Abstract
Background
Hemorrhagic transformation (HT) is a common complication of alteplase treatment. However, the prevalence rate, risk factors, and clinical outcomes of remote intracerebral hemorrhage (rICH) after intravenous thrombolysis in acute ischemic stroke are not well understood.
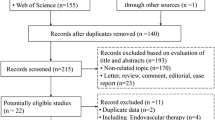
Methods
Following a previously registered protocol, the PubMed, Web of Science, and Embase databases were systematically searched to identify relevant literature up to June 2022. Cohort studies reporting thrombolysis-related rICH in patients with acute ischemic stroke were included. Random effects models were used to calculate pooled prevalence rate, mean difference (MD) or odds ratio (OR) with corresponding 95% confidence interval (CI).
Results
Fourteen studies with 52,610 patients were included in this meta-analysis. The pooled rICH prevalence was 3.2% (95% CI 3.1–3.4%). Compared to patients without intracerebral hemorrhage (ICH), those with rICH were older, more likely to be female, and had a higher proportion of prior stroke, chronic heart failure and cardioembolism, and higher diastolic blood pressure. Small vessel disease markers (e.g., white matter hyperintensities and cerebral microbleeds) were strongly associated with rICH. The presence of rICH decreased the likelihood of favorable outcomes (OR 0.36, 95% CI 0.31–0.41) and increased the risk of mortality (OR 4.37, 95% CI 2.86–6.67).
Conclusions
Although rICH is uncommon after intravenous thrombolysis, its presence can lead to worse functional outcomes and higher mortality in acute ischemic stroke. Patients at high risk of rICH must be identified based on potential risk factors.






Similar content being viewed by others
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Feigin VL, Stark BA, Johnson CO et al (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20:795–820
Emberson J, Lees KR, Lyden P et al (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384:1929–1935
He JF, Fu FW, Zhang WY, Zhan ZX, Cheng ZC (2022) Prognostic significance of the clinical and radiological haemorrhagic transformation subtypes in acute ischaemic stroke: a systematic review and meta-analysis. Eur J Neurol. https://doi.org/10.1111/ene.15482
Hacke W, Kaste M, Fieschi C et al (1995) Intravenous thrombolysis with recombinant tissue-plasminogen activator for acute hemispheric stroke—The European Cooperative Acute Stroke Study (ECASS). JAMA-J Ame Med Assoc 274:1017–1025
von Kummer R, Broderick JP, Campbell BCV et al (2015) The Heidelberg bleeding classification classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986
Mazya MV, Ahmed N, Ford GA et al (2014) Remote or extraischemic intracerebral hemorrhage–an uncommon complication of stroke thrombolysis: results from the safe implementation of treatments in stroke-international stroke thrombolysis register. Stroke 45:1657–1663
Trouillas P, von Kummer R (2006) Classification and pathogenesis of cerebral hemorrhages after thrombolysis in ischemic stroke. Stroke 37:556–561
Curtze S, Putaala J, Sibolt G et al (2016) Cerebral white matter lesions and post-thrombolytic remote parenchymal hemorrhage. Ann Neurol 80:593–599
Prats-Sánchez L, Camps-Renom P, Sotoca-Fernández J et al (2016) Remote intracerebral hemorrhage after intravenous thrombolysis: results from a multicenter study. Stroke 47:2003–2009
Drelon A, Kuchcinski G, Caparros F et al (2020) Remote brain hemorrhage after IV thrombolysis: role of preexisting lesions. Neurology 94:e961–e967
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ-Br Med J 2021:372
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Dersimonian R, Laird N (1986) Metaanalysis in clinical-trials. Control Clin Trials 7:177–188
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ-Br Med J 315:629–634
Duval S, Tweedie R (2000) Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Brott T, Broderick J, Kothari R et al (1997) Intracerebral hemorrhage after intravenous t-PA therapy for ischemic stroke. Stroke 28:2109–2118
Nighoghossian N, Hermier M, Adeleine P et al (2002) Old microbleeds are a potential risk factor for cerebral bleeding after ischemic stroke—a gradient-echo T2*-weighted brain MRI study. Stroke 33:735–742
Martínez-Hernández E, Martínez-Ramírez S, Delgado-Mederos R et al (2010) Remote cerebral hematomas in patients treated with intravenous rt-PA. J Neurol 257:1062–1066
Kimura K, Aoki J, Shibazaki K, Saji N, Uemura J, Sakamoto Y (2013) New appearance of extraischemic microbleeds on T2*-weighted magnetic resonance imaging 24 hours after tissue-type plasminogen activator administration. Stroke 44:2776–2781
Gao Y, Churilov L, Teo S, Yan B (2015) Remote intracerebral haemorrhage post intravenous thrombolysis: experience from an Australian stroke centre. J Clin Neurosci 22:352–356
Charidimou A, Turc G, Oppenheim C et al (2017) Microbleeds, cerebral hemorrhage, and functional outcome after stroke thrombolysis individual patient data meta-analysis. Stroke 48:2084
Tejada-Meza H, Modrego PJ (2017) Cerebellar vermis: a vulnerable location of remote brain haemorrhages after thrombolysis for ischaemic stroke. Neurol Sci 38:185–187
Chen Y, Yan S, Xu M, Zhong G, Liebeskind DS, Lou M (2018) More extensive white matter hyperintensity is linked with higher risk of remote intracerebral hemorrhage after intravenous thrombolysis. Eur J Neurol 25:380-e315
Braemswig TB, Villringer K, Turc G et al (2019) Predictors of new remote cerebral microbleeds after IV thrombolysis for ischemic stroke. Neurology 92:e630–e638
Du H, Wu S, Lei H et al (2022) Total cerebral small vessel disease score and cerebral bleeding risk in patients with acute stroke treated with intravenous thrombolysis. Front Aging Neurosci 14:790262
Honig A, Percy J, Sepehry AA, Gomez AG, Field TS, Benavente OR (2022) Hemorrhagic transformation in acute ischemic stroke: a quantitative systematic review. J Clin Med 11:1162
Wang X, Li JW, Moullaali TJ et al (2019) Low-dose versus standard-dose alteplase in acute ischemic stroke in Asian stroke registries: an individual patient data pooling study. Int J Stroke 14:670–677
Whiteley WN, Slot KB, Fernandes P, Sandercock P, Wardlaw J (2012) Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator a systematic review and meta-analysis of 55 studies. Stroke 43:2904-U2235
Wang YA, Liu JF, Wu Q, Cheng YJ, Liu M, Collaborators V (2022) Validation and comparison of multiple risk scores for prediction of symptomatic intracerebral hemorrhage after intravenous thrombolysis in VISTA. Int J Stroke. https://doi.org/10.1177/17474930221106858
Charidimou A, Martinez-Ramirez S, Reijmer YD et al (2016) Total magnetic resonance imaging burden of small vessel disease in cerebral amyloid angiopathy an imaging-pathologic study of concept validation. JAMA Neurol 73:994–1001
Kozberg MG, Perosa V, Gurol ME, van Veluw SJ (2021) A practical approach to the management of cerebral amyloid angiopathy. Int J Stroke 16:356–369
Ly JV, Rowe CC, Villemagne VL et al (2010) Cerebral beta-amyloid detected by Pittsburgh Compound B positron emission topography predisposes to recombinant tissue plasminogen activator-related hemorrhage. Ann Neurol 68:959–962
Ter Telgte A, van Leijsen EMC, Wiegertjes K et al (2018) Cerebral small vessel disease: from a focal to a global perspective. Nat Rev Neurol 14:387–398
Zhang CE, Wong SM, van de Haar HJ et al (2017) Blood-brain barrier leakage is more widespread in patients with cerebral small vessel disease. Neurology 88:426–432
Bernardo-Castro S, Sousa JA, Bras A et al (2020) Pathophysiology of blood-brain barrier permeability throughout the different stages of ischemic stroke and its implication on hemorrhagic transformation and recovery. Front Neurol. https://doi.org/10.3389/fneur.2020.594672
Sakai K, Ueda M, Fukushima W et al (2019) Nationwide survey on cerebral amyloid angiopathy in Japan. Eur J Neurol 26:1487–1493
Koh YH, Lew LZW, Franke KB et al (2022) Predictive role of atrial fibrillation in cognitive decline: a systematic review and meta-analysis of 2.8 million individuals. Europace. https://doi.org/10.1093/europace/euac003
Silverman A, Kodali S, Sheth KN, Petersen NH (2020) Hemodynamics and hemorrhagic transformation after endovascular therapy for ischemic stroke. Front Neurol. https://doi.org/10.3389/fneur.2020.00728
Burgos AM, Saver JL (2019) Evidence that tenecteplase is noninferior to alteplase for acute ischemic stroke: meta-analysis of 5 randomized trials. Stroke 50:2156–2162
Katsanos AH, Psychogios K, Turc G et al (2022) Off-label use of tenecteplase for the treatment of acute ischemic stroke a systematic review and meta-analysis. JAMA Netw Open 5:e224506
Acknowledgements
The authors wish to acknowledge Dr. Zhao Han, Professor of neurology, Wenzhou Medical University, for his help in interpreting the significance of the results of this study
Funding
This work was supported by the Medical Science and Technology Project of Zhejiang Province of China (No.2021KY797).
Author information
Authors and Affiliations
Contributions
ZC conceived and designed the study. LQ, FF and WZ performed the literature search and data extraction. JH, ZZ and ZC assisted in data analysis. LQ wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval and consent to participate
Ethical approval was not needed, as no individual-level data were utilized.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qiu, L., Fu, F., Zhang, W. et al. Prevalence, risk factors, and clinical outcomes of remote intracerebral hemorrhage after intravenous thrombolysis in acute ischemic stroke: a systematic review and meta-analysis. J Neurol 270, 651–661 (2023). https://doi.org/10.1007/s00415-022-11414-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11414-2