to establish seizure remission, and withdrawing it carries risks of seizure recurrence and Sudden Unexpected Death in Epilepsy (SUDEP). It is also of proven efficacy for bipolar disorder and migraine prevention. Guidelines based on observational and epidemiological studies stress that maternal valproate related teratogenicity and neurodevelopmental effects are significantly higher than for other antiseizure medications (ASMs). It should, therefore, only be used if other medications are ineffective and after balancing the teratogenicity risk. Regulatory restrictions have changed prescribing practices and reduced valproate use. The number of other medications that must be trialled in the different conditions for which valproate has effectiveness and the consequences of the lack of efficacy of those drugs leading to significant harm including death remains unexplored. Risk minimisation measures (RMMs) for valproate, chiefly Pregnancy Prevention practices (PPP), consider foetal risk and not risk to people living with epilepsy. In the United Kingdom (UK), limitations relating to valproate use in all people < 55 years commenced in January 2024. While the evidence in child-bearing women is not disputed, the data in males are based on animal models, case reports, and one commissioned, unpublished, non-peer reviewed report unavailable to the UK public, stakeholder charities or professionals. Evidence suggests that 30–40% of people switching from valproate have breakthrough seizures. Thus, an estimated 21,000–28000 people in the UK will imminently be exposed to the potential hazards of breakthrough seizures, including death. There is little government investment in monitoring the effects of these changes to valproate prescribing on patient health and quality of life. This review summarises the history of valproate regulation, evidence underpinning it and argues how the latest regulations in the UK do not align with the country’s medical regulatory bodies ethical principles nor with the Montgomery principles of informed patient choice and autonomy. It dissects how such regulations infringe Common Law principles, nor give due regard for patient outcomes beyond reproduction. The paper looks to provide recommendations to redress these concerns while appreciating the core need for such governance to emerge in the first place.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This review summarises the history of valproate (sodium valproate) regulation related to adult epilepsy, indications, risks and benefits of valproate for epilepsy. Evidence is graded A–E [1]. The ethical and legal problems with the current Medicines and Healthcare Products Regulatory Agency (MHRA) regulations are discussed, along with circumstances where patients or their representatives may choose valproate. Recommendations are made to re-align focus on the care of people wanting to take valproate after informed consent, and the monitoring of those patients avoiding it.
History of regulation
Advocacy groups maintain that the government, pharmaceutical industry, and clinical responses have been inadequate and too slow, to valproate (VPA) teratogenicity reported in animals since the 1970s and in humans since the 1980s [2]. Since the 1990s, the consensus hardened that the teratogenic effects of VPA were greater than for other older and newer alternatives ASMs (including lamotrigine and later levetiracetam) [3]. Since 2014, valproate has not been recommended for use in the UK for girls and women of childbearing potential unless other treatments are ineffective or not tolerated. It is no longer listed as the first-choice treatment for women with genetic generalised epilepsies, despite its superior efficacy to all other ASMs [4]. Risk minimisation measures (RMMs) to reduce teratogenicity and/or developmental disorders mandated the Pregnancy Prevention Programme (PPP): that is “user independent” contraception (intrauterine devices or subdermal progesterone only implant) for women taking valproate [5]. This created a gender divide in prescribing practice based on guidelines and increasing statutory restrictions [6]. In England, the number of pregnant women prescribed valproate in a 6-month period fell from 68 women in April to September 2018, to 17 women in October 2021 to March 2022 [7]. The MHRA projects a 11% risk of birth defects and a 30–40% risk of neuro-developmental disabilities [7], but there are no published data on the outcomes of these pregnancies, where dose-adjustment and other mitigations may have been effective. In a recent study, approximately 11% of women with epilepsy self-reported being on valproate [8]. Concerns exist about the blanket nature of including all women of childbearing age with epilepsy [6, 9,10,11,12], and for those who lack the ability to have an informed consensual relationship especially those with intellectual disability [9, 10, 12]. It was recognised that the situation is complex especially regarding people with intellectual disability and UK practices were out of kilter with other parts [9,10,11,12,13].
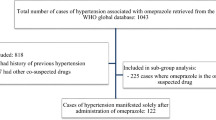
In November 2023, the MHRA announced new RMMs bringing restrictions to all people under the age of 55 years [14]. As shown in Box 1, the emergence of the mechanisms and operational programme for these new measures are unclear. Some of the critical source data for this extension have not been shared with health professionals despite multiple requests to the MHRA, including two Freedom of Information requests from amalgamated epilepsy charities [15]. The MHRA appears to have implemented changes based on a report that was not suitably peer-reviewed and published. The MHRA recorded that “errors have been identified in the study that may impact on the results” requiring further analysis [15]. This leaves professionals and charities in the UK with the impossible task of supporting people with epilepsy in informed decision-making without the information [13, 15].
VPA indications
VPA is licensed to treat all forms of epilepsy [27]. It also has FDA indications for bipolar disorder (including acute mania and mixed episodes) and migraine prevention [28]. Outside licence, it is used occasionally to treat various pain syndromes, although evidence of its benefit in these contexts is lacking [29]. Potential adjuvant therapy roles in conditions such as HIV and cancer, and in neuroprotection (stroke and neurodegenerative diseases), possibly through histone deacetylase inhibition, are under exploration [27].
It became clear from post-licencing clinical experience and comparative randomised-controlled studies published during the 1980s and 1990s that VPA offered clinically significant advantages in seizure control compared with other medications for patients with generalised tonic–clonic seizures (GTCS), which are the hallmark of many of the genetic (idiopathic) generalised epilepsies [30]. A randomised multicentre trial showed that valproate was the most effective medication for generalised epilepsies [31]. Until recently, range of academic and professional guidelines, including NICE, recommended valproate as “first-choice” treatment for this group [32]. Valproate is also considered effective for a number of paediatric epilepsy syndromes, such as Dravet’s syndrome [33].
Sexual health, reproduction and valproate
Studying sexual health is challenging given the lack of standardisation of definitions and outcome measures, and the wide variability that exists across age, cultures and socioeconomic settings [34]. Chronic conditions, including epilepsy, can affect sexual function and fertility in many ways. For people with epilepsy, many inter-related factors can contribute to sexual dysfunction [35]. Those with comorbidities (particularly Intellectual Disability (ID) and psychiatric problems) more severe epilepsy, certain seizure types, and those who are socially deprived are more likely to have difficulties [34]. Fertility levels are reported as lower for people with epilepsy in small, detailed surveys [36] and large population studies [37]. Nevertheless, evidence suggests no direct relationship between sex hormone levels and sexual happiness, with high levels of sexual satisfaction occurring in some people with abnormal hormonal profiles [34, 35]. Men in relationships who have epilepsy report the same level of sexual satisfaction as those in relationships without epilepsy [34, 35].
Valproate may indirectly increase sexual happiness through seizure freedom, which is the main determinant of quality of life in epilepsy and through mood stabilising effects [34]. Indirect negative effects of valproate on sexual function include weight gain [38], insulin resistance with associated increased risk of hypogonadism in males [38], and polycystic ovarian syndrome in women. [38, 39].
Women
Female sexual dysfunction increases with age and worldwide is reported as 41% [40]. ASMs, including VPA, epilepsy, chronic illness all have reported associations with sexual dysfunction, as do socioeconomic deprivation (which correlates with severity of epilepsy), stress and psychiatric illness [34, 41]. The focus of sexual health research in epilepsy has been on reproduction.
There are no current, or planned, randomised controlled trials of ASM use in pregnancy. Observational data derived from population studies, pregnancy registers, and case–control studies in people with epilepsy are the principal evidence for all guidance on this subject. Cochrane reviews conclude that methodological flaws do not affect the assertions of the risks of valproate [42]. A pooled analysis reported major congenital malformations (defined as an abnormality of an essential anatomical structure that substantially interferes with function or requires major intervention) [3] in 6.1% (range 4–10%) [43] of children whose mothers took ASMs during pregnancy, compared with 2.8% in children of untreated women with epilepsy and 2.2% in the general population [44]. Registries [44,45,46,47,48] report rates of major malformations for valproate ranging from 6.7% in the UK and Ireland Epilepsy and pregnancy registers which includes a third of relevant pregnancies [45], 10–13.8% in the Australian Pregnancy Registry, which includes 1 in 12 relevant pregnancies [47]. There are few prospective reports for indications other than epilepsy. The Australian registry captured nine children of women who were taking valproate for indications other than epilepsy, one of whom had a malformation (cleft palate) [49]. Some major malformations (hypospadias, cleft palate, polydactyly, cardiac defects) are treatable, but many leave children dependent, with serious lifelong disability.
Maternal valproate is also associated with neurodevelopmental disorders. These are more difficult to quantify on a shifting backdrop of increasing diagnosis, expanding definitions and potential ascertainment bias [50]. In 2016, 1.85% of children in USA were estimated to have autism compared to 0.67% in 2000 [51]. Scandinavian population studies of maternal valproate exposure report an increased diagnosis of autism (2.5% versus 0.5% in the general population [52]) and attention–deficit/hyperactivity disorder [53]. The mean IQ of children at 6 years with maternal valproate exposure (49/62 children from 25 centres in the UK and US, countries with different educational systems), fell within the normal range at 97 (95% confidence interval 94–101), but lower than for those with maternal lamotrigine exposure (108, CI 105–110). Mean maternal IQ of mothers taking valproate was 96 (CI 92–100), lower than the mean maternal IQ of mothers taking lamotrigine (101, CI 98–104) but all within the normal range [53]. Guidelines and MHRA regulatory statements quote neurodevelopmental problems in 30–40% of offspring of mothers taking valproate [7, 14, 22, 23]. These figures are higher than estimates from population studies of neurodevelopmental disorders in 6.5% of children of mothers taking valproate compared to 2.4% in mothers with untreated or resolved epilepsy [54, 55].
Men
There is little data on the impact of epilepsy and its treatment with ASMs on sexual function in men, with no Grade A evidence or registry studies [1, 34]. Sexual dysfunction is variably defined, and surveys in the general male population estimate the range is from 9.6% of 594 in Norway [57] to 31% of 1410 in US [58] and is reported in two-thirds of men with refractory epilepsy [57]. Epilepsy and ASMs have direct and indirect influences on sexual function and dysfunction including hyposexuality, erectile dysfunction, hypersexuality or impaired fertility (Table 1).
ASMs potentially reduce male fertility through hormonal effects, erectile dysfunction or reduced sperm quality. Teratogenicity or neurodevelopmental problems in offspring of men could be possible through direct transmission of ASMs to the embryo, or through genetic or epigenetic mechanisms. The latter has the potential to cause transgenerational damage. These are discussed, along with evidence from population studies.
Valproate and male fertility-hormonal effects
Data on reproductive hormones in men taking valproate are contradictory and limited to small numbers (Grade C evidence) [34, 59,60,61, 66, 69]. A review totalling 444 patients and 398 controls found that valproate had fewer hormonal effects than enzyme-inducing ASMs [59]. Another review found an association between valproate use in men and lowered testosterone, p = 0.04 [60]. Contradictory findings were found in a controlled study in 90 men for whom in those treated with valproate, 57% had elevated serum androgens (n = 12, p 0.001) as compared with 20% in those taking carbamazepine and 8% in controls [61]. In another study, of 70 males with epilepsy treated with VPA (age-matched to 70 controls) (age range 7–20 years) androgen levels were elevated in 45 (64%, p = 0.0006) particularly in prepubertal patients (p = 0.0003) [62].
Erectile dysfunction
Valproate reduced rodent erectile dysfunction and penile fibrosis in a small study [63] and is trialled as a neuroprotective agent to reduce the risk of erectile dysfunction requiring radical prostatectomy [64]. Population surveys report erectile dysfunction in 2% of healthy men < 40 years and up to 80% of men > 80 years [65]. 42.5% of 80 men with epilepsy reported erectile dysfunction using the self-administered scale [66] with similar rates (38.6%) in an uncontrolled hospital cross-sectional survey in men with neurologic disability [67] (Grade C evidence). Self-reported reduction in erectile function was noted by men taking valproate (n = 32) and levetiracetam (n = 30) compared to controls without epilepsy on no medication, along with reduced sperm motility in both groups; and increased abnormal sperm in the valproate group [68].
Valproate and male fertility—sperm
Pharmacological modelling estimates that concentrations of valproate are < 25,000 times lower for male seminal fluid than the equivalent dose of a single oral 500 mg tablet for women. Therefore, paternal valproate ingestion does not cause adverse effects to the embryo via direct passage [69]. The applicability of animal studies to human experience is debated, particularly in relation to the doses used in animal models. For example, recent studies used valproate doses of 7–33 times the maximum human dose equivalent [70]. Testicular atrophy is reported in rats given valproate at 13 times the human dose equivalents [71]. Other valproate rodent studies report reversible abnormalities in sperm count and motility [70]. Fertility was unchanged in male rats given up to 500 mg/kg/day (17 × maximum human dose), but sperm motility and weights of epididymis, seminal vesicles and prostate were decreased. At higher doses, of 1000 mg/kg/day—equivalent to human dose of 70,000 mg daily (> 33 times the maximum human dose) the rats were moribund or dead at day 5 of the experiment [70].
Sperm and semen quality, morphology and quantity fluctuate significantly in all males and is affected by mood, stress, season, age, ethnicity and lifestyle factors (including alcohol, cigarettes, cannabis, exercise and even choice of underwear) in males without and with epilepsy [72].
There are reports of abnormalities in semen analysis, lower sperm count and motility, and dysmorphic sperm in men with epilepsy before starting ASMs [73]. Similar findings are seen in men prescribed carbamazepine, oxcarbazepine, phenobarbital, phenytoin, valproate, and levetiracetam (Grade B &C) [34]. Lamotrigine has the least reported impact on spermatogenesis [73], with little data on the newer ASMs.
There is Grades B–D evidence of abnormalities in sperm count, morphology and motility in men taking valproate [34, 74,75,76,77]. Reduced testicular volume and sperm abnormalities were reported in 27 men treated with valproate compared to 41 controls [73] with similar findings in another study of 25 men [74]. A case study, without controls or pre-treatment values found a reversible reduction in sperm count in a man taking valproate [77]. Oxcarbazepine, levetiracetam and lamotrigine had no significant effect on sexual function and sex hormones in a study of 38 men. In fact, oxcarbazepine improved sperm motility and survival rate [78]. In 26 men taking levetiracetam, total sperm count, percentage of normal morphology and functional sperm count tested after treatment were significantly lower compared with pre-treatment values (p < 0.05), but there were no effects on hormone levels [79]. There is little data on the newest ASMs.
Genetic and transgenic effects
Tests for gene mutations related to valproate in sperm cells are negative, therefore, transmission is unlikely. Some tests for severe chromosome damage were positive which would lead to sperm cell death and thus no transmission of mutations to offspring. Whether milder chromosomal damage might be transmitted to the offspring is unknown [69].
Epigenetic mechanisms for example via DNA methylation have been postulated as a mechanism for transgenerational passage of autism [79, 80]. A rodent study proposed it as a potential mechanism for teratogenic effects of valproate in second and third generation and increased levels of autism [80]. Study limitations are valproate doses equivalent to 12 × human dose (28000 mg), and small sample size (4 dams in each group). There was no testing of generation 0. The parents of the first generation of mice offspring were not controlled in comparison to their male offspring, only male offspring were studied. The findings also included a reduction in anxiety in first, second and third generation offspring, which was not explained or discussed in the conclusion. Researchers found a lowered threshold in the electroshock model (used as a surrogate for seizures), and they imputed that the male mice with mothers exposed to valproate had an increased risk of seizure. This is both biologically implausible and never described in other models or in humans.
Another study failed to replicate transgenerational effects in mice [79]. Valproate administration induced histone hyperacetylation in testes, but this effect was transient and did not translate to the next generation. Doses used of 200 mg/kg were equivalent to 14,000 mg daily (6 × the usual human maximum dose). Behavioural testing showed a change in light–dark behaviour suggestive of reduced anxiety (not autistic-like behaviour) in the first generation. The authors concluded that valproate treatment relaxes chromatin and increases susceptibility to epigenomic changes but does not produce DNA methylation changes that would persist for multiple generations.
Population studies
There have been recent concerns about a possible increase in major congenital abnormalities and neurodevelopmental disorders (intellectual disability (ID); Communication disorders; Autism Spectrum Disorder (ASD); Attention–Deficit/Hyperactivity Disorder (ADHD); Neurodevelopmental motor disorders, including Tic disorders; and Specific learning disorders) [81] in offspring of males taking valproate. Population studies provide large datasets which can inform this question, but caution is needed to avoid conflating association with causality, assessing homogeneity of cohorts, and critical granularity is lacking [82].
In a nationwide, Swedish registry study of > 1 million births 4544 births were recorded to 2955 fathers with epilepsy, of whom 45.9% were prescribed ASMs during conception. There was no increased risk of MCM, autism, ADHD or intellectual disability compared with offspring of fathers with epilepsy not exposed to ASMs. Rates of autism were 2.9 per 1000 child-years and intellectual disability was 1.4 per 1000 child-years in the offspring of fathers with epilepsy on valproate monotherapy. These were slightly higher compared with the offspring of fathers with epilepsy who did not use ASMs, but the propensity score adjusted analyses showed no statistically significant increased risk of adverse outcomes [83].
A Norwegian prescription database of 340 000 pregnancies occurring between 2004 and 2010 investigated offspring outcomes from fathers and specific drugs dispensed during 3 months prior to conception. 26% of the fathers were dispensed one or more drugs and 1.3% were dispensed at least one drug “requiring special attention.” Adverse pregnancy outcomes were generally not increased [OR 0.99 (95% CI 0.94, 1.0)]. Valproate was not associated with increased risk [84]. The exception was fathers dispensed diazepam who had increased risks of perinatal mortality and growth retardation, with OR and 95% CIs of 2.2 (1.2, 3.9) and 1.4 (1.2, 1.6), respectively. Highlighting the pitfalls of equating correlation and causation [82] further analysis uncovered that diazepam use in males correlated with smoking and co-diazepam use in their female partners. Removing this confounder eliminated any correlation between male use of diazepam and increased risks in offspring [85].
A 2019 Danish population-based study in 733, 282 males found a 23% increase in congenital malformations in offspring of fathers using ASMs [86]. When extending the exposure window to 1 year before conception to the end of pregnancy, except for those using ASMs during the 3 months before conception (the susceptible period of exposure), the increased risks were also observed in children whose fathers were former users (i.e., those using ASMs only from 1 year to 3 months before conception) (OR 1.29, 95% CI 1.03–1.61) and later users (i.e., those using ASMs only during pregnancy after conception of their child) (OR 1.35, 95% CI 1.12–1.65). This study suggested that the increased risk of congenital anomalies in the offspring associated with paternal ASMs use before and after conception may be attributable to the underlying indications related to ASMs use; and unlikely to be ascribable to ASMs.
Ethics of patient choice
The discrepancy between advice about the first-choice treatment offered to men and women arising from previous MHRA guidelines whereby men with generalised tonic–clonic seizures were offered valproate as "first-choice" and women were not, created legal and ethical challenges. Health care professionals were aware of their ethical obligations to treat a patient based on clinical need and within the Equality Act (or equivalent legislation outside the UK). There were major implications in exposing only women to a higher risk of seizures resulting from use of less efficacious medication.
The new January 2024 MHRA regulation removes this difference for all people under the age of 55 years [26], now exposing individuals with epilepsy to a higher risk of seizures. While seen as a solution to address the gender gap, this brings considerable new challenges to prescribers while still not addressing some existing concerns.
Both the new and previous MHRA regulation and it’s recording systems—the RMMs—conflict with a range of ethical–legal issues:
-
The Montgomery and McCulloch rulings.
-
GMC Guidance on informed consent.
-
Article 2 of the European Convention on Human Rights (ECHR)
-
The common law principle of English Law which holds that patient autonomy takes precedence over concern for the health of a future child
The Montgomery and McCulloch ruling
The RMM guidelines do not address the legal challenge encapsulated in judgment in Montgomery v Lanarkshire Health Board [2015] [87]. The medical professional must take reasonable care to ensure that the patient is aware of any material risks involved in any recommended treatment—but also any suitable alternative or variant treatments [2, 6, 87].
The question of “who decides” which alternative treatments are suitable was recently considered in Bilal & Anor v St George’s University Hospital Trust [2023] [88] and McCulloch and others v Forth Valley Health Board [2023] [89]. Both the Court of Appeal and Supreme Court held, respectively, that this decision is a matter of “professional skill and judgment to which the professional practice (Hunter v Hanley/Bolam) test should be applied.” Further, the Court in Bilal emphasised the importance of the specific medical speciality when determining alternative treatments. These judgements mean that the option of treatment with valproate must be discussed with everyone who presents with responsive seizure types, particularly if it is likely to be the most efficacious treatment for them [31].
The law is clear on the role of clinicians on such matters. It is not satisfactory to simply present the patient with technical information “which she cannot reasonably be expected to grasp, let alone by routinely demanding her signature on a consent form” (Montgomery [2015] UKSC 11 at 90) [87].
Yet regulatory body information leaflets for patients [20,21,22,23,24,25,26] do not outline the risks of stopping valproate estimated as a 30–40% chance of recurrence or worsening of seizures [90, 91]. Neither do they explain the risks of “user independent” contraception, nor the risks and benefits of the alternative treatments. Thus, the MHRA valproate regulations do not meet requirements for patient decision-making in line with the Montgomery ruling regarding disclosure of ‘material risks’[6, 87].
GMC guidance on informed consent
MHRA regulations also appear to conflict with the GMC guidance on treating individuals who can make their own decisions, in partnership with their doctors. The GMC and the law respect the fact that patients in their decision-making process can retain the right to make “unwise decisions” or decisions their doctors may not agree with [93]. Following the "GMC Decision Making and Consent Professional Standards"(2020: principle 4, reference): “doctors must try to find out what matters to patients so they can share relevant information about the benefits and harms of proposed options and reasonable alternatives, including the option to take no action.” Guidance includes that doctors should explore:
-
“what matters to patients about their health—their wishes and fears, what activities are important to their quality of life, both personally and professionally—so you can support them to assess the likely impact of the potential outcomes for each option.
-
“with patients what risks they would and wouldn’t be prepared to take to achieve a desired outcome, and how the likelihood of a particular outcome might influence their choice
The current MHRA guidance puts clinicians in a bind as based on medical expertise, valproate is a ‘reasonable alternative’, as the most effective medication for some epilepsies [6, 9,10,11,12,13]. In prescribing this, potentially off-licence if MHRA requirements are not met irrespective of the impact on people with epilepsy themselves, prescribers may fall foul of the MHRA. In not prescribing valproate for an informed patient opting for it, they fail the patient, as well as their legal and GMC obligations.
Article 2 of the European Convention on Human Rights (ECHR) [93]
This specifies “a positive duty to prevent foreseeable loss of life.” Alternatives to valproate are likely to be less effective for a significant number and, therefore, carry greater risk of sudden death. At the minimum, this must be discussed with patients and their carers. Patients who elect to avoid valproate require closer monitoring, opportunities for urgent review and the right to change to valproate treatment. For some, this is too late, and SUDEP has occurred in an unknown and unmonitored number of people avoiding valproate.
The common law principle of English Law [94]
This holds that an individual with capacity can accept or refuse treatment—even if it is against medical advice or not in the best interest of a possible future child. The law is clear that a competent woman who has the capacity to decide may, for religious reasons, other reasons, or for no stated reasons at all, choose not to have medical intervention, even though, the consequence may be the death or serious disability of the child she bears, or her own death. The foetus up to the moment of birth does not have any separate interests capable of being taken into account when a court has to consider an application for a declaration in respect of a caesarean section operation. The court does not have the jurisdiction to declare that such medical intervention is lawful to protect the interests of the unborn child even at the point of birth. [95](Re MB [1997] EWCA Civ 3093 (following statement made in support of an earlier case—Re T [1992] 4 All ER).
The MHRA’s stated aim is preventing any pregnancies in parents taking valproate, focusing on foetal risk [6, 11, 13, 96]. This treats a valproate exposed pregnancy as a “never event” and protects against certain future legal claims (Box 2) [96]. The assumption that valproate usage is “preventable” enforces a certain definition, which is not supported by the science. This raises questions around the moral and legal status of the “hypothetical foetus” especially if medication is restricted among people who are not actively planning pregnancies. Current MHRA regulation means that the prevention of potential harm to a hypothetical foetus takes priority over ensuring the availability of effective life changing medication and implies that all individuals for valproate purposes should always be treated as “pre-parents” [6, 11, 96,97,98,99].
The recent Confidential Inquiry into Maternal Deaths [97] has identified an increase in the deaths of women with epilepsy during pregnancy, and without specifically attributing this to changes in use of valproate in this population the authors do say: “It is of concern that current discourse around valproate use remains focussed around fetal risk without the essential focus on ensuring that women receive alternative effective anti-epileptic medication.”
Discrimination in reproductive rights
In many countries, people may make reproductive decisions with a wide range of options. For example, a person with a serious autosomal dominant genetic condition may choose to have a child without any intervention, or have a termination if they get pregnant, or have pre-natal testing if that is available [6]. They are not required to use contraception, nor told what type of contraception they must use, in order to obtain optimal medical care. They may decline to discuss their sexuality with their healthcare professionals if they wish. People choosing valproate as their treatment are denied these rights [6, 96, 98, 99]. In addition, they now, as per the new MHRA guidelines, may face the stress of potentially running out of their life-saving medication if the necessary reviews and dual signatories are not completed in time [15, 99].
Circumstances when a patient or representatives elects for valproate and not the Pregnancy Prevention Programme (PPP)
There are situations in which a child or adult or their authorised representative may decide that she will continue valproate even though she might be, or may become, pregnant, and when the PPP is not appropriate (Box 3).
Patients may elect for valproate as their preferred treatment option, but decline PPP
People may make this decision de novo, if evidence suggests that valproate is likely to be the most effective medication. They may wish to avoid trials of less effective medication, to reduce the risk of injury, disruption to their life, employment and driving, and SUDEP (1/500 on average, 1/100 for refractory epilepsy) [100]. Patients may undergo one or more unsuccessful trials of other medications in line with MHRA guidelines to avoid valproate, and then opt for valproate treatment. Symptom free patients may wish to remain on valproate to avoid the risks to their personal safety of seizure recurrence in changing to another medication, which survey evidence (4774 patient encounters by 215 clinicians) [90] and a population study [91] suggest is in the order of 30–40%. There are little data on the long-term effects of exposure of babies, infants and children to uncontrolled seizures during their period of maximum neural development, but Grade C evidence suggests that it may damage cognitive development [6]. Some parents or guardians may elect for their child to be on valproate without contraception to optimise seizure control, safety and learning.
After informed discussion, people may decline the contraception recommended by the MHRA for personal, religious or health reasons. For some people sexual relationships outside marriage are forbidden for religious or cultural reasons and using any form of contraception before marriage is thus unacceptable. Other people who do not have heterosexual sex, i.e., who are abstinent, celibate, asexual (ace), or in same-sex relationships may find the PPP unnecessary and unacceptable, and probing about their sexuality intrusive and undignified. Women who are not able to become pregnant for health‐related or physical reasons will not wish to have “user independent” contraception, and repeated discussions as currently stipulated by the PPP when the situation is unchanged, may find the whole experience unpleasant and superfluous. Some women will prefer other contraception.
Intellectual disability (ID)
Systematic reviews estimate that 22% of people with ID have epilepsy, and prevalence rises with the increasing severity of ID [101]. Two-thirds of the population with ID and epilepsy are treatment resistant [102]. Only 5% of research in epilepsy focuses on ID and many clinical trials in epilepsy exclude people with ID [103, 104]. People with ID and epilepsy have significantly higher multi-morbidity, polypharmacy and higher rates of premature mortality than their peers with epilepsy or intellectual disability [105]. Further, SUDEP and epilepsy related harm is considered to be of higher risk in this population [105,106,107]. A third of People with ID and epilepsy suffer psychiatric comorbidities [105,106,107,108].
A Cochrane review recommended using the same treatment paradigms for people with epilepsy and ID as the general population [109], however this is an area which has a poor evidence base especially given the other issues. An expert consensus study suggested that valproate should be considered as first line drug in men with ID [110]. Valproate is often a good choice given its additional mood-stabilising effects, and in those with autism, thus reducing polypharmacy. It has been shown to be the most prescribed ASM in international comparison studies [110,111,112]. Valproate remains a first-line drug for generalised seizures and people with ID and a number of genetic syndromes are specifically responsive [112, 113]. As valproate is a mainstay of treatment in this population, excluding it as a treatment option puts many vulnerable individuals at significant risk of harm.
People with moderate to profound intellectual disability (ID) will usually lack the mental capacity to consent to sexual relationships and pregnancy in this population would raise serious safeguarding concerns, implying sexual abuse [9, 10, 12]. “User independent” contraceptives may put women in this population at unnecessary risk. There may be other clinical indications for contraceptive use such as dysmenorrhea; therefore, each case needs to be considered on an individual basis following the best-interests process under the 2005 Mental Capacity Act (MCA) or local equivalent [9,10,11,12]. Repeated discussions on this topic mandated by a yearly consent form can be an unnecessary and distressing process for the individual and their families [6, 9, 12].9B
The default position is always to assume people have mental capacity [9, 12, 98]. Those with mild ID should be managed as such unless there is clear evidence otherwise. They may need extra time and additional support from carers in their decision making, and possibly augmented communication. In this there is a significant concern that older people with ID and epilepsy would lack suitable consistent representation. It has been evidenced that their epilepsy care is poorer than their younger peers while needs are greater [113].
Emergency situations
In emergencies such as status epilepticus or serial seizures, discussion with the patient is usually not possible and treatment is given on a best interest basis under mental capacity legislation [9, 10]. Emergency care should never be delayed because of potential teratogenicity or pregnancy. The MMBRACE report highlights fatal outcomes caused by withholding life-saving treatments because of fears of harming the foetus [98]. Emergencies in pregnancy require proactive and same care as non-pregnant people. Informed discussions about the associated benefits and risks of continuation of valproate would need to be undertaken on recovery with the person, or their advocates if capacity is impaired [6, 9, 10, 101, 112].
Recommendations (see Table 2).
Full disclosure by the MHRA
The MHRA should disclose all information and the Minutes of discussions about valproate and all medications under their scrutiny. It is a concerning precedent that they have made a major decision influenced by unpublished materials especially as they may have not been peer-reviewed. There is acknowledgement that the study was flawed but needs to be factored to the decision currently held. Disclosures and potential conflict of interest (both professional and personal) of individual members of the MHRA committees and the funding sources for the MHRA should be made freely available to the public.
Adequate resources for informed patient choice and outcome monitoring
In the USA, there were 3 million valproate prescriptions in 2021 [115]. In 2021, the MHRA estimated there were ~ 20,000 females and ~ 50,000 males taking valproate in the UK [7]. Many of the adult men on valproate are not under specialist care, as they are seizure free. Primary care professionals are now under pressure to refer these patients for review, to already overstretched secondary care facilities. The MHRA has not provided resources for the task of identifying and reviewing these patients. This leaves patients vulnerable to running out of medication and to breakthrough seizures, not to mention the unquantified significant risk emerging on mental health issues. The projected 30–40% of seizure recurrences in those stopping valproate [90, 91] leaves these patients needing urgent medication review, at risk of SUDEP (1/500) [100], and unable to drive with implications for quality of life, employment and other responsibilities.
Adherence to medication regimens by people with epilepsy is fragile—although missing tablets is associated with a risk of morbidity and mortality/SUDEP, up to 79% of people may not take their medication as recommended [116]. Numerous factors are relevant, but among them are a patient's beliefs and understanding about the risks and benefits of the drug they are prescribed and logistical barriers to patients receiving regular scripts [99, 117]. To optimise adherence, a doctor must ensure that the messages about the medication and its use are communicated clearly. This cannot be done effectively without more resources, particularly clinician time.
Studies of outcomes of the decision-making regarding valproate are needed—these should be government funded and relate to all patients considering valproate and alternatives, and those switching to other medications.
Reversion to 2016 international guidelines
The 2016 Joint Task Force guidelines of the International League Against Epilepsy, Commission on European Affairs, and European Academy of Neurology (adopted in China and elsewhere) focus of informed decision-making by the patient, balancing the risks and benefits for the individual patient.
Conclusions
There is consensus on the teratogenic harms of valproate for pregnant women and the risk of neurodevelopmental disorders in offspring. The patients and families harmed by valproate, and those who were not warned about these, are outraged. They deserve full compensation and financial and social support, as do all vulnerable and disabled people in societies promoting equality and social justice.
The impact of valproate on male fertility and possible epigenetic effects are unknown, and the MHRA has refused to release the unpublished information on which they have based their restrictions in men. The UK is the only country with such restrictions. They do not align with the Montgomery and McCulloch judgements, GMC regulations or common law principles.
Recent regulations imposed by the MHRA effectively limit or prevent people from choosing valproate, even in circumstances when it is the only medication to prevent life-threatening seizures. 30–40% of people with epilepsy coming off valproate are predicted to experience seizures. Deaths have occurred because of the avoidance of valproate, and more will, unless the regulations are urgently amended. This article focused on adults with epilepsy, but there are also people with bipolar disorder or other mental health problems for whom valproate is the best medication to keep them well. They are often too unwell to advocate for themselves. Uncontrolled seizures, cognitive and neurodevelopmental consequences for young people and children denied valproate from birth have potential long-term and irreversible consequences. It is ironic that restrictions to protect future unborn offspring will harm the neurocognitive development and well-being of some living children.
Necessary elements to ensure patient safety include a return to the consensus valproate guidelines of 2016, resources for monitoring of patient outcomes, public scrutiny of the withheld reports and minutes of MHRA proceedings on valproate, and restoration of informed decision-making for people considering valproate as a treatment.
References
Oxford Centre for evidence-based medicine (2011). www.cebm.net/ocebm-levels-of-evidence/. Accessed Nov 2020
Valproate and malformations. Lancet. 1982 2(8311):1313–4. (PMID: 6128602)
Pennell PB (2016) Use of antiepileptic drugs during pregnancy: evolving concepts. Neurotherapeutics 13:811–820. https://doi.org/10.1007/s13311-016-0464-027502786
Marson A, Burnside G, Appleton R, Smith D, Leach JP, Sills G, Tudur-Smith C, Plumpton C, Hughes DA, Williamson P, Baker GA, Balabanova S, Taylor C, Brown R, Hindley D, Howell S, Maguire M, Mohanraj R, Smith PE, SANAD II Collaborators (2021) The SANAD II study of the effectiveness and cost-effectiveness of valproate versus levetiracetam for newly diagnosed generalised and unclassifiable epilepsy: an open-label, non-inferiority, multicentre, phase 4, randomised controlled trial. Lancet 397(10282):1375–1386. https://doi.org/10.1016/S0140-6736(21)00246-4. (Erratum in: Lancet. 2021 May 15;397(10287):1808. PMID: 33838758; PMCID: PMC8047813)
Ehlken B, Nishikawa C, Kaplan S, Dresco I, Granados D, Toussi M (2022) Effectiveness of risk minimization measures for valproate: a drug utilization study based on implementation of a risk minimization programme in Europe, analysis of data from the UK. Curr Med Res Opin 38(3):461–468. https://doi.org/10.1080/03007995.2021.1997286. (Epub 2022 Jan 8 PMID: 34931552)
Angus-Leppan H, Liu RSN (2018) Weighing the risks of valproate in women who could become pregnant. BMJ 18(361):k1596. https://doi.org/10.1136/bmj.k1596. (PMID: 29669717)
Update on MHRA review into safe use of valproate. GOV.UK. 2022.https://www.gov.uk/government/news/update-on-mhra-review-into-safe-use-of-valproate accessed 27 Apr 2023
Zhou SM, McLean B, Roberts E, Baines R, Hannon P, Ashby S, Newman C, Sen A, Wilkinson E, Laugharne R, Shankar R (2023) Analysing patient-generated data to understand behaviours and characteristics of women with epilepsy of childbearing years: a prospective cohort study. Seizure 108:24–32. https://doi.org/10.1016/j.seizure.2023.04.008
Watkins L, Cock H, Angus-Leppan H, Morley K, Wilcock M, Shankar R (2019) Valproate MHRA guidance: limitations and opportunities. Front Neurol 10:139. https://doi.org/10.3389/fneur.2019.00139
Watkins LV, Cock HR, Angus-Leppan H et al (2019) Valproate and the pregnancy prevention programme: exceptional circumstances. Br J Gen Pract 69:166–167. https://doi.org/10.3399/bjgp19x701897
Lawthom C (2018) Valproate and epilepsy: for women as well as men. Pract Neurol 18:222–223. https://doi.org/10.1136/practneurol-2018-001931
Watkins L, Reuber M, Perera B, Courtenay K, Banks R, Murphy E, Angus-Leppan H, Shankar R (2021) Valproate prescribing practices for women with intellectual disability across Europe. Acta Neurol Scand 143(1):56–61. https://doi.org/10.1111/ane.13337
The Lancet Neurology (2024) Reducing the uses of valproate: a controversial decision. Lancet Neurol 23(2):123. https://doi.org/10.1016/S1474-4422(23)00507-0. (Erratum.In:Lancet Neurol. 2024 Feb16; PMID: 38267170)
The Medicines and Healthcare products Regulatory Agency. Valproate: organisations to prepare for new regulatory measures for oversight of prescribing to new patients and existing female patients. https://assets.publishing.service.gov.uk/media/65660310312f400013e5d508/Valproate-report-review-and-expert-advice.pdf, Accessed Dec 2023.
Public statement from coalition of Epilepsy organisations. SUDEP Action. 2023.https://sudep.org/article/public-statement-coalition-epilepsy-organisations accessed 27 Apr 2023
Medsafe New Zealand. Valproate in pregnancy 2014. http://www.medsafe.govt.nz/profs/PUArticles/December2014SodiumValproate.htm 2018.
Tomson T, Marson A, Boon P, Canevini MP, Covanis A, Gaily E, Kälviäinen R, Trinka E (2015) Valproate in the treatment of epilepsy in girls and women of childbearing potential. Epilepsia 56(7):1006–1019. https://doi.org/10.1111/epi.13021. (Epub 2015 May 16 PMID: 25851171)
FDA. Drug Safety Communication: valproate anti-seizure products contraindicated for migraine prevention in pregnant women due to decreased IQ scores in exposed children. 2013. https://www.fda.gov/Drugs/DrugSafety/ucm350684.htm.
Agence nationale de sécurité du médicament et des produits de santé (ANSM). Valproate and derivatives. 2017. http://ansm.sante.fr/Dossiers/Valproate-et-derives/Valproate-et-derives/(offset)/02018, accessed Dec 2018
Medicines & Healthcare Products Regulatory Agency. New measures to avoid valproate exposure in pregnancy. 2018. https://www.gov.uk/government/news/new-measures-toavoid-valproate-exposure-in-pregnancy, accessed Dec 2018
European Medicines Agency. Valproate and related substances. EMA/145600/2018.2018. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Valproate_and_related_substances/human_referral_prac_000066.jsp&mid=WC0b01ac05805c516f, accessed Dec 2018
Medicines & Healthcare Products Regulatory AgencyUpdate on MHRA review into safe use of valproate https://www.gov.uk/government/news/update-on-mhra-review-into-safe-use-of-valproate, accessed Dec 2022
Medicines & Healthcare Products Regulatory Agency. Safety of valproate—new study on risks in children of men taking valproate. https://www.gov.uk/government/news/safety-of-valproate-new-study-on-risks-in-children-of-men-taking-valproate, accessed Dec 2023.
European Medicines Agency. EMA recommends precautionary measures following review of study in children whose fathers were treated with valproate. https://www.hpra.ie/homepage/medicines/special-topics/valproate-(epilim)/valproate-(epilim-)-ema-review-of-study-in-children-whose-fathers-were-treated-with-valproate, accessed Dec 2023.
New Zealand Medsafe. Sodium valproate (Epilim) use in people who can father children: important new safety information - Update to original communication Internet. Document: 7 Dec 2023. Available from: URL: https://www.medsafe.govt.nz/safety/Alerts/Sodium_valproate_Epilim_use_in_people_who_can_father_children.asp, accessed Dec 2023.
Medicines & Healthcare Products Regulatory Agency. New valproate safety measures apply from 31 January, https://www.gov.uk/government/news/new-valproate-safety-measures-apply-from-31-january#:~:text=From%20today%20%5B31%20January%202024,of%20impaired%20fertility%20in%20males. Accessed Jan 2024
Rahman M, Awosika AO, Nguyen H. Valproic acid. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK559112/
Cipriani A, Reid K, Young AH, Macritchie K, Geddes J (2013) Valproic acid, valproate and divalproex in the maintenance treatment of bipolar disorder. Cochrane Database Syst Rev 2013(10):CD003196
Gill D, Derry S, Wiffen PJ, Moore RA (2011) Valproic acid and sodium valproate for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev 2011(10):CD009183. https://doi.org/10.1002/14651858.CD009183.pub2. (PMID: 21975791; PMCID: PMC6540387)
Perucca E (2002) Pharmacological and therapeutic properties of valproate: a summary after 35 years of clinical experience. CNS Drugs 16(10):695–714. https://doi.org/10.2165/00023210-200216100-00004. (PMID: 12269862)
National Institute for https://www.nice.org.uk/guidance/ng217/chapter/5-Treating-epileptic-seizures-in-children-young-people-and-adults. Epilepsies in children, young people and adults, NICE guideline [NG217] Published: 27 April 2022, accessed Dec 2022
Guerrini R (2006) Valproate as a mainstay of therapy for pediatric epilepsy. Paediatr Drugs 8(2):113–129. https://doi.org/10.2165/00148581-200608020-00004. (PMID: 16608372)
Cross JH, Caraballo RH, Nabbout R, Vigevano F, Guerrini R, Lagae L (2019) Dravet syndrome: treatment options and management of prolonged seizures. Epilepsia 60(Suppl 3):S39–S48. https://doi.org/10.1111/epi.16334.PMID:31904119
Watkins LV, Angus-Leppan H (2020) Valproate, sexual health, and men: a narrative review. Epilepsy Behav 103(Pt A):106835. https://doi.org/10.1016/j.yebeh.2019.106835. (Epub 2019 Dec 28. PMID: 31892466)
Sare G, Rawnsley M, Stoneman A, Duncan S (2007) Men with epilepsy—the lost tribe? Results of a nationwide survey of men with epilepsy living in the UK. Seizure 16(5):384–396
Wu D, Chen L, Ji F, Si Y, Sun H (2018) The effects of oxcarbazepine, levetiracetam, and lamotrigine on semen quality, sexual function, and sex hormones in male adults with epilepsy. Epilepsia 59(7):1344–1350
Artama M, Isojärvi JIT, Auvinen A (2006) Antiepileptic drug use and birth rate in patients with epilepsy—a population-based cohort study in Finland. Hum Reprod 21(9):2290–2295
Isojärvi JI, Laatikainen TJ, Knip M, Pakarinen AJ, Juntunen KT, Myllyla VV (1996) Obesity and endocrine disorders in women taking valproate for epilepsy. Ann Neurol 39(5):579–584
Pylvänen V, Pakarinen A, Knip M, Isojärvi J (2006) Characterization of insulin secretion in valproate-treated patients with epilepsy. Epilepsia 47(9):1460–1464
McCool-Myers M, Theurich M, Zuelke A et al (2018) Predictors of female sexual dysfunction: a systematic review and qualitative analysis through gender inequality paradigms. BMC Womens Health 18:108. https://doi.org/10.1186/s12905-018-0602-4
Abo Al-Azayem S, Kishk NA, Shamloul R, Attia A, Elsayed RM, Magdy R (2023) Patterns and predictors of sexual dysfunction in women with epilepsy. Epilepsy Behav 147:109421. https://doi.org/10.1016/j.yebeh.2023.109421. (Epub 2023 Sep 6 PMID: 37677900)
Bromley R, Weston J, Adab N et al (2014) Treatment for epilepsy in pregnancy: neurodevelopmental outcomes in the child. Cochrane Database Syst Rev 10:CD010236. https://doi.org/10.1002/14651858.CD010236.pub2
Tomson T, Battino D (2012) Teratogenic effects of antiepileptic drugs. Lancet Neurol 11:803–813. https://doi.org/10.1016/S1474-4422(12)70103-5.22805351
Battino D, Tomson T, Bonizzoni E, Craig J, Perucca E, Sabers A, Thomas S, Alvestad S, Perucca P, Vajda F, EURAP Collaborators (2024) Risk of major congenital malformations and exposure to antiseizure medication monotherapy. JAMA Neurol 18:e240258. https://doi.org/10.1001/jamaneurol.2024.0258
Campbell E, Kennedy F, Russell A et al (2014) Malformation risks of antiepileptic drug monotherapies in pregnancy: updated results from the UK and Ireland Epilepsy and Pregnancy Registers. J Neurol Neurosurg Psychiatry 85:1029–1034. https://doi.org/10.1136/jnnp-2013-30631824444855
Hernández-Díaz S, Smith CR, Shen A, North American AED Pregnancy RegistryNorth American AED Pregnancy Registry et al (2012) Comparative safety of antiepileptic drugs during pregnancy. Neurology 78:1692–1699. https://doi.org/10.1212/WNL.0b013e3182574f3922551726
Vajda FJ, O’Brien TJ, Graham JE, Lander CM, Eadie MJ (2013) Dose dependence of fetal malformations associated with valproate. Neurology 81:999–1003. https://doi.org/10.1212/WNL.0b013e3182a43e8123911758
Tomson T. Teratogenic and other considerations in the selection of antiepileptic drugs in girls and women. 2017. https://www.ean.org/amsterdam2017/fileadmin/user_upload/TC07_03_Tomson.pdf. Accessed Dec 2018
Jazayeri D, Graham J, Hitchcock A, O’Brien TJ, Vajda FJE (2018) Outcomes of pregnancies in women taking antiepileptic drugs for non-epilepsy indications. Seizure 56:111–114. https://doi.org/10.1016/j.seizure.2018.02.00929471258
Watkins LV, Angus-Leppan H (2023) Increasing incidence of autism spectrum disorder: are we over-diagnosing? Adv Autism 9(1):42–52. https://doi.org/10.1108/AIA-10-2021-0041
Maenner MJ, Shaw KA, Baio J (2020) Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ 69(4):1–12. https://doi.org/10.15585/mmwr.ss6904a1externalicon
Christensen J, Grønborg TK, Sørensen MJ et al (2013) Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 309:1696–1703. https://doi.org/10.1001/jama.2013.227023613074
Meador KJ, Baker GA, Browning N, Cohen MJ, Bromley RL, Clayton-Smith J et al (2013) Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol 12(3):244–252
Cohen MJ, Meador KJ, Browning N, May R, Baker GA, Clayton-Smith J, Kalayjian LA, Kanner A, Liporace JD, Pennell PB, Privitera M, Loring DW (2013) Fetal antiepileptic drug exposure: adaptive and emotional/behavioral functioning at age 6years. Epilepsy Behav 29(2):308–315. https://doi.org/10.1016/j.yebeh.2013.08.001. (Epub 2013 Sep 5. PMID: 24012508; PMCID: PMC3902100)
Bjørk M-H, Zoega H, Leinonen MK, Cohen JM, Dreier JW, Furu K, Gilhus NE, Gissler M, Hálfdánarson Ó, Igland J, Sun Y, Tomson T, Alvestad S, Christensen J (2022) JAMA Neurol 79(7):1–10. https://doi.org/10.1001/jamaneurol.2022.1269
Veiby G and others. Exposure to antiepileptic drugs in utero and child development: a prospective population-based study. Epilepsia 2013: volume 54, pages 1462 to 1472.
Henning OJ, Nakken KO, Træen B, Mowinckel P, Lossius M (2016) Sexual problems in people with refractory epilepsy. Epilepsy Behav 61:174–179
Laumann EO, Paik A, Rosen RC (1999) Sexual dysfunction in the United States: prevalence and predictors. JAMA 281(6):537–544
Lambert MV (2001) Seizures, hormones and sexuality. Seizure 10(5):319–340
Zhao S, Wang X, Wang Y, Xu J, Zhu G, Zhao C et al (2018) Effects of VPA on reproductive endocrine function in male patients with epilepsy: a systematic review and metaanalysis. Epilepsy Behav 85:120–128
Rättyä J, Turkka J, Pakarinen AJ, Knip M, Kotila MA, Lukkarinen O et al (2001) Reproductive effects of VPA, carbamazepine, and oxcarbazepine in men with epilepsy. Neurology 56(1):31–36
Mikkonen K, Tapanainen P, Pakarinen AJ, Päivänsalo M, Isojärvi JI, Vainionpää LK (2004) Serum androgen levels and testicular structure during pubertal maturation in male subjects with epilepsy. Epilepsia 45(7):769–776
Hannan JL, Kutlu O, Stopak BL, Liu X, Castiglione F, Hedlund P et al (2014) Valproic acid prevents penile fibrosis and erectile dysfunction in cavernous nerve-injured rats. J Sex Med 11(6):1442–1451
Campbell J, Burnett A (2017) Neuroprotective and nerve regenerative approaches for treatment of erectile dysfunction after cavernous nerve injury. Int J Mol Sci 18(8):1794
Prins J, Blanker MH, Bohnen AM, Thomas S, Bosch JL (2002) Prevalence of erectile dysfunction: a systematic review of population-based studies. Int J Impot Res 14(6):422
Nikoobakht M, Motamedi M, Orandi A, Meysamie A, Emamzadeh A (2007) Sexual dysfunctiin epileptic men. Urol J 4(2):111–117
Calabrò RS, Gervasi G, Naro A, de Luca R, Marullo M, Bramanti P (2016) Erectile dysfunction in individuals with neurologic disability: a hospital-based cross-sectional study. Innov Clin Neurosci 13(1–2):10
Xiaotian X, Hengzhong Z, Yao X, Zhipan Z, Daoliang X, Yumei W (2013) Effects of antiepileptic drugs on reproductive endocrine function, sexual function and sperm parameters in Chinese Han men with epilepsy. J Clin Neurosci 20(11):1492–1497. https://doi.org/10.1016/j.jocn.2012.11.028. (Epub 2013 Aug 9 PMID: 23938015)
European Medicines Agency. Procedure under Article 31 of Directive 2001/83/EC resulting from pharmacovigilance data: substances related to valproate. Assessment report [Internet] [cited 2020 Jun]. https://www.ema.europa.eu/en/documents/referral/valproate-related-substances-article-31-referral-pracassessment-report_en.pdf
Roste LS, Tauboll E, Berner A, Berg KA, Aleksandersen M, Gjerstad L (2001) Morphological changes in the testis after long-term VPA treatment in male Wistar rats. Seizure 10(8):559–565
Bairy L, Paul V, Rao Y (2010) Reproductive toxicity of sodium valproate in male rats. Ind J Pharmacol 42(2):90
Gyllenborg J, Skakkebaek NE, Nielsen NC, Keiding N, Giwercman A (1999) Secular and seasonal changes in semen quality among young Danish men: a statistical analysis of semen samples from 1927 donor candidates during 1977–1995. Int J Androl 22(1):28–36. https://doi.org/10.1046/j.1365-2605.1999.00137.x. (PMID: 10068941)
Wu D, Chen L, Ji F, Si Y, Sun H (2018) The effects of oxcarbazepine, levetiracetam, and lamotrigine on semen quality, sexual function, and sex hormones in male adults with epilepsy. Epilepsia 59(7):1344–1350. https://doi.org/10.1111/epi.14450. (Epub 2018 Jun 11 PMID: 29889310)
Isojärvi JI, Löfgren E, Juntunen KS, Pakarinen AJ, Päivänsalo M, Rautakorpi I et al (2004) Effect of epilepsy and antiepileptic drugs on male reproductive health. Neurology 62(2):247–253
Duncan S, Blacklaw J, Beastall GH, Brodie MJ (1999) Antiepileptic drug therapy and sexual function in men with epilepsy. Epilepsia 40(2):197–204
Chen SS, Shen MR, Chen TJ, Lai SL (1992) Effects of antiepileptic drugs on sperm motility of normal controls and epileptic patients with long-term therapy. Epilepsia 33(1):149–153
Tallon E, O’Donovan L, Delanty N (2021) Reversible male infertility with valproate use: a review of the literature. Epilepsy Behav Rep 31(16):100446. https://doi.org/10.1016/j.ebr.2021.100446. (PMID: 34027381; PMCID: PMC8127004)
Ceylan M, Yalcin A, Bayraktutan OF, Karabulut I, Sonkaya AR (2016) Effects of levetiracetam monotherapy on sperm parameters and sex hormones: data from newly diagnosed patients with epilepsy. Seizure 41:70–74. https://doi.org/10.1016/j.seizure.2016.06.001. (Epub 2016 Jul 11 PMID: 27494618)
Sakai K, Hara K, Tanemura K (2023) Testicular histone hyperacetylation in mice by valproic acid administration affects the next generation by changes in sperm DNA methylation. PLoS ONE 18(3):e0282898. https://doi.org/10.1371/journal.pone.0282898. (PMID:36893188; PMCID:PMC9997898)
Choi CS, Gonzales EL, Kim KC, Yang SM, Kim JW, Mabunga DF, Cheong JH, Han SH, Bahn GH, Shin CY (2016) The transgenerational inheritance of autism-like phenotypes in mice exposed to valproic acid during pregnancy. Sci Rep 7(6):36250. https://doi.org/10.1038/srep36250. (PMID: 27819277; PMCID: PMC5098241)
Morris-Rosendahl DJ, Crocq MA (2020) Neurodevelopmental disorders-the history and future of a diagnostic concept. Dialogues Clin Neurosci 22(1):65–72. https://doi.org/10.31887/DCNS.2020.22.1/macrocq. (PMID: 32699506; PMCID: PMC7365295)
von Wrede R, Witt JA, Helmstaedter C (2023) Big data—big trouble: the two faces of publishing results from big data studies based on cohorts with poor clinical definition. Seizure 111:21–22. https://doi.org/10.1016/j.seizure.2023.07.015. (Epub 2023 Jul 21 PMID: 37490829)
Tomson T, Muraca G, Razaz N (2020) Paternal exposure to antiepileptic drugs and offspring outcomes: a nationwide population-based cohort study in Sweden. J Neurol Neurosurg Psychiatry 91(9):907–913. https://doi.org/10.1136/jnnp-2020-323028
Wensink M, Lu Y, Tian L, Jensen TK, Skakkebæk NE, Lindahl-Jacobsen R, Eisenberg M (2022) Nervous system drugs taken by future fathers and birth defects in offspring: a prospective registry-based cohort study. BMJ Open 12(3):e053946. https://doi.org/10.1136/bmjopen-2021-053946. (PMID: 35354621; PMCID: PMC8968542)
Engeland A et al (2013) Effects of preconceptional paternal drug exposure on birth outcomes’: cohort study of 340000 pregnancies using Norwegian population-based databases. Brit J Clin Pharmacol 75:1134–1141
Yang F, Yuan W, Liang H, Song X, Yu Y, Gelaye B, Miao M, Li J (2019) Preconceptional paternal antiepileptic drugs use and risk of congenital anomalies in offspring: a nationwide cohort study. Eur J Epidemiol 34(7):651–660. https://doi.org/10.1007/s10654-019-00509-2. (Epub 2019 Mar 13. PMID: 30868347)
Montgomery (Appellant) v Lanarkshire Health Board (Respondent) (Scotland). The Supreme Court. 2015. https://www.supremecourt.uk/cases/uksc-2013-0136.html accessed 27 Apr 2023
Bilal & Anor v St George’s University Hospital Trust [2023], EWCACiv604
McCulloch and others v Forth Valley Health Board [2023]
Angus-Leppan H, Moghim MM, Cock H, Kinton L, Synnott Wells M, Shankar R (2020) Valproate risk form-Surveying 215 clinicians involving 4775 encounters. Acta Neurol Scand 141(6):483–490. https://doi.org/10.1111/ane.13231. (Epub 2020 Mar 10 PMID: 32072612)
Tomson T, Battino D, Bonizzoni E, Craig J, Lindhout D, Perucca E, Sabers A, Thomas SV, Vajda F, EURAP Study Group (2016) Withdrawal of valproic acid treatment during pregnancy and seizure outcome: observations from EURAP. Epilepsia 57(8):e173–e177. https://doi.org/10.1111/epi.13437. (Epub 2016 Jun 20. PMID: 27319360)
Decision making and consent. General Medical Council. https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/decision-making-and-consent accessed 27 Apr 2023
Article 2 of the European Court of Human Rights (ECHR) Guide on Article 2 of the European Convention on Human Rights. https://www.echr.coe.int/documents/d/echr/Guide_Art_2_ENG#:~:text=Everyone's%20right%20to%20life%20shall,penalty%20is%20provided%20by%20law. August 2022, accessed Nov 2023
Black's Law Dictionary—Common law (10th ed.). 2014
Re MB [1997] EWCA Civ 3093
Arkell R. Women with epilepsy need choice, not diktats, when it comes to sodium valproate https://pharmaceutical-journal.com/article/opinion/women-with-epilepsy-need-choice-not-diktats-when-it-comes-to-sodium-valproate. 28 June 2023, accessed Jul 2023
Mothers and Babies: Reducing Risk through Audit and Confidential Enquiries. MBRRACE-UK Saving Lives Improving Mothers' Care - Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2019–21 https://www.npeu.ox.ac.uk/mbrrace-uk/reports, www.npeu.ox.ac.uk/mbrrace-uk/reports/confidential-enquiry-into-maternal-deaths]
Van McCrary S (2015) Commentary: revised recommendation from CMDh on use of valproate in women is ethically incomplete and neglects the interests of women. Epilepsia 56:1020–1022. https://doi.org/10.1111/epi.13043.26073405
Waddams F. BLOG 93: Valproate—don’t we deserve better? Epilepsy, Pregnancy, Motherhood & Me. 2022. https://fairyfaye1986.weebly.com/blog/blog-93-valproate-dont-we-deserve-better accessed 27 Apr 2023
Keddie S, Angus-Leppan H, Parker T, Toescu S, Nash A, Adewunmi O, Liu R (2016) Discussing sudden unexpected death in epilepsy: are we empowering our patients? A questionnaire survey. JRSM Open 7(9):2054270416654358. https://doi.org/10.1177/2054270416654358. (PMID: 27688898; PMCID: PMC5011309)
Robertson J, Hatton C, Emerson E, Baines S (2015) Prevalence of epilepsy among people with intellectual disabilities: a systematic review. Seizure 29:46–62. https://doi.org/10.1016/j.seizure.2015.03.016. (Epub 2015 Mar 30 PMID: 26076844)
McGrother CW, Bhaumik S, Thorp CF, Hauck A, Branford D, Watson JM (2006) Epilepsy in adults with intellectual disabilities: prevalence, associations and service implications. Seizure 15(6):376–386. https://doi.org/10.1016/j.seizure.2006.04.002. (Epub 2006 Jun 19 PMID: 16782360)
Shankar R, Rowe C, Van Hoorn A, Henley W, Laugharne R, Cox D, Pande R, Roy A, Sander JW (2018) Under representation of people with epilepsy and intellectual disability in research. PLoS ONE 13(6):e0198261. https://doi.org/10.1371/journal.pone.0198261
Bishop R, Laugharne R, Shaw N, Russell AM, Goodley D, Banerjee S, Clack E, SpeakUp CHAMPS, Shankar R (2024) The inclusion of adults with intellectual disabilities in health research—challenges, barriers and opportunities: a mixed-method study among stakeholders in England. J Intell Disability Res JIDR 68(2):140–149. https://doi.org/10.1111/jir.13097]
Sun JJ, Watkins L, Henley W, Laugharne R, Angus-Leppan H, Sawhney I, Shahidi MM, Purandare K, Eyeoyibo M, Scheepers M, Lines G, Winterhalder R, Perera B, Hyams B, Ashby S, Shankar R (2023) Mortality risk in adults with intellectual disabilities and epilepsy: an England and Wales case-control study. J Neurol 270(7):3527–3536. https://doi.org/10.1007/s00415-023-11701-6
Sun JJ, Perera B, Henley W, Angus-Leppan H, Sawhney I, Watkins L, Purandare KN, Eyeoyibo M, Scheepers M, Lines G, Winterhalder R, Ashby S, De Silva R, Miller J, Philpott DE, Ashwin C, Howkins J, Slater H, Medhurst D, Shankar R (2022) Epilepsy related multimorbidity, polypharmacy and risks in adults with intellectual disabilities: a national study. J Neurol 269(5):2750–2760. https://doi.org/10.1007/s00415-021-10938-3
Young C, Shankar R, Palmer J, Craig J, Hargreaves C, McLean B, Cox D, Hillier R (2015) Does intellectual disability increase sudden unexpected death in epilepsy (SUDEP) risk? Seizure 25:112–116. https://doi.org/10.1016/j.seizure.2014.10.001
Watkins LV, Linehan C, Brandt C, Snoeijen-Schouwenaars F, McGowan P, Shankar R (2022) Epilepsy in adults with neurodevelopmental disability—what every neurologist should know. Epileptic Disord 24(1):9–25. https://doi.org/10.1684/epd.2021.1366
Jackson CF, Makin SM, Marson AG, Kerr M (2015) Pharmacological interventions for epilepsy in people with intellectual disabilities. Cochrane Database Syst Rev 2015(9):C005399. https://doi.org/10.1002/14651858.CD005399.pub3. (PMID: 26333428; PMCID: PMC9216174)
Watkins L, O’Dwyer M, Kerr M, Scheepers M, Courtenay K, Shankar R (2020) Quality improvement in the management of people with epilepsy and intellectual disability: the development of clinical guidance. Expert Opin Pharmacother 21(2):173–181. https://doi.org/10.1080/14656566.2019.1695780
Snoeijen-Schouwenaars FM, Young C, Rowe C, van Ool JS, Schelhaas HJ, Shankar R (2021) People with epilepsy and intellectual disability: more than a sum of two conditions. Epilepsy & Behavior E&B 124:108355. https://doi.org/10.1016/j.yebeh.2021.108355. (Advance online publication)
Doran Z, Shankar R, Keezer MR, Dale C, McLean B, Kerr MP et al (2016) Managing anti-epileptic drug treatment in adult patients with intellectual disability: a serious conundrum. Eur J Neurol 23:1152–1157. https://doi.org/10.1111/ene.13016
Watkins LV, Henley W, Sun JJ, Perera B, Angus-Leppan H, Sawhney I, Purandare K, Eyeoyibo M, Scheepers M, Lines G, Winterhalder R, Shankar R (2022) Tackling increased risks in older adults with intellectual disability and epilepsy: data from a national multicentre cohort study. Seizure 101:15–21. https://doi.org/10.1016/j.seizure.2022.05.022
Gabrielsson A, Tromans S, Newman H, Triantafyllopoulou P, Hassiotis A, Bassett P, Watkins L, Sawhney I, Cooper M, Griffiths L, Pullen A, Roy A, Angus-Leppan H, Rh T, Kinney M, Tittensor P, Shankar R (2023) Awareness of social care needs in people with epilepsy and intellectual disability. Epilepsy Behav E&B 145:109296. https://doi.org/10.1016/j.yebeh.2023.109296
“The Top 300 of 2021”. ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.]. In 2021, the MHRA estimated there were ~20,000 females and ~ 50,000 males taking valproate in the UK
Malek N, Heath CA, Greene J (2017) A review of medication adherence in people with epilepsy. Acta Neurol Scand 135(5):507–515. https://doi.org/10.1111/ane.12703. (Epub 2016 Oct 26 PMID: 27781263)
Angus-Leppan H, Sperling MR, Villanueva V (2023) Antiseizure medications (antiepileptic drugs) in adults: starting, monitoring and stopping. J Neurol 270(1):573–581. https://doi.org/10.1007/s00415-022-11378-3. (Epub 2022 Sep 24 PMID: 36153467)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HAL gave evidence at MHRA meetings on valproate, at the Cumberlege hearings in 2019, and Sanofi Women and Epilepsy Education Board 2018. She has also received honoraria for non-pharmaceutical educational talks, as well as NIHR, Royal Free Charity, ncode funding, and Eisai and UCB investigator-initiated research grants. LW has Honoraria for work outside this project from Veriton Pharma. PNC is an unpaid member of the Council, Quality Committee and Epilepsy Advisory Group of the Association of British Neurologists, and a member of the Guidelines and Assessment Committee of the American Epilepsy Society. RS has received institutional and research support from LivaNova, UCB, Eisai, Veriton Pharma, Bial, Angelini, UnEEG and Jazz/GW pharma outside the submitted work. He holds grants from Innovate, NIHR AI, SBRI, ESPRC, ESRC and other funding bodies all outside this work. RA and DH have no Disclosures. The views of all authors are there own.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Angus-Leppan, H., Arkell, R., Watkins, L. et al. New valproate regulations, informed choice and seizure risk. J Neurol (2024). https://doi.org/10.1007/s00415-024-12436-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00415-024-12436-8