Abstract
Introduction
Nystagmus is a valuable clinical finding. Although nystagmus is often described by the direction of its quick phases, it is the slow phase that reflects the underlying disorder. The aim of our study was to describe a new radiological diagnostic sign called “Vestibular Eye Sign”—VES. This sign is defined as an eye deviation that correlates with the slow phase of nystagmus (vestibule pathological side), which is seen in acute vestibular neuronitis and can be assessed on a CT head scan.
Materials and methods
A total of 1250 patients were diagnosed with vertigo in the Emergency Department at Ziv Medical Center (ED) in Safed, Israel. The data of 315 patients who arrived at the ED between January 2010 and January 2022 were collected, with criteria eligible for the study. Patients were divided into 4 groups: Group A, “pure VN”, Group B, “non-VN aetiology”, Group C, BPPV patients, and Group D, patients who had a diagnosis of vertigo with unknown aetiology. All groups underwent head CT examination while in the ED.
Results
In Group 1, pure vestibular neuritis was diagnosed in 70 (22.2%) patients. Regarding accuracy, VES (Vestibular Eye Sign) was found in 65 patients in group 1 and 8 patients in group 2 and had a sensitivity of 89%, specificity of 75% and a negative predictive value of 99.4% in group 1—pure vestibular neuronitis.
Conclusion
VN is still a clinical diagnosis, but if the patient undergoes head CT, we suggest using the “Vestibular Eye Sign” as a complementary sign. As per our findings, this is a valuable sign on CT imaging for diagnosing the pathological side of isolated pure VN. It is sensitive to support a diagnosis with a high negative predictive value.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nystagmus is a valuable clinical finding and it may be defined as a rhythmic, involuntary, rapid, oscillatory movement of the eyes [1]. Peripheral nystagmus can have two phases: slow and fast, or a combination of the two. The fast phase of nystagmus is normally directed away from the side of a destructive lesion, the slow phase sends the eye away from the preferred direction of gaze, and the corrective quick phase (a saccade) returns the eye to the visual target in a peripheral vestibular lesion. Although the fast stages of nystagmus are generally identified by their orientation, the slow phase is what reveals the underlying problem [2].
Peripheral nystagmus is transient, it is always due to unilateral, or if bilateral then asymmetrical, vestibular disease or stimulation. It is always suppressed by visual fixation. Failure of fixation suppression indicates cerebellar disease [3].
Nystagmus with central vertigo, on the other hand, is more likely to appear as “alternating” direction-changing nystagmus. When the patient looks to the right, the nystagmus will be rightward, and when the patient looks to the left, the nystagmus will be leftward [4].
It can be difficult for clinicians to appropriately categorize the nystagmus phase at times. Seeing the patient's eyes move swiftly in real time and determining which side is pathogenic and which is etiological might be difficult. In patients with acute vertigo, detecting nystagmus is a crucial diagnostic signal. Patients with peripheral abnormalities have a continuous direction of nystagmus, whereas those with central disorders have nystagmus that changes direction with or without gaze fixation [5].
Misdiagnosis of common peripheral vestibular disorders such as benign paroxysmal positional vertigo (BPPV) and vestibular neuritis results in inefficient therapy and resource overuse [6].
Over 90% of all vertigo causes are caused by peripheral vertigo. Ischemia of the central vestibular structures in the cerebellum, brainstem, or vestibular nuclei is the most prevalent cause of central vertigo, especially in elderly individuals with vascular risk factors. In younger individuals, acute demyelination, such as that seen in multiple sclerosis, is another rather prevalent cause of central vertigo [7]. Cerebellar haemorrhage, thiamine deficiency, and numerous autoimmune, viral, or metabolic conditions [8, 9] are all rare causes of isolated acute vestibular syndrome (AVS).
Vestibular neuritis (VN) is a condition that causes vertigo, nausea, and gait instability. It is hypothesized to be caused by inflammation of the vestibular component of the eighth cranial nerve. It is a harmless, self-limiting disease that usually lasts a few days, but it can take weeks or months for all vestibular symptoms to disappear [10]. This is a clinical diagnosis, and it is up to the physician to tell the difference between this benign self-limiting condition and other central nervous system causes, such as cerebrovascular syndromes [11].
However, because of the significant underlying aetiology of brainstem ischemia or infarction [5], the clinical diagnosis of central vertigo is critical. VN is a diagnosis of exclusion based on clinical, laboratory, and radiographic evaluations [12] because there are no confirmatory diagnostic tests. Even if a patient shows the typical pattern of spontaneous nystagmus seen in vestibular neuritis, brain imaging should be considered if the patient has an unusual headache, a negative head impulse test, severe unsteadiness, or no improvement after 1–2 days [13].
Guarnizo et al. [14] concluded that both non-contrast computed tomography and computerized tomography angiograms of the head and neck have low diagnostic yield for the detection of central causes of dizziness. However, they suggested that more research be done to determine the role of computerized tomography in the work-up of patients with isolated dizziness in the emergency department.
Vestibular Eye Sign (VES) is seen in head CT as an eye deviation in a horizontal gaze toward the affected vestibule, and it has never been mentioned in predicting the affected side of the vestibulopathy.
The aim of our study was to describe a new radiological diagnostic sign in vestibular neuronitis known as the "Vestibular Eye Sign" (VES).
Patients and methods
Patients
This study was a retrospective review of study patients who were diagnosed with vertigo and already have undergone CT in the ED in Ziv Medical Center between January 2010 and January 2022.
Both the study protocol and the use of data were approved by the Helsinki Committee of the Medical Center.
Inclusion and exclusion criteria
Exclusion criteria
Patients with reports of unilateral hearing loss, history of external or middle ear problems, history of inner ear surgery, ototoxic drug intake, previous neurologic disorders, incomplete clinical data, and with a known aetiology, including trauma, prior eye globe deviation, migraine, and Meniere disease, were excluded from the study.
Inclusion criteria
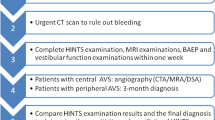
Patients were divided into 4 groups (1 + 2 with spontaneous nystagmus 3 + 4 with no spontaneous nystagmus) (Fig. 1).
Group 1 “pure VN “: The diagnosis of Group 1—“Pure vestibular neuronitis” was based on the diagnostic criteria of Acute Unilateral Vestibulopathy according to the Bárány Society Classification of Vestibular Disorders [14] (Table 1).
Group 2 “non-VN aetiology”: those patients who were suspected to have VN but the diagnosis was ruled out in follow-up and had neurologic symptoms such as weakness, vision or hearing changes, altered level of consciousness, truncal ataxia, transient or vertical nystagmus, cranial nerve deficits or other changes in sensory and motor function favouring the presence of a central cause of vertigo such as cerebrovascular disease, neoplasm, multiple sclerosis or B12 deficiency Patients who had an MRI scan with neurological follow-up were included as an isolated group in the study named “Non-VN cause”.
Group 3 patients who were diagnosed with benign paroxysmal positional vertigo (BPPV) who had head CT while in the ED with no central cause, with no spontaneous nystagmus.
Group 4 patients who had a “vertigo” diagnosis in the ED and underwent head CT while in the ED with both normal otolaryngologic and neurological evaluation, with no spontaneous nystagmus.
All of the participants were subjected to history taking and otoscopy and complete neuro-otologic examination, including bedside vestibular examination, to differentiate peripheral versus central vestibular lesions. Groups 1 and 2 underwent cranial MRI with gadolinium enhancement.
The control group was formed from Groups 3 and 4 (with no spontaneous nystagmus).
Methods
CT diagnosis criteria of the vestibular eye SIGN
CT scans of 315 serial patients presenting with symptoms of acute vertigo were reviewed.
Axial head scans were acquired with CT scanners with the slices parallel to the inferior orbitomeatal line or orbitomeatal line and slice thickness of no more than 6 mm through the orbit.
No instructions were given to the patients regarding eye closure or gaze during the scan, but the 3D reconstruction revealed that the pure vestibular neuritis group (Group 1) had closed eyes.
Three raters blinded to all clinical information independently assessed the orbits and the data were collected and interpreted by a neuroradiologist.
Scans were classified as showing rightward globe, leftward globe, or undeviated indeterminate globe. Indeterminate scans were those where the axes were not visible. If there was movement of the ocular axes across the midline between slices, the scans were classified as undeviated (Fig. 2).
The authors determined the horizontal deviation of eye-in-head position by the using the angle created by the ocular axis's junction with the “line of sight” greatest fit' through the head's midline structures (Fig. 3).
The researcher who carried out the measurements was blinded to the clinical signs of the patient. Horizontal deviations in the direction of positive values were classified on the ipsilesional side, whereas deviations to the contralesional values on the negative side. The values of the right and left eye deviations averaged for every person.
The raters were not given any instructions as to what degree of deviation constituted each of the gaze categories.
Independent measurement quantified the degree of eye deviation and gave an estimate of the threshold at which interpreters typically differentiated between deviated and undeviated eyes.
Consensus ratings (agreement of two out of three raters) and kappa statistics for interobserver agreement were calculated.
Vestibular lesion location was determined by clinical information with fast- and slow-phase nystagmus, which were noted in the patient examination and diagnosis.
The probability that eye deviation correctly predicted the pathological vestibular side was calculated.
Statistical analysis
Data were analysed using SPSS version 25 (SPSS Inc. Chicago, IL, USA).
All continuous variables are presented as the mean and standard deviation, while all categorical variables are presented as frequencies and percentages.
The 2 × 2 contingency table was formulated to determine the sensitivity, specificity, positive predictive value, and negative predictive value of the “Vestibular Eye Sign” in head CT taking clinical findings and normal MRI as the gold standard.
Results
We identified 1250 patients diagnosed with vertigo during the study period, of whom 315 fit the inclusion criteria. Of the 315 patients, 70 were in group 1, 45 were in group 2, 100 were in group 3 and 100 were in group 4. The mean patient age was 47.2 ± 17.5 years in group 1 and 65.2 ± 12.6 years in group 2, and the mean age was 64.75 ± 9.5 years in group 3 and 55.4 ± 10.3 years in group 4.
There were 187 (59.3%) female and 128 (40.7%) male patients.
VES was found in 65 patients in the pure VN group and 8 patients in the non-VN group and was not found in groups 3 and 4 (Fig. 4).
VES was found to have a sensitivity of 89%, specificity of 75%, positive predictive value of 15% and negative predictive value of 99.4% in group A—pure vestibular neuronitis (Table 2).
The diagnostic data of VES in diagnosing pure vestibular neuritis compared to non-VN groups are shown in Table 3.
The side of the eye deviation of the VES was not significantly different in groups A and B (Table 4).
Discussion
Based on the results of this study and the literature, we recommend using the "Vestibular Eye Sign" in conjunction with clinical data to diagnose acute vestibular neuronitis. This is a useful indicator on CT imaging for diagnosing the pathogenic side of isolated pure VN, according to our findings. It has a sensitivity of 89% and a specificity of 75%, as well as the potential to have a high negative predictive value of 99.4%.
Our study results confirm the importance of VN as a clinical diagnosis.
This is not the first time "Vestibular Eye Sign" has been described in the medical literature as a radiological sign for acute VN [15], but it has never been mentioned in predicting the affected side of the vestibulopathy.
If the clinical diagnosis is very probable for VN, the VES is sensitive in predicting the affected side of the vestibulopathy and in confirming this diagnosis, but if it was not found, the clinician should be doubtful and more open to other diagnoses despite the fact that the VES does not rule out VN.
We emphasize the fact that inappropriate CT usage can disclose incidental abnormalities that compromise the validity of the diagnosis and prompt useless, pointless, and even dangerous follow-up tests [16].
After a CT was performed, we evaluated our patients retrospectively and there was ocular lateral deviation.
The patient should next be examined to identify the side that is likely impacted by vestibular neuritis; however, according to our results and based on other articles, some individuals may have actually experienced a lateral medullary stroke [17, 18] or even a hemisphere stroke [19].
The clinical syndrome of sudden spontaneous vertigo (for several days) without any other neurologic or audiologic symptoms or signs is usually attributed to vestibular neuritis (VN) [20, 21], which is caused by viral or post-viral inflammation of the vestibular nerve.
Cerebellar stroke [22], also known as pseudo-VN, causes comparable clinical symptoms and findings. A cerebellar infarction linked with pseudo-VN can be readily missed on a CT scan [23].
Lee et al. [24] concluded that cerebellar infarction mimicking vestibular neuritis is more common than previously assumed and that early diagnosis and recognition of this indication is critical.
According to a large prospective study, approximately 11% of patients with isolated cerebellar infarctions experience isolated vertigo, and the majority of them (96%) had an infarct in the region of the medial branch of the PICA, which includes the nodulus [25].
Ischemia of the lateral medulla, which includes the vestibular nucleus, may be a prevalent source of isolated vascular vertigo since the vestibular nucleus is more sensitive to ischemia than other structures in the brainstem and cerebellum. Isolated vertigo can also be caused by lesions involving the flocculus or dorsal insular cortex [26].
Eye deviation on admission was related to substantial "anterior" circulation and more severe neurological impairments, according to S. Payabvash et al. [27].
In patients with acute unilateral cerebellar lesions, gaze-evoked nystagmus (GEN) may not only be a diagnostic indicator in patients with brainstem lesions but also signal to ipsilesionally localized destruction of midline and lower cerebellar structures [28], according to a study.
Vestibular strokes are frequently misdiagnosed due to clinical symptoms that resemble benign ear diseases. Because over 95% of ED dizziness patients do not have a stroke, diagnosing these cerebrovascular instances is extremely difficult.
Neuroimaging appears to be a natural answer; however, CT seems ineffective, and MRI is imperfect and too expensive to use on all patients who go to the ED with vertigo. This puts a premium on precise bedside diagnosis [29].
The following literature study can explain the meaning of the "Vestibular Eye Sign":
-
A-
Eye deviation seen on CT scans seems to occur more frequently than what is seen during a clinical evaluation. This is possibly because fixation is removed when most patients close their eyes during CT scanning.
-
B-
In the absence of any nystagmus in the light, the appearance of a unidirectional nystagmus with eye closure or in darkness, or an increase of nystagmus present in the light by eye closure or in darkness [30].
-
C-
Because the patient has less time to move during the acquisition, fast scanners reduce motion artifacts. Faster rotation or more X-ray sources could help achieve this [31].
Our study limitations were that it was a retrospective, the use of a single-centre study, and the lack of a quantitative definition for eye deviation observed on admission CT. In addition, given that only the consensus interpretations of CT images were available in the trials public dataset, the interrater agreement cannot be determined; however, prior studies have reported an excellent interrater agreement for the determination of radiological eye deviation with a Kappa coefficient of 0.8.
Our study strengths were that only two prior researches on this specific topic [15, 32] and it is a new research typology.
In this case, discovering the limitations can be considered an important opportunity to present the need for further development in this area of study.
The use of a radiological "Vestibular Eye Sign" to distinguish posterior circulation stroke from vestibular neuritis has never been reported in the literature, but the goal of this research is to first describe this sign in the peripheral VN and then compare it to posterior circulation stroke in a separate study.
Conclusion
Vestibular neuronitis is still a clinical diagnosis, but if the patient undergoes a head CT, we suggest using the “Vestibular Eye Sign” as a complimentary sign and may aid in the localization of the affected vestibular side. As per our findings, this sign is a valuable sign on CT imaging for the diagnosis of the pathological side of isolated pure VN. It is a sensitive sign with high negative predictive value.
References
Eggers S, Bisdorff A, von Brevern M, Zee D, Kim J, Perez-Fernandez N et al (2019) Classification of vestibular signs and examination techniques: nystagmus and nystagmus-like movements. J Vestib Res 29(2–3):57–87. https://doi.org/10.3233/ves-190658
Crane BT, Tian J, Demer JL (2000) Asymmetry of ocular motor and perceptual vestibular processing in humans with unilateral vestibular deafferentation. J Vestib Res 10(6):259–269
Halmagyi GM, McGarvie LA, Strupp M (2020) Nystagmus goggles: how to use them, what you find and what it means. Pract Neurol 20(6):446–450. https://doi.org/10.1136/practneurol-2020-002513
Sekhon RK, Rocha Cabrero F, Deibel JP (2021) Nystagmus Types. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539711/. Accessed 9 Nov 2020
Huh Y, Kim J (2013) Bedside evaluation of dizzy patients. J Clin Neurol 9(4):203. https://doi.org/10.3988/jcn.2013.9.4.203
Newman-Toker DE, Camargo CA Jr, Hsieh YH, Pelletier AJ, Edlow JA (2009) Disconnect between charted vestibular diagnoses and emergency department management decisions: a cross-sectional analysis from a nationally representative sample. Acad Emerg Med 16(10):970–977
Lui F, Foris LA, Willner K et al (2023) Central Vertigo. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441861/. Accessed 22 Dec 2022
Edlow JA, Newman-Toker DE (2015) Medical and nonstroke neurologic causes of acute, continuous vestibular symptoms. Neurol Clin 33(3):699–716 (xi)
Kattah JC, Dhanani SS, Pula JH, Mantokoudis G, Saber Tehrani AS, Newman-Toker D (2013) Vestibular signs of thiamine deficiency during the early phase of suspected Wernicke encephalopathy. Neurol Clin Pract 3:260–468
Solis R, Sun D, Tatro E, Hansen M (2018) Do steroids improve recovery in vestibular neuritis? Laryngoscope 129(2):288–290. https://doi.org/10.1002/lary.27278
Johns P, Quinn J (2020) Clinical diagnosis of benign paroxysmal positional vertigo and vestibular neuritis. Can Med Assoc J 192(8):E182–E186. https://doi.org/10.1503/cmaj.190334
Kim J (2020) When the room is spinning: experience of vestibular neuritis by a neurotologist. Front Neurol. https://doi.org/10.3389/fneur.2020.00157
Jeong S-H, Kim H-J, Kim J-S (2013) Vestibular neuritis. Semin Neurol 33(03):185–194
Guarnizo A, Farah K, Lelli D, Tse D, Zakhari N (2021) Limited usefulness of routine head and neck CT angiogram in the imaging assessment of dizziness in the emergency department. Neuroradiol J 34(4):335–340. https://doi.org/10.1177/1971400920988665
Yang YJ, Kim KW, Choi JE, Lee MY, Yoo DS, Jung JY (2018) Prediction of vestibular imbalance in acute peripheral vestibulopathy by measuring horizontal ocular deviation on magnetic resonance imaging. Otol Neurotol 39:e108–e112 (pmid:29194214)
Saro-Buendía M, Torres-García L, Angel NJ, Acosta RM, Guijo JC, Díaz CB, Piñero AG, Pérez-Guillén V, Carceller MA (2023) Dizziness evaluation and characterisation of patients with posterior circulation stroke in the emergency department; a case series study. Arch Acad Emerg Med. 11(1):e12. https://doi.org/10.22037/aaem.v11i1.1764. (PMID: 36620730; PMCID: PMC9807946)
Kattah JC, Pula J, Newman-Toker DE (2011) Ocular lateropulsion as a central oculomotor sign in acute vestibular syndrome is not posturally dependent. Ann N Y Acad Sci 1233:249–255. https://doi.org/10.1111/j.1749-6632.2011.06160.x
Kattah JC, Badihian S, Pula JH, Tarnutzer AA, Newman-Toker DE, Zee DS (2020) Ocular lateral deviation with brief removal of visual fixation differentiates central from peripheral vestibular syndrome. J Neurol 267(12):3763–3772. https://doi.org/10.1007/s00415-020-10100
Lesley WS, Rangaswamy R, Smith KH, Watkins DM (2009) Predicting acute ischemic stroke by measuring the degree of ocular gaze deviation (Prevost’s sign) on CT. J Neurointerv Surg 1(1):32–34. https://doi.org/10.1136/jnis.2009.000281
Strupp M, Magnusson M (2015) Acute unilateral vestibulopathy. Neurol Clin 33(3):669–685. https://doi.org/10.1016/j.ncl.2015.04.012
Baloh RW (2003) Vestibular neuritis. N Engl J Med 348:1027–1032
Hotson JR, Baloh RW (1998) Acute vestibular syndrome. N Engl J Med 339:680–685
Simmons Z, Biller J, Adams HP, Dunn V, Jacoby CG (1986) Cerebellar infarction: comparison of computed tomography and magnetic resonance imaging. Ann Neurol 19:291–293
Lee H, Sohn S, Cho Y, Lee S, Ahn B, Park B, Baloh R (2006) Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology 67(7):1178–1183. https://doi.org/10.1212/01.wnl.0000238500.02302.b4
Lee H, Sohn SI, Cho YW, Lee SR, Ahn BH, Park BR et al (2006) Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns. Neurology 67:1178–1183
Lee H (2014) Isolated vascular vertigo. J Stroke 16(3):124. https://doi.org/10.5853/jos.2014.16.3.124
Payabvash S, Qureshi I, Qureshi A (2016) Clinical implications of eye deviation on admission CT examination of acute ischaemic stroke patients. Clin Radiol 71(12):1314.e11-1314.e15. https://doi.org/10.1016/j.crad.2016.08.002
Baier B, Dieterich M (2011) Incidence and anatomy of gaze-evoked nystagmus in patients with cerebellar lesions. Neurology 76(4):361–365. https://doi.org/10.1212/wnl.0b013e318208f4c3
Saber Tehrani A, Kattah J, Kerber K, Gold D, Zee D, Urrutia V, Newman-Toker D (2018) Diagnosing stroke in acute dizziness and vertigo. Stroke 49(3):788–795. https://doi.org/10.1161/strokeaha.117.016979
Korres S (1978) Electronystagmographic criteria in neuro-otological diagnosis. 1. 366 Peripheral lesions. J Neurol Neurosurg Psychiatry 41(3):249–253. https://doi.org/10.1136/jnnp.41.3.249. (367)
Yan Z et al (2014) Analysis and solutions of artifacts on multi-slice spiral CT images. In: The proceedings of the 2nd international conference on industrial application engineering 2014 [Preprint]. https://doi.org/10.12792/iciae2014.009
Yang Y-J et al (2019) Measurement of horizontal ocular deviation on magnetic resonance imaging in various disease with acute vertigo. PLoS ONE 14(10):e0224605
Acknowledgements
We would like to thank the entire department of Otolaryngology head and neck surgery, Neurology and Radiology Departments in Ziv Medical Center for their help and support.
Author information
Authors and Affiliations
Contributions
Conceptualization: RF, SM. Data curation: RF, AAA. Formal analysis: RF, WAS, DA. Investigation: RF, SM, WAS, DA. Radiological revision and analysis: RN, SM, RF. Supervision: SM. Validation: SM, YA, AAA. Visualization: RF, RN, SM. Writing-original draft: RF. Writing-review & editing: RF, SM.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standard
This study was a retrospective review of study patients who were diagnosed with vertigo and already have undergone CT in the ED in Ziv Medical Center between January 2010 and January 2022. Both the study protocol and the use of data were approved by the Helsinki Committee of the Medical Center.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farhat, R., Awad, A.A., Shaheen, W.A. et al. The “Vestibular Eye Sign”—“VES”: a new radiological sign of vestibular neuronitis can help to determine the affected vestibule and support the diagnosis. J Neurol 270, 4360–4367 (2023). https://doi.org/10.1007/s00415-023-11771-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11771-6