Abstract
Background and objective
Despite olfactory disorders being among the most common neurological complications of coronavirus disease 2019 (COVID-19), their pathogenesis has not been fully elucidated yet. Brain MR imaging is a consolidated method for evaluating olfactory system’s morphological modification, but a few quantitative studies have been published so far. The aim of the study was to provide MRI evidence of olfactory system alterations in patients with COVID-19 and neurological symptoms, including olfactory dysfunction.
Methods
196 COVID-19 patients (median age: 53 years, 56% females) and 39 controls (median age 55 years, 49% females) were included in this cross-sectional observational study; 78 of the patients reported olfactory loss as the only neurological symptom. MRI processing was performed by ad-hoc semi-automatic processing procedures. Olfactory bulb (OB) volume was measured on T2-weighted MRI based on manual tracing and normalized to the brain volume. Olfactory tract (OT) median signal intensity was quantified on fluid attenuated inversion recovery (FLAIR) sequences, after preliminary intensity normalization.
Results
COVID-19 patients showed significantly lower left, right and total OB volumes than controls (p < 0.05). Age-related OB atrophy was found in the control but not in the patient population. No significant difference was found between patients with olfactory disorders and other neurological symptoms. Several outliers with abnormally high OT FLAIR signal intensity were found in the patient group.
Conclusions
Brain MRI findings demonstrated OB damage in COVID-19 patients with neurological complications. Future longitudinal studies are needed to clarify the transient or permanent nature of OB atrophy in COVID-19 pathology.
Graphical abstract

Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing the coronavirus disease 2019 (COVID-19), initiated a worldwide pandemic that, as of February 2022, has resulted in more than 430 billion confirmed cases and about 5.9 million deaths worldwide [1].
The most common manifestations of COVID-19 are pulmonary in nature, but a number of neurological complications, including smell and taste disorders, cranial nerve deficits, polyneuropathies, cerebrovascular disorders, encephalopathies and inflammatory central nervous system (CNS) syndromes, headache, and seizures, have been increasingly reported [2]. COVID-19 neurological complications are expected to be associated with the suspected neuroinvasive potential of human coronaviruses (CoVs) [3, 4].
A large body of evidence has demonstrated that the total loss or a reduced sense of smell (anosmia and hyposmia, respectively) are the most common neurological complications of COVID-19 [4, 5], especially occurring in otherwise asymptomatic subjects and in early phases of the disease [6]. In spite of the high incidence of olfactory dysfunction (OD) in COVID-19 [7], its underlying mechanism has not been fully elucidated, yet. Nasal and oropharyngeal cavities are considered the possible gateways for many viral pathogens, including SARS-CoV-2. However, unlike other post viral olfactory dysfunctions, COVID-19-related anosmia and hyposmia are not correlated with nasal obstruction or rhinitis, suggesting that they may be rather associated with the neurotropism of the virus. The widespread angiotensin-converting enzyme 2 (ACE2) expression in the brain and in the olfactory bulbs makes them a potential target of COVID-19 and supports the hypothesis of neuroinvasion through the olfactory system [4].
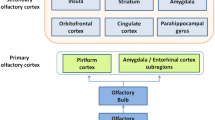
The olfactory system, mediating the sense of smell, is phylogenetically one of the most primitive sensory systems. Olfaction is conveyed by the first cranial nerve (CN I), which originates in the olfactory neuroepithelium, located in the posterosuperior portion of each nasal cavity (olfactory cleft). The epithelium includes the somas of the bipolar olfactory neurons, which are both receptors and neurons of the first order of the olfactory pathway. These represent the origin of the olfactory nerve fibers, and they have the unique ability to regenerate thanks to the stem cells located in the epithelium. The dendrites of the olfactory neurons directly project to the surface of the epithelium, so as to bind to the odorant molecules that reach the nasal cavity. This exposure of the dendrites to the external environment is well-known to be exploited by many viruses, including the Coronaviruses, as a gateway to the central nervous system by retrograde axonal transport [8, 9].
The axons of the first order olfactory nerves group together in the form of small nerve bundles (fila olfactoria) and pass through the small foramina of the cribriform plate of the ethmoid bone, entering the olfactory bulbs through their ventral surface. The olfactory bulb (OB) is a bilateral, elliptical, ventrodorsally-oriented extension of the telencephalon. It represents the primary center of the olfactory system, serving as a relay station for the impulses coming from the epithelium and bound for the olfactory cortex. The olfactory tract (OT) is a thin, myelinated nervous projection that, from the OB, runs posteriorly ending in perforate substance [8].
Brain MR imaging is a useful and consolidated method for evaluating olfactory dysfunction (OD) [10, 11]. Nonetheless, to our knowledge, MRI-based evaluations of olfactory system alterations associated with COVID-19 are still limited to small investigational studies, case series, and case reports [12,13,14,15,16,17,18]. Only a few studies performing systematic, quantitative olfactory system measurements have been published so far, but still on quite small populations [19,20,21,22,23,24,25]. The high prevalence of OD in COVID-19 patients, its impact on the quality of life, and its possible association with the CNS manifestations, make the investigation of this phenomenon of considerable importance.
The aim of this study was to provide MRI evidence of olfactory system modifications in patients with COVID-19 and neurological symptoms, including OD. In particular, OB atrophy was investigated by measuring the OB volume on T2-weighted MR acquisitions, and OT alterations were investigated by assessing fluid-attenuated inversion-recovery (FLAIR) signal intensity in the OT.
Methods
Standard protocol approvals, registrations, and patient consents
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments. The local ethics committee approved the collection and scientific use of the patients’ data as part of a larger observational study protocol (Reg. 118/22). Informed consent was obtained from individual patients or provided by their next of kin (in case of ICU patients).
Study population
Patients were retrospectively included in the study in case of a positive COVID-19 diagnosis and admission to the ASST Papa Giovanni XXIII hospital in Bergamo, Italy, from April 2020 to October 2021 due to neurological disorders and/or olfactory dysfunctions. COVID-19 diagnosis was confirmed: (1) by real-time reverse-transcriptase polymerase-chain-reaction (RT-PCR) on nasopharyngeal specimens; or (2) by RT-PCR on bronchoalveolar lavage (BAL) in case of high clinical suspicion of SARS-CoV-2 infection besides negative test results on at least two nasopharyngeal swabs performed at least 24 h apart; or (3) in the presence of characteristic radiological interstitial pneumonia associated with typical symptoms (fever, dry cough, dyspnea), even with negative RT-PCR. Patients with pre-existing smell/taste disorders, with neurological disorders prior to COVID-19 (e.g., multiple sclerosis, previous history of vascular lesions, psychiatric diseases), pre-existing brain parenchymal lesions (e.g., chronic stroke, tumors) and/or comorbidities were excluded from the study. Patients showing cerebrovascular disorders with parenchymal lesions (e.g., stroke, cerebral venous thrombosis) due to COVID-19 were further excluded, to avoid possible errors in automatic brain segmentation and brain volume computation.
The control group consists of individuals having neither history of COVID-19 (COVID-19 diagnosis or COVID-19-related symptoms), nor self-reported chemosensory dysfunction, who underwent brain MRI at the Neuroradiology Department of the Bergamo hospital for reasons other than COVID-19 complications, with negative MRI findings.
MRI acquisition
All brain MRI scans were acquired at the ASST Papa Giovanni XXIII hospital in Bergamo, Italy, using a General Electric 3 Tesla MRI scanner (Discovery MR 750w GEM).
For both patients and controls, the brain MRI acquisition protocol included pre-contrast axial T1-weighted, coronal T2-weighted and sagittal FLAIR imaging. T1-weighted scans were acquired by an axial Multi Echo Multi Planar (MEMP) sequence with the following parameters: matrix = 288 × 244, field of view = 250 × 250 mm, thickness/gap = 3.0/0.4 mm, TE/TR = 9/600 ms. The T2-weighted MRI scans were acquired by a Periodically Rotated Overlapping ParallEL Lines with Enhanced Reconstruction (PROPELLER) sequence with the following parameters: matrix = 352 × 352, field of view = 210 × 210 mm, slice thickness from 2.4 to 4.5 mm, TE/TR = 128/5791 ms. The FLAIR MRI scans were acquired by a 3D CUBE sequence with the following parameters: matrix = 240 × 230, field of view = 260 × 260 mm, thickness/gap = 1.2/0 mm, TE/TR = 120/5302 ms.
MRI processing
Bilateral OB volume and OT intensity were measured by ad-hoc semi-automatic processing procedures using the following software: ImageJ, version 1.53 h (https://imagej.nih.gov/ij); Statistical Parametric Mapping, version SPM12 (The Wellcome Centre for Human Neuroimaging, UCL Queen Square Institute of Neurology, London, UK); and an in-house code written in MATLAB, version R2020a (Natick, MA, USA).
OB volume quantification
The OBs, appearing as hyso- or tenderly hypointense, ovoid structures surrounded by hyperintense CSF on coronal T2-weighted MR scans (Fig. 1a), were manually outlined on sequential slices using ImageJ (Fig. 1b). The OT volume was not considered; and the sudden change in diameter on the coronal section was considered as OB ending point. Manual tracing was performed by a single operator (S.C.) for all subjects; possible doubts were reviewed and solved in concordance with two trained neuroradiologists (A.B. and G.P.). The operators were blinded to the patient group, as well as to patients’ age and gender. Left and right OB volumes were computed as the sum of the surface area of all OB outlines, multiplied by the slice thickness. Total OB volume was finally computed as the sum of left and right OB volumes.
Olfactory bulb and tract appearance on brain MRI scans. a Coronal T2-weighted MRI scan showing the location and appearance of the olfactory bulbs, surrounded by T2 hyperintense CSF. b Left olfactory bulb outlined on the T2-weighted MRI scan using ImageJ polygon selection tool. c Sagittal FLAIR MRI showing the location of the left olfactory tract, appearing hyperintense compared to normal. d Left olfactory tract outlined on the T2-weighted MRI scan using ImageJ polygon selection tool. Images were taken from a 55-year-old female patient with anosmia, attention and memory deficit, and neuropathy following COVID-19 infection
OB volumes were then normalized to the corresponding brain volume, that was computed on brain masks created on T1-weighted MR scans using SPM12 (Online Resource 1). The T1-weighted MR images were first converted to the Neuroimaging Informatics Technology Initiative (NifTI) format and segmented to obtain the grey matter (GM), white matter (WM), CSF, bone tissue and soft tissue probability maps. GM, WM, and CSF maps were then binarized using a threshold (set at 0.6) empirically chosen to assign each voxel to a tissue class, while avoiding overlap between different classes. GM, WM, and CSF binary masks were then summed up, and the resulting mask was visually inspected and edited by ImageJ software to fill possible holes and remove external regions accidentally taken as brain. Brain volume was finally computed as the sum of all sectional areas, multiplied by the slice thickness.
OT intensity quantification
The OTs were observed on the sagittal FLAIR MR scans as thin, hyperintense projections surrounded by hypointense CSF (Fig. 1c). The measurement of OT signal intensity relied on preliminary OT manual outlining on one to two slices where it was best visualized. Unlike OBs, the OT outlining did not exactly follow the OT contour but was internal to it, not to include any partial volume or CSF hypointense voxel that may have biased the assessment of OT signal intensity (Fig. 1d). The OT outline was then saved as a binary mask.
FLAIR images were intensity normalized using an automated SPM12-based processing procedure specifically designed for the purpose of this study (Online Resource 2), based on a previously published method [26].
The axial T1-weighted and the sagittal FLAIR sequences were first converted to the NifTI format. The T1-weighted scan was spatially normalized to the reference MNI space (ICBM152) and then segmented to generate GM, WM, CSF, bone tissue and soft tissue probability maps. WM and GM maps were binarized by imposing 0.6 as a threshold.
The FLAIR scan was bias corrected and then normalized to the MNI space (ICBM152) by applying the same parameters used to spatially normalize the T1-weighted scan.
The T1-weighted-based WM and GM binary maps were used as an internal reference for intensity normalization of the FLAIR scan. Indeed, the intensity of the GM and WM voxels of the spatially normalized FLAIR image were averaged, the overall mean (\(m\)) was computed, and \(1000/m\) was chosen as the global modulating factor for intensity normalization of the original (non-spatially normalized and non-bias-corrected) FLAIR image.
OT intensity was finally quantified using an in-house MATLAB code, by overlapping the OT binary mask—obtained from the manual outlining—with the intensity normalized FLAIR and computing the median FLAIR intensity of the voxels within the OT mask.
Statistical analysis
All statistical analyses were performed using R software (R Core Team, Vienna, Austria, https://www.r-project.org/), version 4.1.2. Non-parametric Wilcoxon rank sum tests were used to compare patients with controls in terms of age, brain volumes, OB volumes and OT signal intensities. Fisher test was used to assess significant difference in gender due to unequal sample sizes. Independent t-test was used to compare patient subgroups. The distribution of (left, right or total) OB volume and (left, right or overall) median OT intensity by each binary variable (group, gender, and age) was displayed by boxplots. Strength of associations between OB volume and time from disease onset to MRI acquisition was assessed by Spearman correlation. Statistical significance was set at p < 0.050.
Data availability
The data that support the findings of this study are available from the corresponding author, prior submission of a project outline.
Results
A total of 237 patients with COVID-19 and neurologic manifestations were considered eligible for inclusion in the study; 23 were excluded due to motion artifacts or low image quality, and 196 were finally included in the study. 78/196 (40%) COVID-19 patients (age: 48 [36–55] years, 57.7% females) reported OD as the only COVID-19 neurological complication, while the remaining 118 patients (age: 56 [50–62] years, 60.2% females) reported a variety of other neurological disorders (ND), including cranial nerve neuropathies and neuromuscular disorders, cerebrovascular disorders (without parenchymal lesions), encephalopathies, and inflammatory CNS syndromes, cognitive, memory and psychiatric disorders, and seizures. Online Resource 3 is a flow chart that describes the study participants. The OD patient group was significantly younger than the ND one (48 [36–55] vs 56 [50–62] years, respectively; p < 0.001), while the two groups did not significantly differ in gender.
A total of 40 controls were considered for inclusion in the study; one was excluded due to technical reasons. Demographic data about the study population are summarized in Table 1. No statistically significant difference in age between patients and controls was found (53 [42–60] vs 55 [46–66] years, respectively; p = 0.116). Patients showed significantly lower brain volume as compared to controls (1420 [1333–1508] mL vs 1498 [1365–1600] mL; p = 0.048). In particular, brain volume was significantly lower than normal in ND group (1407 [1318–1501] mL, p = 0.018), but not in the OD group (1435 [1350–1526] mL, p = 0.272). Regression analyses showed that brain volume differences between groups were mainly due to the higher prevalence of females, who are denoted by smaller brain volumes than males, in the COVID-19 group (Online Resources 4 and 5).
Olfactory bulb atrophy
Control subjects showed normal and symmetric normalized OB volume (left: 2.07 [1.72–2.54]; right: 2.33 [2.01–2.70]; total: 4.44 [3.65–5.45]). In the patient group, OB volumes were significantly lower than in normal controls (left: 1.78 [1.43–2.25], p = 0.006; right: 2.06 [1.61–2.45], p = 0.005; total: 3.90 [3.09–4.71], p = 0.006) (Fig. 2). In the patient group, there were two cases of bilateral complete atrophy of the OBs, and two cases of unilateral complete atrophy (Fig. 3).
Representative MR images of complete atrophy of the olfactory bulbs in COVID-19 patients. Coronal T2-weighted MRI scan showing a normal-volume olfactory bulbs in a 63-year-old male control subject, b complete atrophy of the left OB in a 48-year-old female COVID-19 patient, and c bilateral complete OB atrophy in a 77-year-old female COVID-19 patient. Abbreviations: OB olfactory bulb
No statistically significant differences were found in total OB volumes between males and females, neither in the patient group (females 3.77 [3.05–4.61], males 4.00 [3.15–4.85], p = 0.391) nor in the control group (females 4.64 [3.71–5.25], males 4.40 [3.54–5.52], p = 0.667) (Fig. 4).
Olfactory bulb volume distribution in 196 COVID-19 patients and 39 controls, by gender and age. a Distribution of the total OB volume in the patient group, by gender (116 females and 80 males). b Distribution of the total OB volume in the control group, by gender (19 females and 20 males). c Distribution of the total OB volume in the patient group, by age (166 young patients < 65 years and 30 elderly patients). d Distribution of the total OB volume in the control group, by age (28 young controls and 11 elderly controls). OB volume was normalized to brain volume. Abbreviations: OB olfactory bulb
In the control group, younger subjects (below 65 years of age [27]) showed significantly higher total OB volume than the elderly (4.65 [3.85–5.59] vs 3.56 [3.03–4.46], p = 0.014). No such difference was found in the patient group (total OB volume = 3.92 [3.19–4.70] and 3.49 [2.65–4.81] in young and old patients, respectively, p = 0.314) (Fig. 4).
No statistically significant difference in OB volume was found between COVID-19 patients with OD compared to patients exhibiting other neurological symptoms (total OB volume: 3.85 [3.00–4.38] in the OD group vs 3.92 [3.17–4.79] in the ND group, p = 0.320) (Fig. 5).
Olfactory bulb volume distribution in 196 COVID-19 patients, subgrouped by neurological complication. a Distribution of the right OB volume in patients complaining about olfactory dysfunction only (OD) and patients with other neurological disorders (ND). b Distribution of the left OB volume in OD and ND patients. d Distribution of the total OB volume in OD and ND patients. p-value was assessed by t-test. OB volume was normalized to whole brain volume. Abbreviations: OB olfactory bulb, OD = olfactory dysfunction only, ND other neurological disorders
In the patient group, the MRI time, defined as number of days between disease onset and MRI acquisition, ranged from 1 to 582 days. However, no statistically significant differences were found in total OB volume between patients subgrouped by MRI time, and no significant correlation was found between total OB volume and MRI time (rho = – 0.006; p = 0.940) (Online Resource 6).
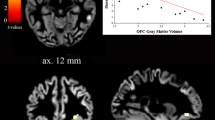
Olfactory tract alteration
Among the study population considered for the OB volumetry, 31 additional patients were excluded because of motion artifacts, low image quality (n = 16), or failure in identifying the OTs (n = 15). One additional control was excluded for MR artifacts in the OT. 165 patients (median age 52 years, 58% females) and 38 controls (median age 54 years, 50% females) were therefore considered eligible for the assessment of OT hyperintensities. The control and patient groups did not significantly differ either in age (p = 0.06), nor in gender (p = 0.462). There was no statistically significant difference in the OT FLAIR signal intensity between patients and controls (284 [204–364] vs 291 [219–406], respectively; p = 0.710). However, several outliers were found in the patient group (Fig. 6), with OT FLAIR signal intensity higher than any control subject. These outliers did not show any significant difference in age, gender, total OB volume and COVID-19 subgroup prevalence, as compared with the other patients.
Discussion
In this study, we found statistically significant OB atrophy in COVID-19 patients with neurological complications as compared with normal controls, with few cases of bilateral or unilateral complete OB atrophy. These findings are in line with previous studies showing OB volume loss occurring in response to upper respiratory tract infections [28,29,30] and correlating with olfactory function [11, 28, 31,32,33]. Moreover, our findings are also in line with previous case reports [14, 17] and quantitative studies [20,21,22], still limited to quite small populations, reporting OB atrophy in patients with COVID-19 related anosmia.
Age-related olfactory bulbs’ atrophy was found in the control population, in line with the well-known physiological decline with age of the five senses, including smell [33, 34]. Conversely, no significant difference in OB volume by age was found in the COVID-19 patient population, suggesting that SARS-CoV-2 infection may cause OB atrophy in all patients irrespective of age, with effects most visible in young and middle-aged patients.
In this study, OD included both smell and gustation disorders, since COVID-19-related taste loss most likely reflects a damage to the olfactory system, rather than damage to the taste buds or taste afferents [35]. No statistically significant difference in OB volume was found between COVID-19 patients with olfactory disorder and patients exhibiting other neurological symptoms. Some of the latter patients might have had OD in addition to other more severe neurological symptoms. Moreover, since the olfactory loss was self-reported and not assessed by any objective test, OD prevalence might have been underestimated, as reported in previous studies [9, 36]. Our results, along with a previous study finding no difference in OB volume between COVID-19 patients with and without self-reported olfactory loss [37], suggest that OB atrophy may be associated with the neurological sequelae of COVID-19, even without leading to (self-perceivable) olfactory loss, supporting the hypothesis of SARS-CoV-2 using the olfactory pathway as a gateway to the brain. This is further supported by the findings of Gu et al. [38] and Buzhdygan et al. [39], but true evidence of the neuroinvasive potential of the Coronavirus is still missing. It may be also possible that neurological complications are due to para- or post-infectious immune processes occurring in response to the virus. Further research is required to investigate this aspect.
Although this is a cross-sectional study, the absence of a significant correlation between MRI time and OB volume suggests that the OB atrophy may be persistent over time or even permanent. The duration of olfactory loss following SARS-CoV-2 infection has been reported to be highly variable, ranging from a few days to many weeks [40, 41], and in some cases up to 1-year after the infection [42]. Besides few case reports [43], to date, no relevant large studies have investigated OB volume evolution over time in COVID-19. The persistent OB atrophy observed in this study may be explained by a possible damage in the olfactory ensheathing cells (OECs) inside the olfactory mucosa, that may lose their usual capability of regenerating olfactory axons within the olfactory nervous system [44]. Future longitudinal brain MRI studies are needed to clarify the temporal evolution of the OB atrophy in COVID-19, and therefore the transient or permanent nature of this structural damage.
We found no significant evidence of FLAIR signal alteration within the OT in the COVID-19 patient group, except for few outliers. This result seems in contrast with previous case reports showing FLAIR hyperintensities in the OB and/or OT of COVID-19 patients [12, 15, 19], and with few COVID-19 studies finding FLAIR OB hyperintensity in 12 COVID-19 patients with neurological symptoms compared with age-matched controls with olfactory dysfunction [21], in 19 anosmic COVID-19 patients [22], and in other 19 COVID-19 patients with persistent olfactory dysfunction [22]. However, beyond the limited sample size of the previous studies, likely causing possible outliers to significantly bias the results, there are several methodological details that may explain this discrepancy. Subjective appreciation of OT signal alterations, given the small size of the structure, could lead to misinterpretation [45]. Moreover, in the previous quantitative studies, OB FLAIR signal was normalized based on the average signal of a ROI placed in the left superior [23] or ipsilateral frontal white matter [24], that we can not rule out being altered in COVID-19 pathology. Conversely, in the current study FLAIR signal was normalized to the average between GM and WM FLAIR intensity, thus reducing the effect of possible local alterations. Last, even though the OT FLAIR signal intensity is known to vary considerably according to the MRI scanner and acquisition parameters, this cannot have affected our results [45] since all patients and controls involved in this study were acquired on the same scanner with the same acquisition protocol.
The main added value of this study in comparison with the studies published so far is the noteworthy number of patients that to the best of our knowledge is the largest COVID-19 population with quantitative analysis of the olfactory system ever published. Such a large population allowed us to investigate the effects of age, gender, and anosmia on olfactory bulbs’ volume, while maintaining adequate statistical power. Another major strength of this study is the MRI processing procedure specifically developed for the purpose of this study, which allowed to accurately quantify both OB atrophy and OT possible alterations. Last, the normalization of the olfactory bulbs’ volume by the brain volume is a novelty aspect, allowing to account for differences in physical appearance thus obtaining unbiased results.
One of the main study limitations is that no COVID-19 patients without neurological complications underwent brain MRI and could be used as control patients; it was therefore not possible to assess any possible association between olfactory system alterations and neurological disorders in COVID-19.
The rather low number of controls was mainly due to technical reasons. For MRI protocol consistency, it was not possible to include in the control group MRI scans acquired on MRI scanners different from the one used for COVID-19 patients, or before the study starting, when the MRI protocol adopted in this study was not in place yet. Moreover, we cannot rule out the possibility that some normal controls, despite never having COVID-19-related symptoms, were affected by entirely asymptomatic COVID-19 pathology, and could therefore have partly biased the study results. Secondly, since data acquisition was performed during clinical practice and not as part of a clinical trial, MRI time was not standardized and even very variable from patient to patient. Patients with olfactory disorders underwent brain MRI significantly later than patients with additional neurological complications, and this could have affected the results. Thirdly, in this study, the olfactory disorder was self-reported and not quantified; therefore, it was not possible to investigate the association between OB atrophy and severity of the olfactory dysfunction. Although the OB was clearly visible on coronal T2-weighted images in all cases included in the study, the variability in slice thickness may have affected OB volume quantification. Moreover, OB volumetry technique, as accurate may be, is operator dependent; possible inconsistencies in manual drawing of the OBs may have biased the results. Last, the monocentric recruitment in a single ethnic group could limit the generalizability of the study findings.
Future longitudinal studies featuring the administration of a validated smell test such as the Sniffin’ Sticks Test [46] are needed to objectively assess and quantify OD, investigate the correlation between OB volume and olfactory function, and clarify the transient or permanent nature of OB atrophy in COVID-19 pathology.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed 28 Feb 2022
Ellul MA, Benjamin L, Singh B et al (2020) Neurological associations of COVID-19. The Lancet Neurology 19:767–783. https://doi.org/10.1016/S1474-4422(20)30221-0
Veleri S (2021) Neurotropism of SARS-CoV-2 and neurological diseases of the central nervous system in COVID-19 patients. Exp Brain Res. https://doi.org/10.1007/s00221-021-06244-z
Zubair AS, McAlpine LS, Gardin T et al (2020) Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2019: A Review. JAMA Neurol 77:1018. https://doi.org/10.1001/jamaneurol.2020.2065
Tsivgoulis G, Fragkou PC, Delides A et al (2020) Quantitative evaluation of olfactory dysfunction in hospitalized patients with Coronavirus [2] (COVID-19). J Neurol 267:2193–2195. https://doi.org/10.1007/s00415-020-09935-9
Lechien JR, Chiesa-Estomba CM, Beckers E et al (2021) Prevalence and 6-month recovery of olfactory dysfunction: a multicentre study of 1363 COVID-19 patients. J Intern Med 290:451–461. https://doi.org/10.1111/joim.13209
Liu N, Yang D, Zhang T et al (2022) Systematic review and meta-analysis of olfactory and gustatory dysfunction in COVID-19. Int J Infect Dis 117:155–161. https://doi.org/10.1016/j.ijid.2022.02.004
López-Elizalde R, Campero A, Sánchez-Delgadillo T et al (2018) Anatomy of the olfactory nerve: A comprehensive review with cadaveric dissection: Anatomy of the Olfactory Nerve. Clin Anat 31:109–117. https://doi.org/10.1002/ca.23003
Karamali K, Elliott M, Hopkins C (2022) COVID-19 related olfactory dysfunction. Current Opinion in Otolaryngology & Head and Neck Surgery 30:
Duprez TP, Rombaux P (2010) Imaging the olfactory tract (cranial nerve #1). Eur J Radiol 74:288–298. https://doi.org/10.1016/j.ejrad.2009.05.065
Lie G, Wilson A, Campion T, Adams A (2021) What’s that smell? A pictorial review of the olfactory pathways and imaging assessment of the myriad pathologies that can affect them. Insights Imaging 12:7. https://doi.org/10.1186/s13244-020-00951-x
Li C-W, Syue L-S, Tsai Y-S et al (2021) Anosmia and olfactory tract neuropathy in a case of COVID-19. J Microbiol Immunol Infect 54:93–96. https://doi.org/10.1016/j.jmii.2020.05.017
Galougahi MK, Ghorbani J, Bakhshayeshkaram M et al (2020) Olfactory bulb magnetic resonance imaging in SARS-CoV-2-induced anosmia: The First Report. Acad Radiol 27:892–893. https://doi.org/10.1016/j.acra.2020.04.002
Chiu A, Fischbein N, Wintermark M et al (2021) COVID-19-induced anosmia associated with olfactory bulb atrophy. Neuroradiology 63:147–148. https://doi.org/10.1007/s00234-020-02554-1
Politi LS, Salsano E, Grimaldi M (2020) Magnetic resonance imaging alteration of the brain in a patient with coronavirus disease 2019 (COVID-19) and anosmia. JAMA Neurol 77:1028–1029. https://doi.org/10.1001/jamaneurol.2020.2125
Aragão MFVV, Leal MC, Cartaxo Filho OQ et al (2020) Anosmia in COVID-19 associated with injury to the olfactory bulbs evident on MRI. AJNR Am J Neuroradiol 41:1703–1706. https://doi.org/10.3174/ajnr.A6675
Liang Y-C, Tsai Y-S, Syue L-S et al (2020) Olfactory bulb atrophy in a case of COVID-19 with hyposmia. Acad Radiol 27:1649–1650. https://doi.org/10.1016/j.acra.2020.08.016
Laurendon T, Radulesco T, Mugnier J et al (2020) Bilateral transient olfactory bulb edema during COVID-19–related anosmia. Neurology 95:224. https://doi.org/10.1212/WNL.0000000000009850
Keshavarz P, Haseli S, Yazdanpanah F et al (2021) A systematic review of imaging studies in olfactory dysfunction secondary to COVID-19. Acad Radiol 28:1530–1540. https://doi.org/10.1016/j.acra.2021.08.010
Altunisik E, Baykan AH, Sahin S et al (2021) Quantitative Analysis of the Olfactory System in COVID-19: An MR Imaging Study. AJNR Am J Neuroradiol 42:2207–2214. https://doi.org/10.3174/ajnr.A7278
Yildirim D, Kandemirli SG, Tekcan Sanli DE et al (2022) A comparative olfactory MRI, DTI and fMRI study of COVID-19 related anosmia and post viral olfactory dysfunction. Acad Radiol 29:31–41. https://doi.org/10.1016/j.acra.2021.10.019
Kandemirli SG, Altundag A, Yildirim D et al (2021) Olfactory bulb MRI and paranasal sinus CT findings in persistent COVID-19 anosmia. Acad Radiol 28:28–35. https://doi.org/10.1016/j.acra.2020.10.006
Strauss SB, Lantos JE, Heier LA et al (2020) Olfactory Bulb Signal Abnormality in Patients with COVID-19 Who Present with Neurologic Symptoms. AJNR Am J Neuroradiol 41:1882–1887. https://doi.org/10.3174/ajnr.A6751
Chetrit A, Lechien JR, Ammar A et al (2020) Magnetic resonance imaging of COVID-19 anosmic patients reveals abnormalities of the olfactory bulb: Preliminary prospective study. J Infect 81:816–846. https://doi.org/10.1016/j.jinf.2020.07.028
Girardeau Y, Gallois Y, De Bonnecaze G, et al (2020) Confirmed central olfactory system lesions on brain MRI in COVID-19 patients with anosmia: a case-series. medRxiv 2020.07.08.20148692. https://doi.org/10.1101/2020.07.08.20148692
Huppertz H-J, Wagner J, Weber B et al (2011) Automated quantitative FLAIR analysis in hippocampal sclerosis. Epilepsy Res 97:146–156. https://doi.org/10.1016/j.eplepsyres.2011.08.001
(2010) World Health Organization (WHO). Definition of an older or elderly person. Geneva; 2010
Chung MS, Choi WR, Jeong H-Y et al (2018) MR imaging-based evaluations of olfactory bulb atrophy in patients with olfactory dysfunction. AJNR Am J Neuroradiol 39:532–537. https://doi.org/10.3174/ajnr.A5491
Yao L, Yi X, Pinto JM et al (2017) Olfactory cortex and olfactory bulb volume alterations in patients with post-infectious Olfactory loss. Brain Imaging Behav 12:1355–1362
Hummel T, Urbig A, Huart C et al (2015) Volume of olfactory bulb and depth of olfactory sulcus in 378 consecutive patients with olfactory loss. J Neurol 262:1046–1051. https://doi.org/10.1007/s00415-015-7691-x
Buschhüter D, Smitka M, Puschmann S et al (2008) Correlation between olfactory bulb volume and olfactory function. Neuroimage 42:498–502. https://doi.org/10.1016/j.neuroimage.2008.05.004
Mueller A, Rodewald A, Reden J, et al (2005) Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction. NeuroReport 16:
Rombaux P, Mouraux A, Bertrand B et al (2006) Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss. Laryngoscope 116:436–439. https://doi.org/10.1097/01.MLG.0000195291.36641.1E
Doty R, Kamath V (2014) The influences of age on olfaction: a review. Frontiers in Psychology 5:. https://doi.org/10.3389/fpsyg.2014.00020
Moein ST, Hashemian SM, Mansourafshar B et al (2020) Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol 10:944–950. https://doi.org/10.1002/alr.22587
Favero R, Hajrulla S, Bordin A et al (2022) Olfactory dysfunction in COVID-19 patients who do not report olfactory symptoms: a pilot study with some suggestions for dentists. Int J Environ Res Public Health 19:1036. https://doi.org/10.3390/ijerph19031036
Akkaya H, Kizilog LuA, Dilek O et al (1992) (2021) Evaluation of the olfactory bulb volume and morphology in patients with coronavirus disease 2019: can differences create predisposition to anosmia? Rev Assoc Med Bras 67:1491–1497. https://doi.org/10.1590/1806-9282.20210678
Gu J, Gong E, Zhang B et al (2005) Multiple organ infection and the pathogenesis of SARS. J Exp Med 202:415–424. https://doi.org/10.1084/jem.20050828
Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, et al (2020) The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood-brain barrier. Neurobiol Dis 146:105131. https://doi.org/10.1016/j.nbd.2020.105131
Amer MA, Elsherif HS, Abdel-Hamid AS, Elzayat S (2020) Early recovery patterns of olfactory disorders in COVID-19 patients; a clinical cohort study. Am J Otolaryngol 41:102725–102725. https://doi.org/10.1016/j.amjoto.2020.102725
Chiesa-Estomba CM, Lechien JR, Radulesco T et al (2020) Patterns of smell recovery in 751 patients affected by the COVID-19 outbreak. Eur J Neurol 27:2318–2321. https://doi.org/10.1111/ene.14440
Fortunato F, Martinelli D, Iannelli G et al (2022) Self-reported olfactory and gustatory dysfunctions in COVID-19 patients: a 1-year follow-up study in Foggia district. Italy BMC Infectious Diseases 22:77. https://doi.org/10.1186/s12879-022-07052-8
Frosolini A, Parrino D, Fabbris C, et al (2022) Magnetic resonance imaging confirmed olfactory bulb reduction in long COVID-19: literature review and case series. Brain Sci 12:. https://doi.org/10.3390/brainsci12040430
Sun X, Tan Z, Huang X et al (2019) Direct neuronal reprogramming of olfactory ensheathing cells for CNS repair. Cell Death Dis 10:646. https://doi.org/10.1038/s41419-019-1887-4
Shor N, Chougar L, Pyatigorskaya N (2021) MR imaging of the olfactory bulbs in patients with COVID-19 and anosmia: how to avoid misinterpretation. Am J Neuroradiol 42:E10. https://doi.org/10.3174/ajnr.A6921
Hummel T, Sekinger B, Wolf SR et al (1997) ‘Sniffin’ Sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22:39–52. https://doi.org/10.1093/chemse/22.1.39
Acknowledgements
The authors gratefully acknowledge Cristina Casalini, radiology technician of the ASST Papa Giovanni XXIII Bergamo, Italy, for acquisition of most MRIs in the first part of the pandemic, nurses and technicians of Neuroradiology Unit of the ASST Papa Giovanni XXIII Bergamo, Italy, for devotion and support in managing these particular patients especially at the beginning of the pandemic.
Funding
The study was supported in part by a grant from Brembo SpA (Curno, Bergamo, Italy), under the initiative “Progetto TrexUno”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no competing interests to declare.
Ethical approval
The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Online Resource 1
Schematic representation of the MRI processing procedure used for creating the whole brain masks. First, the T1-weighted brain MRI scan is segmented to obtain probability maps of the different brain tissues (step 1). Gray matter (GM), white matter (WM) and CSF probability maps are binarized (step 2) and then added up (step 3) to create the whole brain mask. (PDF 95 KB)
Online Resource 2
Schematic representation of the MRI processing procedure used for intensity normalizing the FLAIR images. First, the T1-weighted brain MRI scan is normalized to the ICBM152 reference space (step 1). The resulting image is segmented, obtaining probability maps of the different brain tissues (step 2). Gray matter (GM) and white matter (WM) probability maps are then binarized (step 3). The FLAIR scan is bias-corrected (step 4) and normalized to the reference space (step 5). The binary maps obtained from the T1-weighted scan are used to mask the normalized FLAIR scan (step 6). The average intensities of the GM and WM in the FLAIR normalized image are therefore computed (step 7), and the two values are further averaged to obtain the overall mean average (m). The original FLAIR scan is finally intensity normalized by multiplying it by the factor 1000/m (step 8). (PDF 151 KB)
Online Resource 3
Flow chart of the study population. Abbreviations: FLAIR FLuid-Attenuated Inversion Recovery, OB olfactory bulb, OD olfactory dysfunction only, ND other neurological disorders. (PDF 71 KB)
Online Resource 4
Linear regression analysis exploring the effect of COVID-19, gender, and age on brain volume. (PDF 74 KB)
Online Resource 5
Linear regression analysis exploring the effect of COVID-19 subgroups, gender and age on brain volume. (PDF 76 KB)
Online Resource 6
Association between MRI time and OB volume, normalized to whole brain volume. a Linear regression of total olfactory bulb volume on MRI time in 196 COVID-19 patients. R denotes the Spearman correlation coefficient with the pertinent p-value. b OB volume distribution in 196 COVID-19 patients, subgrouped by based on the timing of MRI acquisition (MRI within one week, from one week to three months, from three to six months, from six months to one year and beyond one year). Pairwise comparisons were performed by Wilcoxon test. Abbreviations: OB olfactory bulb. (PDF 144 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Capelli, S., Caroli, A., Barletta, A. et al. MRI evidence of olfactory system alterations in patients with COVID-19 and neurological symptoms. J Neurol 270, 1195–1206 (2023). https://doi.org/10.1007/s00415-023-11561-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11561-0