Abstract
This study aimed to explore the heterogeneity of persisting symptoms after sport-related concussion (SRC). We examined the structure of symptom subtypes within 163 patients with SRC (M = 16.7 weeks post-injury). Subsequently, we investigated the existence of subgroups of patients based on comparable configuration of co-occurring symptom subtypes. To explore factors that may contribute to the emergence of SRC patient subgroups, subgroups were compared on pre-injury (i.e., demographics and medical history), personality (Severity Indices of Personality Problems Short Form) and SRC characteristics (i.e., history of prior concussions, loss of consciousness and post-traumatic amnesia). To investigate the relevance of SRC subgrouping for clinical outcome, subgroups were compared on symptom severity (Sport Concussion Assessment Tool 5). The results provide empirical evidence for the existence of symptom subtypes, characterized as a: neurocognitive, fatigue, emotional, migraine and vestibular-ocular symptom subtype in patients with persisting SRC. Study results also showed evidence for the existence of SRC subgroups of patients with a comparable configuration of co-occurring prevailing symptom subtypes, including a neurocognitive-migraine, fatigue, migraine-emotional and neurocognitive-emotional subgroup. The subgroups differed on pre-injury, personality and SRC characteristics, suggesting that these factors may contribute to the emergence of specific SRC patient subgroups. The subgroups also differed in the severity of persisting symptoms, highlighting the clinical relevance of SRC subgrouping. These results support the idea that patient subgroups with persisting SRC with a comparable pattern of co-occurring symptom subtypes exists, which may require targeted prognosis, clinical management and treatment to optimize recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, 50–60 million people suffer from traumatic brain injury (TBI) each year [1, 2], among which the majority (60–95%) have mild TBI (i.e., concussion) [3]. Sports injuries are among the most common causes (24–29%) of concussion [4]. Although the majority of patients with a concussion recover within 10–14 days, 10–15% of patients suffer from persisting symptoms (i.e., for more than 1 month) [5]. Sport-related concussions (SRCs) show great heterogeneity in terms of the emergence, evolution and recovery of symptoms and functional impairments over time [6,7,8]. To date, the sources of this variability are largely unknown and a general effective treatment for SRC is missing, which might be due to the heterogenetic nature of SRC. Moreover, prominent differences between patients challenge the development and application of clinical SRC management. Better understanding of the heterogeneity in SRC symptoms could importantly contribute to the development of more targeted and personalized care.
In recent research, the variability in SRC symptomatology has spurred a search into possible symptom subtypes of concussion. Early descriptions of SRC subtypes based on clinical observation [9] have recently been revised into consensus-driven descriptions of symptom subtypes in the acute timeframe after concussion (0–3 days post-injury), for which support was subsequently found in meta-analytic evidence [10]. In a meta-cluster analysis, we recently provided further support for delineation of SRC symptoms into subtypes within the typical course of SRC recovery (within 1 month post-injury) [11]. More specifically, the existing literature provides evidence for the existence of at least five symptom subtypes that are characterized by (i) migraine symptoms; (ii) cognitive and emotional symptoms (iii); cognitive and sleep symptoms; (iv) neurological symptoms; and (v) undefined feelings (i.e., “don’t feel right” and confusion). The literature also provides evidence for relations between symptom subtypes and clinical outcomes [11]. More specifically, symptoms relating to the migraine subtype were most strongly related to aspects of clinical outcome (e.g., prolonged recovery and cognitive deficits). Symptom subtyping may be informative with regard to the underlying cause(s) and prognosis of SRC, and may be useful to define optimal combinations of interventions in SRC management. Unfortunately, there is no research on the classification of symptom subtypes beyond the typical course of recovery, while targeted SRC management may be considered particularly crucial for the group of patients with persistent symptoms after SRC, where considerable negative impact on daily life and participation is at stake [12,13,14].
While symptom subtyping may contribute to a better understanding of the heterogeneity in persistent symptoms after SRC, symptom subtypes are known to overlap (e.g., certain symptoms contribute to multiple subtypes) and can co-occur within individuals (e.g., patients may experience symptoms from multiple subtypes at the same time) [10, 11]. This idea supports the classification of patients with persisting SRC into subgroups with a comparable configuration of co-occurring symptom subtypes (i.e., symptom subgroups). Symptom subgrouping has shown potential for combat-related concussions, with clear relevance to clinical outcome (i.e., return to duty) [15]. To our best knowledge, no study to date has investigated symptom subgroups among patients with persisting symptoms of concussion. In addition, exploring what determinants may contribute to the emergence of SRC symptom subgroups might potentially be relevant to provide insight in risk and protective factors that may pave the road to new treatment approaches.
The aim of the current study is to explore the heterogeneity of persisting symptoms after SRC. This study will investigate (1) the structure of symptom subtypes based on symptoms that tend to co-occur within patients, (2) the existence of SRC subgroups of patients, based on comparable configuration of co-occurring symptom subtypes, (3) the potential clinical relevance of SRC patients subgroups by exploring (a) whether pre-injury, personality and clinical characteristics may contribute to the emergence of SRC patient subgroups, and (b) whether SRC patient subgroups differ in terms of persisting symptom severity. This is the first study to explore SRC subgroups in patients with persisting symptoms after SRC. The results may contribute to a better understanding of the heterogeneity in SRCs, and may potentially facilitate more targeted and individualized management of patients with SRC to optimize recovery after SRC.
Methods
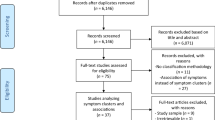
Participants
Sample
This study examined 163 patients with persisting symptoms after SRC. These patients were referred by a general practitioner to the Concussion Clinic at the Sports Medical Center of the Royal Netherlands Football Association (KNVB) between March 2018 and August 2020. This clinic offers concussion management for patients with persisting symptoms after a sport-related concussion, where persisting symptoms are defined by incomplete recovery of symptoms beyond 4 weeks post-injury [7]. The clinic focuses on optimization of recovery following SRC, not luxation of recovery in the chronic phase. Therefore, the clinic is available for patients that initiate treatment up to 9 months post-injury. For this study, the sample was confined to the adult age range (> 16 years). To increase homogeneity in terms of injury severity, patients with suspected moderate/severe TBI were excluded from this study, as reflected by self-reported loss of consciousness (LOC) > 30 min; and/or (2) anterograde post-traumatic amnesia (PTA) > 24 h [16].
Measures
Demographics and background information
Data on demographic information (i.e., sex, age and socio-economic status) and medical history (i.e., pre-injury diagnosed neurological, psychiatric, personality or learning disorders) were obtained using a custom-made questionnaire. Socio-economic status (SES) was defined as the highest level of current or finalized education, ranging from 1 (no education) to 8 (postdoctoral education) [17].
SRC characteristics
Information on history of prior concussion, the type of sport at which SRC was sustained, and SRC severity (i.e., presence of LOC, PTA and vomiting) were collected using a custom-made questionnaire.
Symptoms of concussion
Symptoms of concussion were assessed using the symptom scale of the widely used Sport Concussion Assessment Tool 5 (SCAT-5), which consists of 22-items. Severity of symptoms was rated on a 7-point Likert scale, ranging from 0 (none) to 6 (severe). In addition, patients rated what percentage of normal they felt, on a scale ranging from 0 (feeling absolutely not normal) to 100 (feeling completely normal). Each individual item score, the total score and the normality score were used for the current analysis. The SCAT-5 has shown excellent reliability (α = 0.95) [18].
Personality structure
Personality characteristics were measured using the Severity Indices of Personality Problems Short Form (SIPP-SF), assessing the following domains: self-control, identity integration, responsibility, relational capacities and social concordance. The SIPP-SF consists of 60 items rated on a 4-point Likert scale, ranging from 1 (fully disagree) to 4 (fully agree). Lower scores represent more prominent characteristics of personality disorders. The total SIPP-SF score and the score for each domain were used for the current analysis. The SIPP has adequate internal consistency reliability (Cronbach’s alpha = 0.80) [19].
Procedure
Structured prospective clinical measurements were obtained using online questionnaires that were sent out 1 week prior to the intake appointment to the clinic. Patients provided informed consent for re-use of clinical data for scientific studies. The medical ethical committee of the Amsterdam UMC (location AMC) approved this study (W18_045).
Statistical analysis
All analyses were performed using R studio (v. 1.2.1) [20]. All dependent variables were screened for outliers by using box-plots. Outliers (> M + 2SD) were subsequently rescaled using Winsorizing with the ‘Desctools’ package in R [21]. In addition, dependent measures that were not normally distributed were subjected to van der Waerden transformation, using the ‘BestNormalize’ package in R [22]. Missing data (< 1% on all measures) were imputed by multiple imputation using the ‘MICE’ package in R [23, 24].
Symptom subtypes
To identify symptom subtypes, a principal component analysis with varimax rotation of the 22 SCAT symptoms was performed using the ‘psych’ package in R [25]. The number of components to extract was determined by the cumulative proportion of variance explained (R2 ~ > 60%) [26]. Subsequently, each extracted component was considered to represent a symptom subtype, which was labeled according to the set of symptoms that made the strongest contribution to the component in terms of effect size (ƞ2 > 0.4).
To control for differences in total symptom severity between patients (reflected by the total SCAT score), we calculated dominance scores for each symptom subtype. Therefore, each individual symptom subtype score was transformed to a z-score, with higher scores reflecting higher symptom severity. Second, individual dominance scores (%) were calculated for each symptom subtype by dividing the individual z-score on each symptom subtype by the sum of z-scores for all symptom subtypes of that individual. As such, the dominance score reflects the relative contribution of a given symptom subtype to the general symptom burden of each individual.
SRC patient subgroups
To identify SRC patient subgroups, a cluster analysis (k-means clustering) on the dominance scores of the identified symptom subtypes was conducted, using the ‘NbClust’ package in R [27]. To investigate the identity of the determined SRC patient subgroups, we compared each subgroup to the other subgroups combined on the dominance scores of the symptom subtypes using t-testing. The observed group differences and effect size (Cohen’s d > 0.50) [28] were used to label subgroups based on the configuration of prevailing symptom subtypes that were found characteristic of a subgroup.
Pre-injury, personality and SRC characteristics
To explore factors that may contribute to the emergence of SRC patient subgroups, each subgroup was compared to all other subgroups on pre-injury characteristics (i.e., sex, age, SES, psychiatric and learning disorders), personality characteristics (i.e., total SIPP-SF score) and SRC characteristics (i.e., history of prior concussions, LOC and PTA). To guard against type-1 errors, significant subgroup differences on total SIPP-SF scores were followed-up by subgroup comparisons at the level of the five subscale scores.
Symptom severity
To investigate total severity of persisting symptoms, each symptom subgroup was also compared to all other subgroups combined on the total SCAT score and SCAT normality score, using independent t-tests.
All statistical testing was two-sided at α = 0.05 and effect sizes of group differences were calculated in terms of Cohen’s d for continuous dependent variables and odds ratios (OR) for binary dependent variables [28].
Results
Background information
Demographic information, SRC characteristics and medical history of 163 patients with persistent symptoms after concussion are displayed in Table 1.
Symptom subtypes
To explore the existence of symptom subtypes, a principal component analysis was performed on the 22-items of the SCAT-5. The results supported a component solution discriminating between five clusters (i.e., symptom subtypes), accounting for 59.8% of the variance. According to the set of the symptoms that made the strongest contribution to each cluster, the symptom subtypes were labelled as follows (see Table 2): (1) neurocognitive subtype: 14.0% of variance, 5 items; (2) fatigue subtype: 13.2% of variance, 4 items; (3) emotional subtype: 12.9% of variance, 4 items; (4) migraine subtype: 11.1% of variance, 3 items; and (5) vestibular-ocular subtype: 8.6% of variance, 3 items. A visual representation of the identified symptom subtypes and their relations to specific symptoms is displayed in Fig. 1.
SRC patient subgroups
To identify SRC patient subgroups with a comparable configuration of prevailing symptom subtypes, a cluster analysis was conducted. Based on the screen plot, we choose to extract a clinically manageable number of four clusters of patients, i.e., the patient subgroups. Figure 2 shows the comparison of each subgroup to the other subgroups combined on the dominance scores. The first subgroup (n = 44) was characterized by higher dominance scores on neurocognitive symptoms (t(72.9) = − 4.8, p < 0.001, d = 0.87), migraine symptoms (t(99.4) = − 4.3, p < 0.001, d = 0.72) and fatigue symptoms (t(92.6) = − 2.3, p = 0.026, d = 0.38) as compared to the other subgroups. The first subgroup was therefore labeled as the neurocognitive-migraine subgroup, which also displayed lower dominance scores on emotional symptoms (t(131.7) = 11.5, p < 0.001, d = 1.77) and vestibular-ocular symptoms (t(89.5) = 4.0, p < 0.001, d = 0.67) than the other subgroups. The second subgroup (n = 40) showed higher dominance scores on fatigue symptoms (t(81.4) = − 10.0, p < 0.001, d = 1.72) and vestibular-ocular symptoms (t(83.9) = − 2.6, p < 0.013, d = 0.47) than the other subgroups. The second subgroup was labeled as the fatigue subgroup, which also displayed lower dominance scores on migraine symptoms (t(91.7) = 5.2, p < 0.001, d = 0.87) and neurocognitive symptoms (t(128.0) = 8.5, p < 0.001, d = 1.30) than the other subgroups. The third subgroup (n = 44) was characterized by higher dominance scores on migraine symptoms (t(89.9) = -8.5, p < 0.001, d = 1.41) and emotional symptoms (t(79.7) = − 4.7, p < 0.001, d = 0.82) as compared to the other subgroups. Therefore, the third subgroup was labeled as the migraine-emotional subgroup, which also displayed lower dominance scores on neurocognitive symptoms (t(109.3) = 4.4, p < 0.001, d = 0.71) and fatigue symptoms (t(111.7) = 8.4, p < 0.001, d = 1.35) than the other subgroups. The last subgroup (n = 35) showed higher dominance scores on neurocognitive symptoms (t(66.3) = − 5.9, p < 0.001, d = 1.05) and emotional symptoms (t(62.6) = − 3.9, p < 0.001, d = 0.71) than the other subgroups. The last subgroup was therefore labeled as the neurocognitive-emotional subgroup and also showed lower dominance scores on fatigue symptoms (t(89.3) = 4.3, p < 0.001, d = 0.71) and migraine symptoms (t(152.1) = 12.6, p < 0.001, d = 1.80) than the other subgroups.
Clinical relevance of SRC patient subgroups
To explore subgroup differences, each patient subgroup was compared to the other subgroups combined on pre-injury characteristics (i.e., demographic information and medical history), personality characteristics, SRC characteristics and symptom severity (see Table 3).
Pre-injury characteristics
The patient subgroups did not differ on premorbid characteristics (− 1.9 ≤ ts ≤ 2.8, ps ≥ 0.07), with the single exception of SES. More specifically, the neurocognitive-migraine subgroup had lower SES than the other subgroups (t(68.9) = 2.8, p = 0.007, d = 0.50), while the emotional-migraine subgroup had higher SES than the other subgroups (t(107.7) = -2.0, p = 0.045, d = 0.33).
Personality characteristics
With regard to personality characteristics, the neurocognitive-emotional subgroup showed lower scores on the SIPP-SF (t(52.0) = 2.3, p = 0.028, d = 0.45), indicating that SRC patients with a combination of predominating neurocognitive and emotional symptoms show more prominent characteristics of personality disorders. Follow-up analysis at the level of SIPP-SF subscale scores, showed that the neurocognitive-emotional subgroup had lower responsibility domain scores (t(51.1) = 2.1, p = 0.037, d = 0.44), indicative of poorer ability to set realistic goals and achieve these goals as compared to other SRC patient subgroups. Furthermore, we found that the fatigue subgroup showed higher scores on the SIPP-SF as compared to the other subgroups (t(63.5) = − 2.5, p = 0.014, d = 0.48). Subsequent follow-up analyses on SIPP-SF subscale scores, showed that self-control (t(64.2) = − 2.1, p = 0.042, d = 0.27), relational capacities (t(74.2) = − 2.4, p = 0.019, d = 0.50) and social concordance domain scores (t(71.2) = − 2.3, p = 0.023, d = 0.42) were higher for the fatigue subgroup than other subgroups. These results indicate that patients with prevailing fatigue-related symptoms have less prominent characteristics of personality problems in general and are more likely to better tolerate, use and control emotions and impulses (self-control), genuinely care about others (relational capacities) and value someone’s identity and work with others (social concordance) than other SRC patients.
SRC characteristics
In terms of SRC severity, the frequency of LOC in the neurocognitive-migraine subgroup was higher than in the other subgroups (χ2 (1, N = 163) = 4.8, p = 0.029), indicating that SRC patients with a combination of predominating neurocognitive and migraine related symptoms are more likely to have experienced LOC post-injury than other SRC patients. No other differences were observed on SRC characteristics (i.e., prior concussion and PTA; χ2s ≤ 1.8, ps ≥ 0.180).
Symptom severity
Regarding the severity of persisting symptoms, the neurocognitive-migraine subgroup had higher total SCAT scores than the other subgroups (t(84.0) = − 2.8, p = 0.006, d = 0.48). In addition, the migraine-emotional group showed a lower normality score as compared to the other subgroups (t(77.1) = 2.1, p = 0.042, d = 0.37), while a higher normality score was observed in the neurocognitive-emotional group than the other subgroups (t(58.8) = − 4.2, p < 0.001, d = 0.77). The results indicate that, on the one hand, SRC patients with a combination of predominating neurocognitive and migraine symptoms experience higher symptom severity and SRC patients with a combination of prevailing migraine and emotional related symptoms feel less normal post-injury than other SRC patients. On the other hand, SRC patients with a combination of dominant neurocognitive and emotional related symptoms feel more normal following SRC than other SRC patients. An overview of the reported subgroup differences is displayed in Fig. 3.
Overview of significant group differences between SRC patient subgroups on pre-injury characteristics, personality characteristics, SRC characteristics and symptom severity. Color-coding refers to worse (i.e., red) or better (i.e., green) scores/associations. LOC loss of consciousness; SCAT sport concussion assessment tool 5; SES socio-economic status; SIPP-SF severity indices of personality problems short form
Discussion
This study aimed to explore the heterogeneity of persisting symptoms in a large sample of patients with sport-related concussion (SRC). The results indicate that persisting symptoms cluster within patients into distinct symptom subtypes. Furthermore, we present evidence for the existence of SRC subgroups of patients with a comparable configuration of co-occurring symptom subtypes. These SRC patient subgroups differ on pre-injury, personality and SRC characteristics, suggesting that complex interplay between such factors may contribute to the emergence of specific SRC patient subgroups. The SRC patient subgroups also differed in symptom severity, highlighting the relevance of SRC subgrouping for clinical outcome. Together, the findings of this study provide a framework for a better understanding of the distinct heterogeneity in SRC symptomatology, which may pave the way for the development of more personalized and targeted treatment of persisting symptoms after SRC.
The current study used a data-driven approach to provide empirical evidence for the existence of five subtypes of persisting symptoms after SRC, including a neurocognitive, a fatigue, an emotional, a migraine and a vestibular-ocular symptom subtype. These results align with previous work into the variability in SRC symptomatology, showing some overlap with acute symptom subtypes as established in meta analytic reviews [10, 11]. While previous work found evidence for symptom subtypes within the typical course of recovery, this study extends the existing literature by describing symptom subtypes beyond this phase (> 4 weeks post-injury; M = 16.7 weeks post-injury), characterizing long-lasting SRC. As compared to the previously determined acute symptom subtypes, vestibular and ocular symptoms seem to cluster together in the persisting subtypes, as do neurocognitive and neurological symptoms. These differences may reflect the evolution of symptom clustering over time since injury [7, 29].
Examination of systematic co-occurrence of symptom subtypes within patients further revealed evidence for the existence of distinct subgroups of SRC patient. Patients with a combination of predominating neurocognitive and migraine symptoms (neurocognitive-migraine subgroup) differentiated from other patients based on pre-injury characteristics (i.e., lower SES), SRC characteristics (higher incidence of LOC) and symptom severity (i.e., more severe symptoms). Patients with predominating fatigue symptoms were more likely to have more adaptive personality structure than other patients. Patients with predominating migraine and emotional symptoms differentiated on pre-injury characteristics (i.e., higher SES) and symptom severity (i.e., feeling less normal). Lastly, patients with predominating neurocognitive and emotional symptoms differentiated on personality characteristics (i.e., less adaptive personality structure) and symptom severity (i.e., less severe symptom severity). Taken together, these findings suggest that a complex combination of pre-injury, personality and SRC characteristics may contribute to the constellation of persisting symptoms after SRC.
The results of this study may expose several mechanisms that could influence the configuration of persistent symptoms. One of the most striking findings is that both SRC subgroups with predominating migraine symptoms (i.e., neurocognitive-migraine subgroup and migraine-emotional subgroup) have poorer outcome in terms of symptoms severity. This aligns with previous research that has identified the presence of migraine symptoms to be associated with relatively long-lasting recovery of SRC [30,31,32]. Our findings further indicate that among patients with predominating migraine symptoms, patients with lower educational level are more likely to also have predominating neurocognitive symptoms, while patients with higher educational level are more likely to also have predominating emotional symptoms. These findings corroborate with earlier research, showing that symptoms of depression and anxiety after mild TBI are more prevalent among highly educated patients. [33]. Our findings may also reflect that patients with lower educational levels have a smaller cognitive reserve. Cognitive reserve theories suggest that patients with higher education may be able to better compensate the influence of brain injury on daily life functioning with their premorbid higher level of functioning and/or deployment of (more effective) compensation strategies. [34, 35] Since educational level is also subject to cultural stigma [36], other cultural factors such as race and ethnicity might also have an impact on symptom perception and reporting [37]. However, we did not assess these cultural factors and therefore cannot investigate their relevance for our results. Lastly, this study indicates that patients with predominating neurocognitive and migraine symptoms were more likely to have sustained more severe SRC (i.e., presence of loss of consciousness). This supports the idea that persisting post-concussive symptoms might also be accounted for by a biological basis related to injury severity [38]. Together, these findings suggest that educational level and the severity of SRC might importantly influence the configuration of persistent SRC symptoms.
The results of the current study also identified two SRC subgroups with predominating neurocognitive symptoms (i.e., the neurocognitive-migraine and neurocognitive-emotional subgroups). Noteworthy, 81% of SRC patients with dyslexia were part of one of these subgroups with prevailing neurocognitive symptoms. Indeed, explorative analysis confirms that the prevalence of dyslexia is much higher in patients with predominating neurocognitive symptoms than other patients with persisting SRC (OR = 5.32, p = 0.012). This finding may reflect the presence of pre-morbid neurocognitive symptoms in patients with dyslexia, or may reflect that these patients have increased vulnerability for prevailing neurocognitive symptoms after SRC. To our knowledge, this is the first study to show a link between pre-existent dyslexia and prevailing neurocognitive symptoms after SRC, a finding that awaits replication in future studies.
Our findings provided evidence for one subgroup of SRC patients with predominating fatigue-related symptoms. Patients with predominating fatigue-related symptoms were found to have a more adaptive personality structure in general, characterized by the abilities to better able tolerate, use and control emotions and impulses, genuinely care about others, and value someone’s identity and work with others. These results suggest that adaptive personality characteristics may be related to the type of persistent SRC symptoms experienced, where fatigue symptoms are more prevailing than neurocognitive, migraine and vestibular-ocular symptoms. This finding adds to the hypothesis that personality characteristics contribute to the presence and absence of specific persistent post-concussion symptoms [39]. Vice versa, this study showed that having more prominent characteristics of personality disorders (i.e., poor ability to set realistic goals and achieve these goals) is associated with predominating neurocognitive and emotional related symptoms after SRC. This finding is partly supported by a study showing that differences in pre-injury coping (known to be strongly related to personality structure) [40] contributes to the prediction of anxiety and depression symptoms at three months following mild TBI [33]. Taken together, these findings suggest that personality characteristics may influence the configuration of persisting SRC symptoms.
The current results have relevance for concussion management, especially when considering targeted treatment of persisting symptoms. Regarding treatment options, the results indicate that specific pre-injury and SRC characteristics might predispose patients to experiencing specific symptoms in the chronic phase following SRC. Clinicians might use such knowledge when designing an individualized treatment approach from the available and emerging treatment options. For example, SRC patients with higher SES might benefit from additional psychoeducation and psychological treatment, as those patients have a higher risk for emotional disruption after SRC. In addition, specific subgroups of patients with persistent SRC might benefit from other existing and emerging treatments for persisting symptoms (e.g., cognitive behavioral therapy, graded exercise and cervical manual therapy) [41,42,43,44]. Future studies may provide valuable information on the role of prevailing symptoms in the efficiency of targeted treatment options for patient subgroups. As for prognostic purposes, results indicate that SRC patients with predominating migraine related symptoms have worse outcome than other patients, which warrants careful prospective monitoring and education of such patients in the early phase of recovery.
This study has some weaknesses. As we used prospectively collected data gathered at a single time point, we could not explore the stability of SRC patient subgroups over time. Relative stability of SRC patient subgroups may be considered important when SRC patient subgroups would be used as a starting point for individualized treatments. It remains to be investigated whether the configuration of dominant symptoms should be regarded as a state or trait of SRC patients. Considering the temporal dynamics of SRC symptoms, we consider it plausible that prevailing symptoms may change over time within patients. If so, it could be suggested that targeted treatment approaches should also flexibly adapt to the evolution of symptom configuration within patients. Furthermore, we used a sample that was confined to the adult age range, whereas research indicates that the relation between SRC symptom subtypes and recovery times may vary across ages [7, 45], which may suggest that SRC symptom subtypes in children might be different from adults. Future research should investigate SRC symptomatology in children specifically. In addition, the sample of our patients may have relatively high educational level as compared to the general population, which may decrease the generalizability of our results to other SRC populations. Finally, injury-related information was retrospectively collected and therefore prone to recall bias. Strengths of this study include the availability of a large group of patients with persisting symptoms of SRC and the use of data-driven methods to explore the heterogeneity of persisting SRC symptoms.
To our best knowledge, this study is the first to provide evidence for persisting symptom subtypes within patients with SRC as well as the existence of patient subgroups with a comparable configuration of predominant symptom subtypes. This evidence may contribute to better understand the heterogeneity in SRCs, especially where more long-lasting forms of SRC exist. In addition, the current study suggests that pre-injury, personality and SRC characteristics may contribute to the emergence of SRC subgroups within patients with persisting symptoms, and that SRC subgroups differ in terms of persisting symptom severity. These results support the idea that subgroups of patients with persisting SRC with a comparable pattern of co-occurring symptom subtypes allow targeted prognosis, clinical management and treatment to optimize recovery of persistent SRC. Future studies should investigate the relationship between SRC subgroups and functional outcome, which may contribute to facilitate optimal combinations of interventions and may be useful to develop novel treatment.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Hyder AA, Wunderlich CA, Puvanachandra P et al (2007) The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 22:341–353
Coronado VG, McGuire LC, Sarmiento K et al (2012) Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res 48:117
Maas AIR, Menon DK, Adelson PD et al (2017) Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol 16:987–1048
Skandsen T, Einarsen CE, Normann I et al (2018) The epidemiology of mild traumatic brain injury: the Trondheim MTBI follow-up study. Scand J Trauma Resusc Emerg Med. https://doi.org/10.1186/s13049-018-0495-0
Makdissi M, Cantu RC, Johnston KM et al (2013) The difficult concussion patient: what is the best approach to investigation and management of persistent (>10 days) postconcussive symptoms? Br J Sports Med 47:1–2
Giza CC, Kutcher JS, Ashwal S et al (2013) Summary of evidence-based guideline update: evaluation and management of concussion in sports. Neurology 80:2250–2257
McCrory P, Meeuwisse W, Dvorak J et al (2017) Consensus statement on concussion in sport—the 5 international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. https://doi.org/10.1136/bjsports-2017-097699
Reddy CC, Collins MW, Gioia GA (2008) Adolescent sports concussion. Phys Med Rehabil Clin North Am 19:247–269
Collins MW, Kontos AP, Reynolds E et al (2014) A comprehensive, targeted approach to the clinical care of athletes following sport-related concussion. Knee Surg Sport Traumatol Arthrosc 22:235–246
Lumba-Brown A, Teramoto M, Josh Bloom O et al (2020) Concussion guidelines step 2: evidence for subtype classification. Neurosurgery. https://doi.org/10.1093/neuros/nyz332
Langdon S, Königs M, Adang EAMC et al (2020) Subtypes of sport-related concussion: a systematic review and meta-cluster analysis. Sports Med. https://doi.org/10.1007/s40279-020-01321-9
Sterr A, Herron KA, Hayward C et al (2006) Are mild head injuries as mild as we think? Neurobehavioral concomitants of chronic post-concussion syndrome. BMC Neurol 6:7
Whittaker R, Kemp S, House A (2007) Illness perceptions and outcome in mild head injury: a longitudinal study. J Neurol Neurosurg Psychiatry 78:644–646
Hall RCW, Hall RCW, Chapman MJ (2005) Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics 46:195–202
Bailie JM, Kennedy JE, French LM et al (2016) Profile analysis of the neurobehavioral and psychiatric symptoms following combat-related mild traumatic brain injury: identification of subtypes. J Head Trauma Rehabil 31:2–12
Malec JF, Brown AW, Leibson CL et al (2007) The mayo classification system for traumatic brain injury severity. J Neurotrauma 24:1417–1424
Statistics Netherlands (2006) The Dutch standard classification of education
Robinson M (2019) Evaluation of the psychometric and measurement properties of the SCAT5 and child SCAT5 [dissertation]. The University of Western Ontario
Goodman R (2001) Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 40:1337–1345
Rstudio Team (2015) RStudio: integrated development for R. RStudio Inc., Boston, MA
Signorell A, Aho K, Alfons A, Anderegg N, Aragon T, Arppe A, Baddeley A et al (2016) DescTools: tools for descriptive statistics. R package version 0.99.18. Available at https://cran.r-project.org/package=DescTools
Peterson RA, Cavanaugh JE (2020) Ordered quantile normalization: a semiparametric transformation built for the cross-validation era. J Appl Stat 47:2312–2327
Sterne JAC, White IR, Carlin JB et al (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ (Online). https://doi.org/10.1136/bmj.b2393
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 45:1–67
Revelle W, Northwestern University. psych: procedures for psychological, psychometric, and personality research.
Jolliffe I (2002) Principal component analysis. Springer, New York
Charrad M, Ghazzali N, Boiteau V et al (2014) Nbclust: an R package for determining the relevant number of clusters in a data set. J Stat Softw 61:1–36
Cohen J (1988) Statistical power analysis for the behavioral sciences. Stat Power Anal Behav Sci. https://doi.org/10.1234/12345678
Duhaime AC, Beckwith JG, Maerlender AC et al (2012) Spectrum of acute clinical characteristics of diagnosed concussions in college athletes wearing instrumented helmets: clinical article. J Neurosurg 117:1092–1099
Kontos AP, Elbin RJ, Lau B et al (2013) Posttraumatic migraine as a predictor of recovery and cognitive impairment after sport-related concussion. Am J Sports Med 41:1497–1504
Howell DR, Kriz P, Mannix RC et al (2018) Concussion symptom profiles among child, adolescent, and young adult athletes. Clin J Sport Med. https://doi.org/10.1097/jsm.0000000000000629
Mihalik JP, Register-Mihalik J, Kerr ZY et al (2013) Recovery of posttraumatic migraine characteristics in patients after mild traumatic brain injury. Am J Sports Med 41:1490–1496
Maestas KL, Sander AM, Clark AN et al (2014) Preinjury coping, emotional functioning, and quality of life following uncomplicated and complicated mild traumatic brain injury. J Head Trauma Rehabil 29:407–417
Stern Y (2002) What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 8:448–460
Kesler SR, Adams HF, Blasey CM et al (2003) Premorbid intellectual functioning, education, and brain size in traumatic brain injury: an investigation of the cognitive reserve hypothesis. Appl Neuropsychol 10:153–162
Papadopoulos C, Leavey G, Vincent C (2002) Factors influencing stigma. A comparison of Greek-Cypriot and English attitudes towards mental illness in north London. Soc Psychiatry Psychiatr Epidemiol 37:430–434
Misra S, Jackson VW, Chong J et al (2021) Systematic review of cultural aspects of stigma and mental illness among racial and ethnic minority groups in the United States: implications for interventions. Am J Community Psychol 68:486–512
Bigler ED (2008) Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc 14:1–22
Garden N, Sullivan KA, Lange RT (2010) The relationship between personality characteristics and postconcussion symptoms in a nonclinical sample. Neuropsychology 24:168–175
Carver CS, Connor-Smith J (2010) Personality and coping. Annu Rev Psychol 61:679–704
Sullivan KA, Hills AP, Iverson GL (2018) Graded combined aerobic resistance exercise (CARE) to prevent or treat the persistent post-concussion syndrome. Curr Neurol Neurosci Rep 18:75
Langevin P, Fremont P, Fait P et al (2020) Aerobic exercise for sport-related concussion: a systematic review and meta-analysis. Med Sci Sport Exerc 08:8
Cheever K, McDevitt J, Phillips J et al (2021) The role of cervical symptoms in post-concussion management: a systematic review. Sport Med 51:1875–1891
Chen CL, Lin MY, Huda MH et al (2020) Effects of cognitive behavioral therapy for adults with post-concussion syndrome: a systematic review and meta-analysis of randomized controlled trials. J Psychosom Res. https://doi.org/10.1016/j.jpsychores.2020.110190
Howell DRPATC, Kriz PMD, Mannix RCMDMPH et al (2019) Concussion symptom profiles among child, adolescent, and young adult athletes. Clin J Sport Med 29:391–397
Acknowledgements
This research was supported by the Royal Netherlands Football Association (KNVB).
Funding
This study was funded by the Royal Netherlands Football Association (KNVB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SL, MK, EG and MI. The first draft of the manuscript was written by SL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Edwin Goedhart and Melanie Inklaar are employed as sports medicine physician at the Medical Centre of the Royal Netherlands Football Association.
Ethical approval
The Medical Centre of the Royal Netherlands Football Association has set up the concussion clinic to combine patient care an scientific research on the topic of sport-related concussion. For patient care the insurance company of the patients will cover a small part of the costs of care. The main part is being covered by the Association. This is an observational study. The medical ethical committee of the Amsterdam UMC (location AMC) has approved this study (W18_045).
Consent to participate and publish
Athletes at the sport-related concussion clinic gave verbal consent for re-use of clinical data for this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Langdon, S., Goedhart, E., Inklaar, M. et al. Heterogeneity of persisting symptoms after sport-related concussion (SRC): exploring symptom subtypes and patient subgroups. J Neurol 270, 1512–1523 (2023). https://doi.org/10.1007/s00415-022-11448-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11448-6