Abstract
Background and objectives
Observational studies have demonstrated a significant association between socio-economic status (SES) and Alzheimer's disease (AD). Nonetheless, the precise biological mechanisms underlying this association remain unclear. Therefore, we adopted a Mendelian Randomization (MR) approach to investigate the causal relationship between SES and genetic susceptibility to AD, as well as to explore the potential mediation effects of inflammation.
Methods
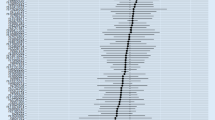
Large-scale cohorts based on publicly available genome-wide association study (GWAS) datasets from European populations were employed for conducting the MR study. The primary criterion utilized was the inverse-variance weighting (IVW) model. Heterogeneity and horizontal pleiotropy were assessed. In addition, multivariate MR (MVMR) was utilized to correct the confounders. Moreover, a two-step MR approach was used to evaluate the potential mediating effects of factors on the causal effects between SES and AD.
Results
As indicated by the results of the IVW model, educational years (OR = 0.708, 95% CI 0.610–0.821, P < 0.001) and household income (OR = 0.746, 95% CI 0.566–0.982, P = 0.037) was associated with a decreased genetic susceptibility risk for AD. The univariable results showed that the causal effect of educational years on the lower risk of AD remained significant (OR = 0.643, 95% CI 0.467–0.886, P = 0.006). In addition, our findings indicated that C-reactive protein (CRP) played a role in the causal effect of educational years on AD. The proportions of mediation were − 50.08% (95% CI − 92.78; − 7.38%).
Discussion
These findings provided evidence supporting the causal effect of educational attainment lower AD risk, with inflammation playing a mediating role. These findings may inform prevention strategies and interventions directed toward AD. Future studies should explore other plausible biological mechanisms.



Similar content being viewed by others
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. The dataset generated during and analysed during the current study are available from the MR Base database (http://www.mrbase.org/).
References
Jia L, Quan M, Fu Y et al (2020) Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol 19(1):81–92
Wang ZT, Fu Y, Zhang YR et al (2022) Modified dementia risk score as a tool for the prediction of dementia: a prospective cohort study of 239745 participants. Transl Psychiatry 12(1):509
Livingston G, Sommerlad A, Orgeta V et al (2017) Dementia prevention, intervention, and care. Lancet 390(10113):2673–2734
Frankish H, Horton R (2017) Prevention and management of dementia: a priority for public health. Lancet 390(10113):2614–2615
Yeung CHC, Au Yeung SL, Schooling CM (2022) Association of autoimmune diseases with Alzheimer’s disease: a mendelian randomization study. J Psychiatr Res 155:550–558
Zhang Y, Chen SD, Deng YT et al (2023) Identifying modifiable factors and their joint effect on dementia risk in the UK Biobank. Nat Hum Behav 7(7):1185–1195
Wu H, Yang J, Wang H, Li L (2023) Mendelian randomization to explore the direct or mediating associations between socioeconomic status and lung cancer. Front Oncol 13:1143059
Xu Q, Cai M, Ji Y et al (2023) Identifying the mediating role of socioeconomic status on the relationship between schizophrenia and major depressive disorder: a Mendelian randomisation analysis. Schizophrenia (Heidelb) 9(1):53
Deckers K, Cadar D, van Boxtel MPJ, Verhey FRJ, Steptoe A, Kohler S (2019) Modifiable risk factors explain socioeconomic inequalities in dementia risk: evidence from a population-based prospective cohort study. J Alzheimers Dis 71(2):549–557
Park D, Son KJ, Jeong E et al (2022) Effects of socioeconomic status and residence areas on long-term survival in patients with early-onset dementia: the Korean National Health Insurance Service Database Study. J Korean Med Sci 37(49):e354
Nong W, Mo G, Luo C (2023) Exploring the bidirectional causal link between household income status and genetic susceptibility to neurological diseases: findings from a Mendelian randomization study. Front Public Health 11:1202747
Seyedsalehi A, Warrier V, Bethlehem RAI, Perry BI, Burgess S, Murray GK (2023) Educational attainment, structural brain reserve and Alzheimer’s disease: a Mendelian randomization analysis. Brain 146(5):2059–2074
Wang AY, Hu HY, Ou YN et al (2023) Socioeconomic status and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 39 prospective studies. J Prev Alzheimers Dis 10(1):83–94
Kivipelto M, Mangialasche F, Ngandu T (2018) Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat Rev Neurol 14(11):653–666
Zavecz Z, Shah VD, Murillo OG et al (2023) NREM sleep as a novel protective cognitive reserve factor in the face of Alzheimer’s disease pathology. BMC Med 21(1):156
Stern Y, Arenaza-Urquijo EM, Bartres-Faz D et al (2020) Whitepaper: defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimers Dement 16(9):1305–1311
Gireesh A, Sacker A, McMunn A, Cadar D (2023) Role of inflammation in the socioeconomic inequalities of neurocognitive disorders. Brain Behav Immun 113:203–211
Hughes A, Kumari M, McMunn A, Bartley M (2017) Unemployment and inflammatory markers in England, Wales and Scotland, 1998–2012: meta-analysis of results from 12 studies. Brain Behav Immun 64:91–102
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey SG (2008) Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 27(8):1133–1163
Ioannidis JP, Haidich AB, Pappa M et al (2001) Comparison of evidence of treatment effects in randomized and nonrandomized studies. JAMA 286(7):821–830
Jin T, Huang W, Cao F et al (2022) Causal association between systemic lupus erythematosus and the risk of dementia: a Mendelian randomization study. Front Immunol 13:1063110
Goff DC Jr, Zaccaro DJ, Haffner SM, Saad MF, Insulin Resistance Atherosclerosis S (2003) Insulin sensitivity and the risk of incident hypertension: insights from the Insulin Resistance Atherosclerosis Study. Diabetes Care 26(3):805–809
Lee JJ, Wedow R, Okbay A et al (2018) Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nat Genet 50(8):1112–1121
Kunkle BW, Grenier-Boley B, Sims R et al (2019) Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Abeta, tau, immunity and lipid processing. Nat Genet 51(3):414–430
Meng L, Wang Z, Ming YC, Shen L, Ji HF (2022) Are micronutrient levels and supplements causally associated with the risk of Alzheimer’s disease? A two-sample Mendelian randomization analysis. Food Funct 13(12):6665–6673
Sanderson E, Spiller W, Bowden J (2021) Testing and correcting for weak and pleiotropic instruments in two-sample multivariable Mendelian randomization. Stat Med 40(25):5434–5452
Burgess S, Thompson SG, Collaboration CCG (2011) Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol 40(3):755–764
Burgess S, Butterworth A, Thompson SG (2013) Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 37(7):658–665
Bowden J, Davey Smith G, Haycock PC, Burgess S (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314
Bowden J (2017) Misconceptions on the use of MR-Egger regression and the evaluation of the InSIDE assumption. Int J Epidemiol 46(6):2097–2099
Nguyen LT, Schmidt HA, von Haeseler A, Minh BQ (2015) IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol Biol Evol 32(1):268–274
Verbanck M, Chen CY, Neale B, Do R (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 50(5):693–698
Liu Z, Wang H, Yang Z, Lu Y, Zou C (2023) Causal associations between type 1 diabetes mellitus and cardiovascular diseases: a Mendelian randomization study. Cardiovasc Diabetol 22(1):236
Hemani G, Zheng J, Elsworth B et al (2018) The MR-Base platform supports systematic causal inference across the human phenome. Elife 7:e34408
Stephan BCM, Siervo M, Brayne C (2020) How can population-based studies best be utilized to reduce the global impact of dementia? Recommendations for researchers, funders, and policymakers. Alzheimers Dement 16(10):1448–1456
Hackman DA, Farah MJ, Meaney MJ (2010) Socioeconomic status and the brain: mechanistic insights from human and animal research. Nat Rev Neurosci 11(9):651–659
Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimaki M, Batty GD (2013) Socioeconomic status as a risk factor for dementia death: individual participant meta-analysis of 86 508 men and women from the UK. Br J Psychiatry 203(1):10–17
Petersen JD, Wehberg S, Packness A et al (2021) Association of socioeconomic status with dementia diagnosis among older adults in Denmark. JAMA Netw Open 4(5):e2110432
Cadar D, Lassale C, Davies H, Llewellyn DJ, Batty GD, Steptoe A (2018) Individual and area-based socioeconomic factors associated with dementia incidence in England: evidence from a 12-year follow-up in the English Longitudinal Study of Ageing. JAMA Psychiat 75(7):723–732
Soh Y, Whitmer RA, Mayeda ER et al (2023) State-level indicators of childhood educational quality and incident dementia in older black and white adults. JAMA Neurol 80(4):352–359
Marden JR, Tchetgen Tchetgen EJ, Kawachi I, Glymour MM (2017) Contribution of socioeconomic status at 3 life-course periods to late-life memory function and decline: early and late predictors of dementia risk. Am J Epidemiol 186(7):805–814
Meyer OL, Mungas D, King J et al (2018) Neighborhood socioeconomic status and cognitive trajectories in a diverse longitudinal cohort. Clin Gerontol 41(1):82–93
Trani JF, Moodley J, Maw MTT, Babulal GM (2022) Association of multidimensional poverty with dementia in adults aged 50 years or older in South Africa. JAMA Netw Open 5(3):e224160
Wang RZ, Yang YX, Li HQ et al (2021) Genetically determined low income modifies Alzheimer’s disease risk. Ann Transl Med 9(15):1222
Farah MJ (2018) Socioeconomic status and the brain: prospects for neuroscience-informed policy. Nat Rev Neurosci 19(7):428–438
Tang J, Chen A, He F et al (2023) Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China. Environ Res 223:115048
Zhang Y, Yang H, Li S, Li WD, Wang Y (2021) Consumption of coffee and tea and risk of developing stroke, dementia, and poststroke dementia: a cohort study in the UK Biobank. PLoS Med 18(11):e1003830
Marshall IJ, Wang Y, Crichton S, McKevitt C, Rudd AG, Wolfe CD (2015) The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol 14(12):1206–1218
Letellier N, Ilango SD, Mortamais M et al (2021) Socioeconomic inequalities in dementia risk among a French population-based cohort: quantifying the role of cardiovascular health and vascular events. Eur J Epidemiol 36(10):1015–1023
Lai KY, Webster C, Kumari S, Gallacher JEJ, Sarkar C (2023) The associations of socioeconomic status with incident dementia and Alzheimer’s disease are modified by leucocyte telomere length: a population-based cohort study. Sci Rep 13(1):6163
Lazar M, Davenport L (2018) Barriers to health care access for low income families: a review of literature. J Community Health Nurs 35(1):28–37
Bennett JM, Reeves G, Billman GE, Sturmberg JP (2018) Inflammation-nature’s way to efficiently respond to all types of challenges: implications for understanding and managing “the epidemic” of chronic diseases. Front Med (Lausanne) 5:316
Haroon E, Raison CL, Miller AH (2012) Psychoneuroimmunology meets neuropsychopharmacology: translational implications of the impact of inflammation on behavior. Neuropsychopharmacology 37(1):137–162
Emdin CA, Khera AV, Kathiresan S (2017) Mendelian randomization. JAMA 318(19):1925–1926
Cao J, Wang Z, Zhu M, Huang Y, Jin Z, Xiong Z (2023) Low-density lipoprotein cholesterol and risk of hepatocellular carcinoma: a Mendelian randomization and mediation analysis. Lipids Health Dis 22(1):110
Acknowledgements
We are grateful to the many participants and researchers for collecting, contributing to the GWAS dataset, and making their GWAS summary statistics publicly available.
Funding
This work was supported by the National Key Research and Development Program of China (2022YFC3602600), National Natural Science Foundation of China (82220108009, 81970996), and STI2030-Major Projects (2021ZD0201801).
Author information
Authors and Affiliations
Contributions
CG and KM study concept, design, software, and paper writing. KM data curation and software. YT dissertation revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no interest.
Ethical approval
Since all analyses were based on publicly available summary statistics, no patients were involved in the design of the study, and no ethical approval from an institutional review board was required.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geng, C., Meng, K. & Tang, Y. Identifying the mediating role of inflammation on the relationship between socioeconomic status and Alzheimer’s disease: a Mendelian randomization analysis and mediation analysis. J Neurol 271, 2484–2493 (2024). https://doi.org/10.1007/s00415-023-12176-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-12176-1