Abstract
Backgrounds
Freezing of gait (FOG) and cognitive impairment are serious symptoms of Parkinson’s disease (PD). Understanding the association between FOG and cognition may help formulate specific interventions for PD individuals.
Objectives
We aimed to investigate the associations of cognitive impairment in different domains with FOG status using multiple neuropsychological tests.
Methods
Two cohorts including 691 and 104 participants were recruited from Parkinson’s progression markers initiative (PPMI) and central China, respectively. All participants underwent FOG assessment and neuropsychological tests, and 595 individuals from PPMI and 51 from central China were enrolled for longitudinal observation. Cross-sectional and longitudinal associations between cognition and FOG status were evaluated using multivariable-adjusted models.
Results
Worse cognitive performances were observed in patients with FOG compared to those without FOG in both cohorts (β = − 0.020, p < 0.001) using multivariate-adjusted models. Moreover, patients with progressive FOG during follow-up manifested more serious cognitive declines (HR = 1.40, 95% CI = 1.07–1.80). The FOG was mainly associated with the decline of executive, attention, and orientation. Furthermore, FOG was associated with higher levels of cognition-related biomarkers including T-tau, P-tau, and NfL in cerebrospinal fluid (p < 0.050).
Conclusions
FOG is a risk factor for cognitive decline in PD, which emphasizes the need for early detection and monitoring of cognitive changes and interventions on cognitive impairments in PD patients with FOG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease characterized by a broad spectrum of motor and non-motor symptoms with complex clinical, genetic, and molecular features [1]. Cognitive decline is one of the most serious non-motor syndromes of PD, as it is associated with decreased quality of life and increased burden on institutions, economics, and caregivers [2]. It was reported that 25% of PD patients were diagnosed with mild cognitive impairment, and approximately 80% of them would ultimately progress to dementia [1, 3]. Freezing of gait (FOG), a paroxysmal gait disturbance in which patients lose the ability to initiate or resume walking, is a serious symptom of PD and associates with disease severity [4]. The occurrence of FOG and cognitive deficits are highly variable at the different stages of PD, and both jointly lead to poor quality of life [5].
FOG is not a pure motor symptom, but rather a complex interaction effect between motor and cognition [6]. Previous studies have verified that patients with gait disturbances have a greater proportion of cognitive decline and a higher risk of developing mild cognitive impairment or dementia [7, 8], and PD patients with FOG showed faster rates of cognitive decline than those without FOG in a 2-year follow-up study [9]. However, it is reported that cognitive impairment only added the risk of FOG in PD subjects without motor complications [10], and there were studies showing no significant association between FOG and cognition [11, 12]. Thus, the association between FOG and cognitive impairment in PD remains unclear.
We hypothesize that FOG is a risk factor of cognitive impairments in PD patients. To test our hypothesis, we analyzed the association between FOG and cognitive impairment in two cohorts including 691 and 104 participants recruited from Parkinson’s progression markers initiative (PPMI) and central China, respectively. Moreover, 595 individuals from PPMI and 51 from central China were enrolled for longitudinal observation of FOG progression and cognition impairment. Understanding the association between FOG and cognition can help formulate specific interventions for PD individuals with comorbidities of FOG and cognitive impairment.
Methods
Study participants
PPMI
All clinical information of PPMI in the present study was obtained and used after formal authorization (http://www.ppmi-info.org) [13]. The PPMI was founded by the Michael J. Fox Foundation, which specifically aimed to define reliable biomarkers for predicting PD progression and create a channel for the accelerated blossom and clinical application of novel disease-modifying therapeutics by establishing large-cohort observational studies. Participants were enrolled into PPMI if they (a) were > 30 years, (b) diagnosed with PD in 2 years without medication treating, (c) had at least two symptoms of resting tremor, bradykinesia, and rigidity, or an asymmetric resting tremor or asymmetric bradykinesia, and (d) Hoehn and Yahr stages < 3. Participants were excluded if they (1) were diagnosed with Parkinsonism-plus syndromes, including multiple system atrophy, progressive supranuclear palsy, and Lewy body dementia; (2) had the history of surgery, including stereotactic nerve nuclei lesions and deep brain stimulation; (3) had the history of psychiatric symptoms, cancer, or any serious cardiovascular complications, and (4) could not complete the gait or cognitive evaluation. All patients underwent 3-month intervals follow-up in the first year and 6-month intervals in the subsequent years. The additional follow-up was conducted before the regularly scheduled visit if one withdrew early from the study or began symptomatic therapy. The data up to 10 years of follow-up were included from this study.
Central Chinese cohort
The Central Chinese cohort was an observational, single-center, longitudinal study that enrolled PD participants who visited the Department of Neurology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology from October 2014 to October 2021. The diagnosis of PD was based on the clinical diagnostic criteria for movement disorders in 2015 [14], and the and exclusion criteria were same as those used for PPMI. This study was approved by the Medical Ethics Committee of Tongji Hospital (Wuhan, China). Written informed consent was obtained from participants or their legally acceptable representatives. After enrollment, participants were followed up every half to 2 years.
Clinical assessments
FOG assessments
FOG was evaluated using the Movement Disorders Society–Unified Parkinson’s Disease Rating Scale (MDS–UPDRS) item 2.13 (freezing) and item 3.11 (FOG) for PPMI. The present FOG status was defined as any of these two items ≥ 1, while FOG severity was defined as the total score of MDS–UPDRS item 2.13 and 3.11. As well, the progression of FOG was defined as the FOG score ≥ 1 at any point during follow-up periods. On the other hand, the Freezing of Gait Questionnaire (FOG-Q) for the Central Chinese cohort. FOG-Q is a patient-reported outcome measure, which has six questions and can easily be administered in clinics. The total FOG-Q score ≥ 1 was defined as FOG individuals, and higher FOG-Q scores represents the more severity of FOG symptoms [15].
Cognitive assessments
Global cognitive functions were assessed by Montreal Cognitive Assessment (MoCA) in PPMI and the Central Chinese cohort. Other cognitive indicators were also examined for several specific areas, including verbal episodic memory (Hopkins Verbal Learning Test [HVLT] Immediate Recall; HVLT Delayed Recall; HVLT Recognition), visuospatial ability (Judgment of Line Orientation [JoLO]), executive function/working memory (Letter Number Sequencing [LNS]), language (Semantic Fluency Test), and processing speed/attention (Symbol Digit Modality Test [SDMT]) [16], as well as subscores of MoCA (visuospatial/executive, naming, attention, language, abstraction, delayed memory and orientation). All the cognitive tests scores were corrected according to the published norms. The cognitive declines were defined as at least two cognitive tests of more than 1.5 standard deviations below normal at baseline in line with described before [17].
PD Subtypes and levodopa equivalent daily dose (LEDD) assessments
Tremor dominant (TD) and postural instability and gait difficulty (PIGD) were grouped based on the ratio of TD to PIGD scores: TD patients with ratios > 1.15, PIGD with ratios < 0.90, and unclear with ratios among 0.90–1.15 [18]. LEDD was calculated according to the common conversion formulae [19]. The patients of PPMI did not take anti-PD medicines for their condition at the time of evaluation, while patients in the Central Chinese cohort were on medication.
Fluid biomarkers measurements
The detailed approaches were as described previously [20]. Cerebrospinal fluid (CSF) amyloid-β1-42 (Aβ1-42), total-Tau (T-tau), and phosphorylated tau (P-tau) were measured using the xMAP-Luminex platform with INNOBIA AlzBio3 immunoassay kit-based reagents (Fujirebio-Innogenetics, Ghent, Belgium), while Total α-synuclein and NfL levels were measured by enzyme-linked immunosorbent assay kit (Covance, Dedham, MA). Serum neurofilament light (NfL) levels were measured by the Simoa Human NF-light Advantage kit (UmanDiagnostics, Umeå, Sweden) using Single Molecule Array (Simoa) technology. The impacts of possible extreme outliers on the results were weakened through additional quality control.
Statistical analyses
All analyses were conducted using R (version 3.6.3), and the statistical significance threshold was set at a two-tailed p < 0.05.
Differences in demographic characteristics between patients with FOG and without FOG were assessed using the Mann–Whitney U test and χ2 test. Baseline associations of FOG and cognitive impairment were explored by multiple linear regression models that adjusted for age, sex, education levels, disease onset age, disease duration, MDS–UPDRS-III, Hoehn–Yahr stages, Geriatric Depression Scale (GDS) and apathy (MDS–UPDRS-I). The demographic characteristics and variables did not display a normal distribution (Kolmogorov–Smirnov test, p < 0.05); therefore, they were log-transformed to approximate the normal distribution by “car” package of R. Cox models were employed to compare the probabilities of cognitive decline with FOG, while mixed-effects linear models were conducted to assess the changes of cognitive impairment and fluid biomarkers. The models included random intercepts and slopes for time and an unstructured covariance matrix for random effects, which was regarded as a predictor of the interactions between time and dependent variables.
Results
Participants characteristics of PPMI
Baseline characteristics of the study participants were presented in Table 1. Briefly, 691 participants aged 62.2 years (SD = 10.2; 286 females) from PPMI were enrolled at baseline, therein 76 (11.0%) patients with FOG were identified. Of these, 96 individuals had no available visit data on follow-ups so that were excluded. Finally, 595 patients were included during the follow-ups for the longitudinal analyses, and the average follow-up period was 5.0 ± 2.4 years. Therein, 231 (43.5%) of 531 PD patients without FOG developed to FOG during the 10-year follow-up. There were no significant differences in age, educational levels and disease onset age between the FOG and non-FOG individuals as determined by Mann–Whitney U test (p > 0.05).
Baseline associations of FOG with cognitive functions of PPMI
Using the multiple linear regression models, we found that participants with FOG status had lower scores of MoCA (β = − 0.020, p < 0.001), LNS (β = − 0.050, p = 0.032) and Semantic Fluency Test (β = − 0.030, p = 0.036) after adjusting for age, sex, educational levels, age at disease onset, disease − duration, MDS-UPDRS-III, Hoehn-Yahr stages, GDS and apathy. This suggests that individuals with FOG had worse cognitive performances compared to those without FOG. Specifically, FOG was mainly associated with the cognitive functions of visuospatial/executive (β = − 0.095, p < 0.001), attention (β = − 0.037, p = 0.021), abstraction (β = − 0.070, p < 0.001) and orientation (β = − 0.013, p = 0.017) using MoCA subscores. Similar to the results of FOG status, higher FOG scores were also significantly associated with JoLO (β = − 0.019, p = 0.038) and SDMT (β = − 0.021 p = 0.002). There were no significant associations between FOG and other neuropsychological tests and fluid biomarkers (Table 2).
Longitudinal associations of FOG with cognitive functions of PPMI
Associations of baseline FOG and cognitive changes
We analyzed the association between baseline FOG and cognitive decline using multivariable-adjusted Cox proportional hazard regression and mixed-effect linear models. Patients with FOG were at a higher risk of cognitive decline (hazard ratio [HR] = 1.53, 95% confidence interval [CI] = 1.03–2.27, p = 0.035, Fig. 1a) compared to non-FOG subjects. Patients with FOG also had greater declines of total MoCA score (β = − 0.00138, p < 0.001, Fig. 1b), as well as naming (β = − 0.00108, p < 0.001, Fig. 1c), attention (β = − 0.00276, p < 0.001, Fig. 1d) and orientation (β = − 0.00306, p < 0.001, Fig. 1e) of MoCA than non-FOG subjects. In addition, the occurrence of FOG at baseline were associated with greater accumulation cognitive impairment-related biomarkers including T-tau (β = 0.00027, p = 0.038, Fig. 2a) and P-tau (β = 0.00027, p = 0.017, Fig. 2b) in CSF. On the other hand, the baseline FOG severity was associated with decreased visuospatial/executive (β = − 0.00131, p = 0.036), language (β = -0.00158, p = 0.007) and delayed memory (β = − 0.00096, p = 0.002) in MoCA, as well as LNS (β = − 0.00170, p = 0.049) (Table 3).
Associations between Baseline FOG and longitudinal cognitive changes in PPMI. The Kaplan–Meier survival curve did not show that patients with FOG had a higher risk of cognitive impairment progression (log-rank p = 0.032, a). Mixed-effect linear models indicated that baseline individuals with FOG had greater cognitive decline, including total MoCA (β = − 0.00139, p < 0.001, b), naming (β = − 0.00108, p < 0.001, c), attention (β = − 0.00276, p < 0.001, d) and orientation (β = − 0.00306, p < 0.001, e). FOG, freezing of gait; MoCA, Montreal cognitive assessment; PPMI, Parkinson’s progression markers initiative
Associations between FOG and longitudinal changes of fluid biomarkers in PPMI. On one hand, baseline FOG patients had greater accumulation of CSF T-tau (β = 0.00027, p = 0.038, a) and P-tau (β = 0.00027, p = 0.017, b), which might represent the worse cognitive condition. On the other hand, PD patients with FOG progression were likely associated more increases of CSF T-tau (β = 0.00015, p = 0.034, c), P-tau (β = 0.00013, p = 0.038, d), NfL (β = 0.00071, p = 0.009, e), as well as serum NfL (β = 0.00097, p = 0.004, f). CSF, cerebrospinal fluid; FOG, freezing of gait; NfL, neurofilament light; T-tau, total tau; PPMI, Parkinson’s progression markers initiative; P-tau, phosphorylated tau
Associations of FOG progression and cognitive changes
Cox models showed that patients with FOG progression had higher risk of cognitive impairment (HR = 1.40, 95% CI = 1.07–1.80, p = 0.007, Fig. 3a). Patients with FOG progression had more decreases of MoCA scores (β = − 0.00040, p = 0.005; Fig. 3b), HVLT total recall (β = − 0.00033, p = 0.015; Fig. 3c), HVLT delayed recall (β = − 0.00052, p < 0.001; Fig. 3d), JoLO (β = − 0.00042, p < 0.001; Fig. 3e), LNS (β = − 0.00066, p = 0.003; Fig. 3g), Semantic Fluency Test (β = − 0.00063, p < 0.001; Fig. 3f) and SDMT (β = − 0.00060, p < 0.001; Fig. 3h). The separate domains analyses revealed that the FOG progression was mostly correlated with visuospatial/executive (β = − 0.00244, p < 0.001), attention (β = − 0.00085, p = 0.014), delayed memory (β = − 0.00166, p = 0.023) and orientation (β = − 0.00074, p = 0.002) of MoCA (Table 3). Furthermore, FOG progression was associated with higher levels of cognitive impairment-related biomarkers including CSF T-tau (β = 0.00015, p = 0.034, Fig. 2c), P-tau (β = 0.00013, p = 0.038, Fig. 2d), NfL (β = 0.00071, p = 0.009, Fig. 2e) and serum NfL (β = 0.00097, p = 0.004, Fig. 2f). These data suggest that FOG progression is associated with cognitive impairment.
Associations between FOG progression with longitudinal cognitive changes in PPMI. The Kaplan–Meier survival curve expressed that patients with FOG progression had a higher risk of cognitive decline (log-rank p = 0.00037, a). Mixed-effect linear models indicated that the progression of FOG meant larger decreases of cognition, including total MoCA (β = − 0.00040, p = 0.005, b), HVLT total recall (β = − 0.00033, p = 0.015, c), HVLT delayed recall (β = − 0.00053, p < 0.001, d), JoLO (β = − 0.00042, p < 0.001, e), LNS (β = − 0.00066, p = 0.003, f), Semantic Fluency Test (β = − 0.00065, p < 0.001, g) and SDMT (β = − 0.00060, p < 0.001, h). FOG, freezing of gait; HVLT, Hopkins verbal learning test; JoLO, Benton judgment of line orientation; LNS, letter number sequencing; MoCA, Montreal cognitive assessment; PPMI, Parkinson’s progression markers initiative; SDMT, symbol digit modality test
Associations of FOG with cognitive functions in the central Chinese cohort
We next assessed the association between FOG and cognitive functions in another cohort including 104 PD patients from central China, of which 63 (60.6%) patients with FOG were identified (eTable 1). Therein, 51 (49.0%) participants were included into longitudinal analyses with an average follow-up of 2.7 ± 1.0 years. Twenty-five non-FOG subjects were conducted to explore the association between FOG progression and cognitive decline, and 6 (24.0%) subjects progressed to FOG. There were no significant differences in demographic characteristics between FOG and non-FOG patients (all p > 0.05).
In the Central Chinese cohort, FOG was evaluated using FOG-Q. The presence of baseline FOG was associated with declines of MoCA (β = − 0.085, p < 0.001) and China-Modified Mini-Mental State Examination (CM-MMSE; β = − 0.036, p = 0.037) according to multivariable-adjusted multiple linear regression models. The worse cognitive functions were more frequently observed in terms of naming, attention, calculation, and delayed memory in subdomains, which showed similar results with continuous FOG-Q scores (eTable 2). On the other hand, the higher FOG-Q scores were associated with greater decreases of MoCA (β = − 0.00056, p = 0.001) and CM-MMSE (β = − 0.00027, p = 0.034), while FOG progression was related to MoCA (β = − 0.00323, p < 0.001) and CM-MMSE (β = − 0.00213, p < 0.001) (eTable 3). The mainly involved domains of cognition were delayed memory and orientation.
Discussion
The present study comprehensively evaluated the associations between FOG and cognitive functions in two prospective cohorts of PD patients. In support of the hypothesis that FOG is a risk factor of cognitive impairment, worse cognitive performances were observed in patients with FOG compared to those without FOG in both cohorts. Moreover, patients with progressive FOG during follow-ups manifested more serious cognitive declines. Of note, FOG was associated with higher levels of cognitive impairment-related biomarkers in CSF and serum. These findings deepen the understanding of the associations between FOG and cognitive impairment, and emphasize that more attention should be paid to cognitive changes in PD patients with FOG.
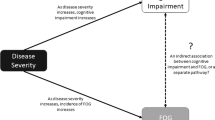
The primary results demonstrated that patients with FOG have worse cognitive performances at baseline and greater cognitive decline at follow-ups compared to patients without FOG. The presence of FOG and FOG progression were associated with deficits in global cognition and specific domains. Our findings are consistent with previous studies that patients with FOG have higher risk and greater decline of cognitive impairment than those without FOG [7,8,9]. However, there are reports showing no significant associations between FOG and cognitive impairment [11, 12]. The possible explanations include the interference of motor function and insensitive cognitive scales [11]. Several studies have reported that dopaminergic nuclei is associated with cognitive impairment as the major impaired lesions of FOG [21]. The diffuse destruction of nigrostriatal and extra-nigrostriatal pathways also play vital roles in the relation between FOG and cognition performances [22]. Several functional magnetic resonance imaging (fMRI) studies discover the reduced structural connectivity in FOG patients between pedunculopontine nucleus and cerebellum [23], thalamus and frontal regions, as well as prefrontal cortex [24]. Furthermore, one multi-tracer positron emission tomography study demonstrates that cortical cholinergic denervation is linked with elevated risk of FOG, especially in patients with concomitant cortical amyloid deposition [25]. These studies suggest the significant roles of FOG in the pathogenesis of cognitive impairment. Nevertheless, it is also raised that FOG occurs via two parallel processes of increasing motor severity and advancing cognitive impairment [12]. Besides, the more serious motor symptoms in FOG group might result in poor performances of speech or writing when making neurophysiological tests. In consequence, it could not reflect the cognitive performances truthfully. In our study, significant correlations survived after adjusting multivariable analysis suggesting that FOG is a risk factor for cognitive impairment.
Fluid biomarkers are valuable and sensitive in early detection of central pathology. Interestingly, our data show that the progression of FOG was significantly associated with cognition-related biomarkers including T-tau, P-tau and NfL in CSF, as well as NfL in serum. This is consistent with previous reports that elevated levels of CSF P-tau and serum NfL accompanied the pathogenesis of cognitive impairment in FOG patients [26, 27]. Apolipoprotein E (APOE) ε4 genotype was reported to be associated with faster FOG progression in PD patients, suggesting a novel genetic risk factor for FOG [28]. The APOE ε4 carriers have higher levels of tau pathology than non-carriers, suggesting that this genotype may affect the neural circuitry associated with FOG and needs further study.
FOG is provoked by the deficits of executive and attention when passing narrow spaces or turning [29]. Structural and functional changes of frontal regions affect both executive and attention [30, 31]. Our findings indicated that FOG was a risk factor for cognitive impairment in individuals with PD, especially in specific cognitive domains of executive and attention. In support of this, neuroimaging studies revealed impairment of executive-attention and visual neural networks in patients with FOG [32], as well as the lower gray volumes or atrophy of frontal and parietal related to executive and visuospatial functions in FOG subjects [33, 34]. Controversies persist about the relationship between FOG and dopaminergic medication. FOG is generally responsive to dopaminergic medication in the most common dopamine-responsive patients, while long-term levodopa treatment may cause FOG deterioration [35, 36]. Levodopa-unresponsive FOG is reported to be associated with executive and visuospatial dysfunction [37]. Levodopa-unresponsive FOG is related to frontostriatal pathway, while levodopa-responsive FOG is associated with posterior cortical regions involved hallucinations. These studies warrant the explorations of FOG drug responsiveness, and more prospective studies are needed to clarify these complex relationships.
Previous studies focused on the cognitive status [10, 38], but PD patients at early stage have slight cognitive decline which may not be detected using simple cognitive classification. The MoCA used in the present study is a sensitive scale for the early detection and diagnosis of cognition impairment [39]. In our central China cohort, FOG-Q was used to evaluate FOG severity and FOG-Q assessment could provide more precise information of the patients with FOG compared to PPMI cohort [15]. More serious FOG is associated with poorer cognitive performances in our cohort, which is consistent with previous studies [40]. A longer duration of follow-up visit of our cohort is in progress to further observe the association between FOG and cognition impairment.
Our study has several limitations. First, the diagnosis of FOG based on the MDS–UPDRS item 2.13 and 3.11 in PPMI was subjective and can be affected by the researchers’ experience. New assessment tools including wearable and virtual reality equipment may be promising. Second, it remained a challenge to eliminate the interfering factors, such as disease duration and severity, and to control motor function discrepancy between FOG and non-FOG groups.
Taken together, our findings suggest that FOG is a risk factor for cognitive impairment in patients with PD. This emphasizes the need for early detection and monitoring of cognitive changes and interventions on cognitive impairments in PD patients with FOG.
Data availability
The clinical data used in this study from PPMI cohort are available at the PPMI website (https://www.ppmi-info.org/access-data-specimens/download-data/), and the data from Central Chinese cohort can be shared on reasonable requests by contacting the corresponding authors.
References
Hely MA et al (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23(6):837–844. https://doi.org/10.1002/mds.21956
Leroi I et al (2012) Cognitive impairment in Parkinson disease: impact on quality of life, disability, and caregiver burden. J Geriatr Psychiatry Neurol 25(4):208–214. https://doi.org/10.1177/0891988712464823
Aarsland D et al (2009) Cognitive impairment in incident, untreated Parkinson disease: the Norwegian ParkWest study. Neurology 72(13):1121–1126. https://doi.org/10.1212/01.wnl.0000338632.00552.cb
Forsaa EB et al (2015) A 12-year population-based study of freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord 21(3):254–258. https://doi.org/10.1016/j.parkreldis.2014.12.020
Huang YF et al (2015) Risk and adverse outcomes of fractures in patients with Parkinson’s disease: two nationwide studies. Osteoporos Int 26(6):1723–1732. https://doi.org/10.1007/s00198-015-3052-y
Factor SA et al (2014) Cognitive correlates of hallucinations and delusions in Parkinson’s disease. J Neurol Sci 347(1–2):316–321. https://doi.org/10.1016/j.jns.2014.10.033
Verbaan D et al (2007) Cognitive impairment in Parkinson’s disease. J Neurol Neurosurg Psychiatry 78(11):1182–1187. https://doi.org/10.1136/jnnp.2006.112367
Poletti M et al (2012) Mild cognitive impairment and cognitive-motor relationships in newly diagnosed drug-naive patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 83(6):601–606. https://doi.org/10.1136/jnnp-2011-301874
Amboni M et al (2010) A two-year follow-up study of executive dysfunctions in parkinsonian patients with freezing of gait at on-state. Mov Disord 25(6):800–802. https://doi.org/10.1002/mds.23033
Lichter DG, Benedict RHB, Hershey LA (2021) Freezing of gait in parkinson’s disease: risk factors, their interactions, and associated nonmotor symptoms. Parkinsons Dis 2021:8857204. https://doi.org/10.1155/2021/8857204
Taximaimaiti R, Wang XP (2021) Comparing the clinical and neuropsychological characteristics of Parkinson’s disease with and without freezing of gait. Front Neurosci 15:660340. https://doi.org/10.3389/fnins.2021.660340
Morris R et al (2020) Cognitive function in people with and without freezing of gait in Parkinson’s disease. NPJ Parkinsons Dis 6:9. https://doi.org/10.1038/s41531-020-0111-7
The Parkinson Progression Marker Initiative (PPMI). Prog Neurobiol, 2011. 95(4): 629–35. https://doi.org/10.1016/j.pneurobio.2011.09.005
Postuma RB et al (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601. https://doi.org/10.1002/mds.26424
Giladi N et al (2009) Validation of the freezing of gait questionnaire in patients with Parkinson’s disease. Mov Disord 24(5):655–661. https://doi.org/10.1002/mds.21745
Kang JH et al (2013) Association of cerebrospinal fluid β-amyloid 1–42, T-tau, P-tau181, and α-synuclein levels with clinical features of drug-naive patients with early Parkinson disease. JAMA Neurol 70(10):1277–1287. https://doi.org/10.1001/jamaneurol.2013.3861
Ray NJ et al (2018) In vivo cholinergic basal forebrain atrophy predicts cognitive decline in de novo Parkinson’s disease. Brain 141(1):165–176. https://doi.org/10.1093/brain/awx310
Stebbins GT et al (2013) How to identify tremor dominant and postural instability/gait difficulty groups with the movement disorder society unified Parkinson’s disease rating scale: comparison with the unified Parkinson’s disease rating scale. Mov Disord 28(5):668–670. https://doi.org/10.1002/mds.25383
Tomlinson CL et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25(15):2649–2653. https://doi.org/10.1002/mds.23429
Kang JH et al (2016) CSF biomarkers associated with disease heterogeneity in early Parkinson’s disease: the Parkinson’s Progression Markers Initiative study. Acta Neuropathol 131(6):935–949. https://doi.org/10.1007/s00401-016-1552-2
Aarsland D et al (2017) Cognitive decline in Parkinson disease. Nat Rev Neurol 13(4):217–231. https://doi.org/10.1038/nrneurol.2017.27
Velseboer DC et al (2013) Prognostic factors of motor impairment, disability, and quality of life in newly diagnosed PD. Neurology 80(7):627–633. https://doi.org/10.1212/WNL.0b013e318281cc99
Schweder PM et al (2010) Connectivity of the pedunculopontine nucleus in parkinsonian freezing of gait. NeuroReport 21(14):914–916. https://doi.org/10.1097/WNR.0b013e32833ce5f1
Fling BW et al (2013) Asymmetric pedunculopontine network connectivity in parkinsonian patients with freezing of gait. Brain 136(Pt 8):2405–2418. https://doi.org/10.1093/brain/awt172
Bohnen NI et al (2014) Extra-nigral pathological conditions are common in Parkinson’s disease with freezing of gait: an in vivo positron emission tomography study. Mov Disord 29(9):1118–1124. https://doi.org/10.1002/mds.25929
Zuo LJ et al (2016) The association between different motor phenotypes and cognitive impairment in Parkinson’s disease and its mechanism. Beijing Med J 38(10):1003–1008. https://doi.org/10.15932/j.0253-9713.2016.10.009
Kim R, Jeon B (2021) Serum neurofilament light chain predicts future freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord 91:102–104. https://doi.org/10.1016/j.parkreldis.2021.08.015
Kim R et al (2020) Apolipoprotein E ε4 genotype and risk of freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord 81:173–178. https://doi.org/10.1016/j.parkreldis.2020.10.033
Nutt JG et al (2011) Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol 10(8):734–744. https://doi.org/10.1016/s1474-4422(11)70143-0
Brugger F et al (2015) Do executive dysfunction and freezing of gait in Parkinson’s disease share the same neuroanatomical correlates? J Neurol Sci 356(1–2):184–187. https://doi.org/10.1016/j.jns.2015.06.046
Tard C et al (2015) Brain metabolic abnormalities during gait with freezing in Parkinson’s disease. Neuroscience 307:281–301. https://doi.org/10.1016/j.neuroscience.2015.08.063
Imamura K, Okayasu N, Nagatsu T (2012) Cerebral blood flow and freezing of gait in Parkinson’s disease. Acta Neurol Scand 126(3):210–218. https://doi.org/10.1111/j.1600-0404.2012.01652.x
Kostic VS et al (2012) Pattern of brain tissue loss associated with freezing of gait in Parkinson disease. Neurology 78(6):409–416. https://doi.org/10.1212/WNL.0b013e318245d23c
Tessitore A et al (2012) Regional gray matter atrophy in patients with Parkinson disease and freezing of gait. AJNR Am J Neuroradiol 33(9):1804–1809. https://doi.org/10.3174/ajnr.A3066
Garcia-Ruiz PJ (2011) Gait disturbances in Parkinson disease. Did freezing of gait exist before levodopa? Historical review. J Neurol Sci 307(1–2):15–17. https://doi.org/10.1016/j.jns.2011.05.019
Koehler PJ, Nonnekes J, Bloem BR (2021) Freezing of gait before the introduction of levodopa. Lancet Neurol 20(2):97. https://doi.org/10.1016/s1474-4422(19)30091-2
Factor SA et al (2014) Freezing of gait subtypes have different cognitive correlates in Parkinson’s disease. Parkinsonism Relat Disord 20(12):1359–1364. https://doi.org/10.1016/j.parkreldis.2014.09.023
Palermo G et al (2019) Freezing of gait and dementia in Parkinsonism: a retrospective case-control study. Brain Behav 9(6):e01247. https://doi.org/10.1002/brb3.1247
Hendershott TR et al (2019) Comparative sensitivity of the MoCA and Mattis Dementia Rating Scale-2 in Parkinson’s disease. Mov Disord 34(2):285–291. https://doi.org/10.1002/mds.27575
Yao Z, Shao Y, Han X (2017) Freezing of gait is associated with cognitive impairment in patients with Parkinson disease. Neurosci Lett 656:126–130. https://doi.org/10.1016/j.neulet.2017.07.004
Acknowledgements
This study was funded by the National Natural Science Foundation of China (Grant numbers 81771376 and 91849121) and the National Natural Science Foundation of Hubei Province (Grant number 2020CFB590). The data used in the preparation of this article were obtained from the PPMI database (ppmi-info.org/data). For updated information on the study, visit ppmi-info.org. PPMI (a public private partnership) is funded by the Michael J. Fox Foundation for Parkinson’s Research and multiple funding partners, including AbbVie, Avid, Biogen, Bristol-Myers Squibb, Covance, GE Healthcare, Genentech, GlaxoSmithKline, Lilly, Lundbeck, Merck, Meso Scale Discovery, Pfizer, Piramal, Roche, Servier, Teva, and UCB.
Author information
Authors and Affiliations
Contributions
XZ and YQ designed and conceptualized the study; YQ, JTL, YPC, QMY, LJY, QXQ, DLW, and JWZ conducted the study. YQ, ZJM, YJX, ZM, and ZX analyzed and extracted the data; YQ, JTL, YPC, and ZX wrote the first draft of the manuscript. All authors have reviewed the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None of the authors have any financial disclosures and conflicts of interest.
Ethical standard statement
This study was approved by the Medical Ethics Committee of Tongji Hospital (Wuhan, China).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qu, Y., Li, J., Chen, Y. et al. Freezing of gait is a risk factor for cognitive decline in Parkinson’s disease. J Neurol 270, 466–476 (2023). https://doi.org/10.1007/s00415-022-11371-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11371-w