Abstract
Background and objectives
The etiologic distribution and clinical features of diplopia may differ according to the specialties involved in the management. This study aimed to establish the clinical features and underlying etiologies of diplopia by recruiting patients from all departments.
Methods
We reviewed the medical records of 4127 patients with diplopia as the chief complaint, who had been recruited from all departments at Seoul National University Bundang Hospital, Seongnam, Republic of Korea, from 2003 to 2020.
Results
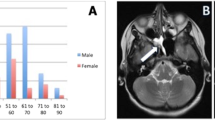
Diplopia was binocular in 3557 (94.2%) and monocular in 219 (5.8%) patients. The common causes of binocular diplopia included microvascular (n = 516, 14.5%), strokes (n = 412, 11.6%), neoplastic (n = 304, 8.5%), myasthenia gravis (n = 253, 7.1%), traumatic (n = 240, 6.7%), and decompensated phoria (n = 232, 6.5%), and comprised more than a half of the causes. Patients with binocular diplopia were usually managed by neurologists (2549/3557, 71.7%), followed by ophthalmologists (2247/3557, 63.2%), emergency physicians (1528/3557, 43.0%), neurosurgeons (361/3557, 10.1%), and others (271/3557, 7.6%). The etiologies of binocular diplopia differed markedly according to the patients’ age and the specialties involved in the management (p < 0.001).
Conclusions
Given the differences in the etiologic distribution of diplopia according to the patients’ age and the specialties involved in the management, the results of previous reports on the characteristics and etiology of diplopia, primarily performed in a single specialty department, should be interpreted with a possible selection bias.





Similar content being viewed by others
Data availability statement
Anonymized data will be shared by request from any qualified investigator.
References
McBain HB, Au CK, Hancox J, MacKenzie KA, Ezra DG, Adams GG, Newman SP (2014) The impact of strabismus on quality of life in adults with and without diplopia: a systematic review. Surv Ophthalmol 59(2):185–191. https://doi.org/10.1016/j.survophthal.2013.04.001
De Lott LB, Kerber KA, Lee PP, Brown DL, Burke JF (2017) Diplopia-Related Ambulatory and Emergency Department Visits in the United States, 2003–2012. JAMA Ophthal 135(12):1339–1344. https://doi.org/10.1001/jamaophthalmol.2017.4508
J.D. Trobe (2014) Diplopia and strabismus. In: Encyclopedia of the neurological sciences, Michigan. https://doi.org/10.1016/B978-0-12-385157-4.00126-3
O’Colmain U, Gilmour C, MacEwen CJ (2014) Acute-onset diplopia. Acta Ophthalmol 92(4):382–386. https://doi.org/10.1111/aos.12062
Morris RJ (1991) Double vision as a presenting symptom in an ophthalmic casualty department. Eye (Lond) 5(Pt 1):124–129. https://doi.org/10.1038/eye.1991.23
Nolan J (1968) Diplopia. Br J Ophthalmol 52(2):166–171. https://doi.org/10.1136/bjo.52.2.166
Comer RM, Dawson E, Plant G, Acheson JF, Lee JP (2007) Causes and outcomes for patients presenting with diplopia to an eye casualty department. Eye (Lond) 21(3):413–418. https://doi.org/10.1038/sj.eye.6702415
Kumar S (2020) Acute onset binocular diplopia: a retrospective observational study of 100 consecutive cases managed at a tertiary eye centre in Saudi Arabia. Eye (Lond) 34(9):1608–1613. https://doi.org/10.1038/s41433-019-0705-7
Bartley GB, Fatourechi V, Kadrmas EF, Jacobsen SJ, Ilstrup DM, Garrity JA, Gorman CA (1995) The incidence of Graves’ ophthalmopathy in Olmsted County, Minnesota. Am J Ophthalmol 120(4):511–517. https://doi.org/10.1016/s0002-9394(14)72666-2
Kim JH, Hwang JM (2017) Imaging of cranial nerves III, IV, VI in congenital cranial dysinnervation disorders. Korean J Ophthalmol: KJO 31(3):183–193. https://doi.org/10.3341/kjo.2017.0024
Holmes JM, Mutyala S, Maus TL, Grill R, Hodge DO, Gray DT (1999) Pediatric third, fourth, and sixth nerve palsies: a population-based study. Am J Ophthalmol 127(4):388–392. https://doi.org/10.1016/s0002-9394(98)00424-3
Harley RD (1980) Paralytic strabismus in children. Etiologic incidence and management of the third, fourth, and sixth nerve palsies. Ophthalmology 87(1):24–43. https://doi.org/10.1016/s0161-6420(80)35280-9
Höftberger R, Lassmann H (2017) Inflammatory demyelinating diseases of the central nervous system. Handb Clin Neurol 145:263–283. https://doi.org/10.1016/B978-0-12-802395-2.00019-5
Kumar N, Kaur S, Raj S, Lal V, Sukhija J (2021) Causes and outcomes of patients presenting with diplopia: a hospital-based study. Neuro-ophthalmology (Aeolus Press) 45(4):238–245. https://doi.org/10.1080/01658107.2020.1860091
Merino P, Fuentes D, Gómez de Liaño P, Ordóñez MA (2017) Binocular diplopia in a tertiary hospital: Aetiology, diagnosis and treatment. Diplopía binocular en un hospital terciario: etiología, diagnóstico y tratamiento. Archivos de la Sociedad Espanola de Oftalmologia 92(12):565–570. https://doi.org/10.1016/j.oftal.2017.05.008
Peck T, Goldberg D (2018) Double vision in adults. J Binocular Vis Ocular Motility 68(3):63–69. https://doi.org/10.1080/2576117X.2018.1481265
Wang Z, Zhu B, Fu L, Yan J (2022) Etiology and clinical features of diplopia in South China: analysis of 303 cases. Front Neurol 12:805253. https://doi.org/10.3389/fneur.2021.805253
Chowdhary S, Cavuoto KM, Osigian CJ, Capó H (2021) Characteristics of diplopia as the presenting symptom to an ocular emergency room. J AAPOS 25(3):175–177. https://doi.org/10.1016/j.jaapos.2021.02.005
Cerulli Irelli E, Di Pietro G, Fisco G, Orlando B, Asci F, Salamone EM, Morano A, Di Bonaventura C (2021) Acute-onset binocular diplopia in neurological unit: aetiological factors and diagnostic assessment. Acta Neurol Scand 144(1):92–98. https://doi.org/10.1111/ane.13425
Kremmyda O, Frenzel C, Hüfner K, Goldschagg N, Brem C, Linn J, Strupp M (2020) Acute binocular diplopia: peripheral or central? J Neurol 267(Suppl 1):136–142. https://doi.org/10.1007/s00415-020-10088-y
Wan-Seok L, Ki-Hun Y (2015) A study on the prevalence analysis of astigmatism and the effect of astigmatic refractive power on corrected vision in growing children and the young. Korean J Vis Sci 17:249–257
Rim TH, Kim SH, Lim KH, Choi M, Kim HY, Baek SH, Epidemiologic Survey Committee of the Korean Ophthalmological Society (2016) Refractive errors in Koreans: The Korea National Health and Nutrition Examination Survey 2008–2012. Korean J Ophthalmol: KJO 30(3):214–224. https://doi.org/10.3341/kjo.2016.30.3.214
Song KJ, Han MY, Kim SY, Ha JY, Kim EK (2007) Prevalence estimation of cataract based on a screening test. J Korean Ophthalmol Soc 48:768–773
Funding
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Ministry of Science and ICT (No. NRF-2021R1F1A1061527).
Author information
Authors and Affiliations
Contributions
HJK analyzed and interpreted the data and wrote the manuscript. HJK, JYC, HKY, JMH, HJK, and JSK analyzed and interpreted the data and revised the manuscript. JSK designed and conceptualized the study, interpreted the data, and revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. J. S. Kim serves as an associate editor of Frontiers in Neuro-otology and on the editorial boards of the Journal of Clinical Neurology, Frontiers in Neuro-ophthalmology, Journal of Neuro-ophthalmology, Journal of Vestibular Research, Journal of Neurology, and Medicine. The other authors have nothing to disclose.
Ethical standard
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of the Institutional Review Board of Seoul National University Bundang Hospital (B-2109–707-001).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, HJ., Kim, HJ., Choi, JY. et al. Diplopia: characteristics and etiologic distribution in a referral-based university hospital. J Neurol 270, 1067–1075 (2023). https://doi.org/10.1007/s00415-022-11471-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11471-7