Abstract
T lymphocytes are involved in the pathogenesis of Parkinson’s disease (PD), while the heterogeneity of T-cell subpopulations remains elusive. In this study, we analyzed up to 22 subpopulations of T lymphocytes in 115 PD patients and 60 matched healthy controls (HC) using flow cytometry. We found that PD patients exhibited decreased naïve CD8+ T cells (CD3+ CD8+ CD45RA+ CD45RO−) and increased late-differentiated CD4+ T cells (CD3+ CD4+ CD28− CD27−), compared to HC, which were not affected by anti-parkinsonism medication administration. The proportion of naïve CD8+ T cells in PD patients was positively correlated with their severity of autonomic dysfunction and psychiatric complications, but negatively associated with the severity of rapid eye movement and sleep behavior disorder. The proportion of late-differentiated CD4+ T cells was negatively correlated with the onset age of the disease. We further developed individualized PD risk prediction models with high reliability and accuracy on the base of the T lymphocyte subpopulations. These data suggest that peripheral cellular immunity is disturbed in PD patients, and changes in CD8+ T cells and late-differentiated CD4+ T cells are representative and significant. Therefore, we recommend naïve CD8 + and late-differentiated CD4+ T cells as candidates for multicentric clinical study and pathomechanism study of PD.
Similar content being viewed by others
Background
Parkinson’s disease (PD) is a neurodegenerative disease characterized by progressive degeneration of dopaminergic neurons and aggregation of alpha-synuclein (α-syn) in the substantia nigra (SN), which subsequently results in motor impairments [1, 2]. Mounting pieces of evidence implicates neuroinflammation contributing to the pathogenesis of PD. As the major component of the adaptive immune system, abundant T cells appear in the post-mortem brain of PD patients [1], whereas few are present in normal brains[2]. Recent studies have revealed that T cells in PD patients can recognize the specific epitopes derived from α-syn [3, 4]and mediate subsequent robust autoimmune reactions [5,6,7]. Therefore, the characteristics of T cells in the peripheral blood may reflect the pathophysiological changes at the early stage of PD. The prediction and diagnosis of that disease may rely upon identifying T-cell subsets in individuals.
T lymphocytes consist of two major groups: the CD4+ and CD8+ populations. The CD4+ T cells “help” the activity of other cells, while the CD8+ T cells mediate cytotoxicity. Both CD4+ and CD8+ T populations can be subdivided into different subsets according to their surface cluster of differentiation molecules or various functions. Previous pieces of evidence have indicated that infiltrating T cells exert diverse effects on the pathogenesis of PD. In PD patients, the infiltration of nigral CD8+ T cells initiates and propagates the progression of neuronal death and synucleinopathy [8]. Moreover, deficiency of CD4+ T cells in mice prevents the dopaminergic cell loss post 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) administration or α-syn overexpression [1, 9]. However, adoptive transfer of CD3-activated regulatory T cells (Tregs) or specific T cells from copolymer-1-immunized mice into MPTP-treated mice reduced microglia activation and neuron loss in the nigrostriatal system [10]. Although the diverse roles of T cells in the pathogenesis of PD are examined, the heterogeneity of T-cell subpopulations remains elusive.
Impairment in lymphatic vessels or blood–brain barrier was observed in PD [11, 12], which may suggest that intracephalic T-cell distribution is a reflection of that in peripheral blood. Several clinical investigations revealed that in peripheral blood, PD patients have fewer CD3+ and CD4+ T lymphocytes [13,14,15], but more Th17 cells [13, 16] compared to healthy controls (HC). Some studies reported a decrease in naïve T cells [17], Tregs [14, 18, 19], Th1 [20], and CD8+ T cells [18], whereas other studies show an increase in activated T cells [21] and CD8+ T cells [22] in PD patients. Due to relatively small sample sizes, different phenotyping methods, and patients’ recruitment, no consistent conclusion has been drawn so far.
In this study, we devote to uncovering the key T lymphocyte subpopulations associated with PD. To determine the relationship between the various symptoms of PD patients and the specific pattern of T lymphocyte subpopulations in PD condition, we profiled the clinical information of 115 PD patients and 60 HC individuals, and examined 22 T-cell subsets in peripheral blood. We found that PD patients exhibited less naïve CD8+ T (CD8+ Tn) cells and more late-differentiated (LD) CD4+ T cells. Based on our data, we generated nomogram models to predict the PD risk in individuals.
Materials
Participants
Participants were recruited from the Movement Disorder Outpatient of Tongji hospital from Nov 2017 to May 2020. Inclusion criteria: (i) patients with Parkinsonian symptoms aged 40–80 years who met the Movement Disorders Society (MDS) clinical diagnostic criteria for PD [23], diagnosed as clinically established PD or clinically probable PD; (ii) patients who presented modified Hoehn and Yahr (H&Y) rating scale from 1 to 3 stage; (iii) patients could cooperate in completing all the clinical evaluations; (iv) If the anti-parkinsonism medication was taken, the medication must be stable for 8 weeks before baseline. Exclusion criteria: (i) patients had a diagnosis of atypical parkinsonism or other central nervous system diseases; (ii) subjects whose CRP and/or WBC counts were above the upper limit of the normal range (upper limit of the normal range, CRP: 10 mg/L; WBCs: 10 × 109/L); (iii) subjects with autoimmune disease or chronic infections, a history of immunosuppressive treatment and those on anti-inflammatory therapy such as NSAIDs; (iv) subjects were unable to cooperate with the clinical evaluation due to cognitive impairment or clinically significant mood disorder; (v) patients had been taking anti-parkinsonism drugs for less than 8 weeks or had adjusted their dose of anti-parkinsonism drugs within 8 weeks before enrollment. Age- and sex-matched HC were also included at the same time at the same location.
Following enrollment, subjects underwent a complete neurological examination and provided information on their disease states, including treatment history, age of PD onset, course of the disease, and drug administration. The current dose of anti-parkinsonism drugs taken was converted to the levodopa-equivalent daily dose (LEDD). Scales evaluations were conducted by filling in various questionnaires covering demographic information and motor/non-motor features of PD, and supervised by a qualified movement disorder specialist. Motor symptoms such as bradykinesia, rigidity, tremor, postural problems, balance problems, and motor complications were evaluated by the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS), Berg Balance Scale (BBS), Mini version of Balance Evaluation Systems Test (Mini-BEST), and Short Parkinson’s Evaluation Scale/Scales for Outcomes in Parkinson’s disease (SPES/SCOPA). Non-motor symptoms consist of anosmia, constipation, sleep disorders, emotional disorder, cognitive deficiency, autonomic dysfunction, and psychiatric complications. These features were evaluated by the Non-motor symptom scale (NMSS), Hyposmia rating scale (HRS), Constipation Severity Instrument (CSI), Pittsburgh sleep quality index (PSQI), REM sleep behavior disorder screening questionnaire (RBDSQ), Epworth Sleeping Scale (ESS), Restless Leg Syndrome (RLS), Hospital Anxiety and Depression Scale (HAD)-Anxiety part (A)/ Depression part (D), 17-item Hamilton Depression Scale (HAMD-17), Mini-Mental State Examination (MMSE), Scales for Outcomes in Parkinson's disease for Autonomic symptoms (SCOPA-AUT), and Scales for Outcomes in Parkinson’s disease for Psychiatric Complications (SCOPA-PC). The life quality of PD patients was measured by 39-item Parkinson’s Disease Questionnaire (PDQ-39).
This study was approved by the Ethics Committee of Tongji Hospital of Tongji University (Approved ID: KYSB-2017-097). All the participants signed the informed consent before enrollment. The study was performed according to the Declaration of Helsinki and the relevant ethical guidelines for research on humans.
Blood cell analysis and flow cytometric analysis
Peripheral venous blood samples were collected after a fasting night, between 6:00 a.m. and 9:00 a.m., in EDTA-coated tubes. To ensure processing efficiency, no more than two individual blood samples were collected per day. Leukocyte and total lymphocytes analyses were performed immediately after blood sample collection, and were completed by Sysmex-XN A1 automatic hematology analyzer (Sysmex, Kobe, Japan).
For lymphocyte subsets analysis, 2 ml aliquots of whole blood were prepared from each participant and processed immediately to ensure homogeneous treatment. Each sample was divided and every 50 ul aliquots were incubated with a cocktail of different four-color panels fluorescein-conjugated antibody (FITC-PE-PerCP-APC) for targeted immunocytes: B cells (CD3− CD19+), natural killer (NK) cells (CD3− CD16+ CD56+), T cells (CD3+), and 22 types of T-cell subsets, including NKT cells (CD3+ CD16+ CD56+), CD4+ T cells (CD3+ CD4+), CD4+ naïve T (Tn) cells (CD3+ CD4+ CD45RA+ CD45RO−), CD4+ memory T (Tm) cells (CD3+ CD4+ CD45RA− CD45RO+), CD4+ effector memory T cells (Tem) cells (CD3+ CD4+ CD45RO+ CD62L−), CD4+ central memory T (Tcm) cells (CD3+ CD4+ CD45RO+ CD62L+), CD8+ T cells (CD3+ CD8+), CD8+ Tn cells (CD3+ CD8+ CD45RA+ CD45RO−), CD8+ Tm cells (CD3+ CD8+ CD45RA− CD45RO+), CD8+Tem cells (CD3+ CD8+ CD45RO+ CD62L−), CD8+ Tcm cells (CD3+ CD8+ CD45RO+ CD62L+), activated CD4+ T cells (CD38+ HLA-DR+ CD3+ CD4+), activated CD8+ T cells (CD38+ HLA-DR+ CD3+ CD8+), CD4+ regulatory T (Treg) cells (CD4+ CD25+ CD127−), CD8+ Treg cells (CD8+ CD28−), early differentiated (ED) CD4+ T cells (CD3+ CD4+ CD28+ CD27+), medium-differentiated (MD) CD4+ T cells (CD3+ CD4+ CD28+ CD27−), LD CD4+ T cells (CD3+ CD4+ CD28− CD27−), ED CD8+ T cells (CD3+ CD8+ CD28+ CD27+), MD CD8+ T cells (CD3+ CD8+ CD28+ CD27−), LD CD8+ T cells (CD3+ CD8+ CD28− CD27−), and senescent T cells (CD57+ CD3+). The markers used for each individual subset of T cells are also listed in Table 2. After 30 min in the dark at room temperature, erythrocytes were removed by lysis solution (BD, 349,202). Samples were then centrifuged, supernatants were removed, and cells were washed in phosphate-buffered saline (PBS) and resuspended in PBS. Antibodies used in the study are listed in Online Resource 1. Acquisition and data analysis were then performed on a BD Accuri C6 flow cytometer (Becton Dickinson, Milan, Italy) with BD C6 software (version 1.0.264.21). To ensure high-quality and consistent results, the flow cytometry instrument was calibrated daily, and antibody fluorescence intensity was monitored weekly.
Data were analyzed with the BD C6 software (version 1.0.264.21). Unstained samples were used to set voltages for fluorescence channels and single-color controls were set to correct for fluorescence spillover. The gating strategy for lymphocytes using side scatter (SSC) and forward scatter (FSC) according to Salzman et al. [24]. 5000 cells were obtained in the lymphocyte gate to make sure that the same number of cells was used for each sample. All percentage and statistical analyses were performed inside the lymphocytes gate, thus excluding cell debris. The isotype controls were set to inform the gating. The gating strategy is shown in Online Resource 2. The results are finally expressed as the percentage of positive cells (%) in the father group, and the father group is, respectively, remarked on the vertical coordinates of boxplots in Fig. 2.
Statistical analysis
Data are expressed as mean (standard deviation range), median (interquartile range), or percentage depending on the type of data and their distribution. Continuous variables were subjected to Student’s t tests if they fit a normal distribution with homogeneous variances; otherwise, Mann–Whitney tests were used. Differences in categorical variables between groups were tested by the Chi-square test. Multivariate logistic regression analyses were applied to adjust for potential confounders and determine the factors affecting PD diagnosis. A nomogram based on the results of previous multivariable analyses was constructed to predict PD risk. The calibration curve was used to analyze the agreement between the nomogram and actual observation. Confidence intervals were obtained by creating 1000 bootstrap samples from the corresponding cohort and replicating the estimation process. Discrimination was assessed using the concordance index (C-index). Linear regression was used to identify major clinical features of PD patients in response to their lymphocyte changes. Statistical analyses were conducted using the SPSS version 19.0 software (IBM Corporation, Armonk, NY, USA) and R version 3.5.2 (http://www.r-project.org). P < 0.05 was regarded as statistically significant.
Results
Baseline characteristics
We recruited 238 participants in Movement Disorder Outpatient of Tongji hospital, and 63 of them were excluded for inclusion criteria not met (n = 22), exclusion criteria met (n = 14), refused to enroll (n = 21), and incomplete clinical evaluations (n = 6). Finally, a total of 115 PD patients entered the analysis. At the same time, 60 age- and sex-matched HCs were included in the analysis (Fig. 1). Generally, there was no significant difference in age, sex, and BMI between the PD patients and HC individuals. In terms of lifelong habits, more people in the HC group had habits of smoking, alcohol consumption, and tea consumption than that in the PD group, while the rate of coffee consumption and exercise showed no differences between the two groups. Interestingly, the comparison of past medical history between the two groups showed comorbidity that more people in the PD group suffered diabetes after adjusting for multiple covariates such as age, sex, smoking, and alcohol consumption (Table 1).
LD CD4+ T cells and CD8+ Tn cells are independent predictors of PD condition
We investigated the characteristics of T lymphocytes in peripheral blood of 115 PD patients and 60 HC persons. In general, the total lymphocytes descended in the PD group, including both proportion and absolute number levels compared with HC in our cohort (P < 0.05), while the number of leukocytes was similar between the two groups (Online Resource 3). To elucidate the precise changes of lymphocyte subpopulations in PD conditions, we next analyzed 25 types of lymphocytes, including 22 subtypes of T cells. The classifications are based on cell surface markers, focusing on functional and differentiated subpopulations. The distributions of each lymphocyte subpopulation in the PD and the HC groups are shown in Fig. 2. And the alteration of CD8+ Tn cells, LD CD4+ T cells, and ED CD8+ T cells in PD patients reached statistical differences (P < 0.05) in univariate analysis of cell proportions. Compared with HC subjects, LD CD4+ T cells and ED CD8+ T cells were upregulated but CD8+ Tn cells were downregulated in PD patients (Fig. 2), suggesting a redistribution of T lymphocyte subsets in PD condition.
Level of lymphocyte subpopulations in peripheral blood between groups of patients with Parkinson’s disease and healthy controls. a Lymphocyte subpopulations classification strategy used in this study. b Distribution of the major lymphocyte subsets (T cells, B cells, NK cells). c Distribution of CD4+ T lymphocytes, CD8+ T lymphocytes, NKT cells, and senescent T cells. d Distribution of CD4+ T lymphocytes’ functional subpopulations (CD4+ Tn cells, CD4+ Tm cells, CD4+ Tem cells, CD4+ Tcm cells, activated CD4+ T cells, and CD4+ Treg cells). e Distribution of CD4+ T cell differentiated subpopulations (ED CD4+ T cells, MD CD4+ T cells, LD CD4+ T cells). f Distribution of CD8+ T lymphocytes’ functional subpopulations (CD8+ Tn cells, CD8+ Tm cells, CD8+ Tem cells, CD8+ Tcm cells, activated CD8+ T cells and CD8+ Treg cells). g Distribution of CD8+ T cell differentiated subpopulations (ED CD8+ T cells, MD CD8+ T cells, LD CD8+ T cells). Data were presented as a box plot, with the center, box, whiskers, and points corresponding to the median, interquartile range, extremum range, and outliers, respectively. P values were calculated by Student’s t test (variables of CD8+ Tm cells and ED CD8+ T cells) or Mann–Whitney test (variables except for CD8+ Tm cells and ED CD8+ T cells). PD: n = 115, HC: n = 60. * indicates P < 0.05. PD Parkinson’s disease, HC Healthy control, NK Natural killer, Tn Naive T cells, Tm Memory T cells, Tcm Central Memory T cells, Tem Effector Memory T cells, Treg Regulatory T cells, ED Early differentiated, MD Medium-differentiated, LD Late-differentiated
Next, we conducted a logistic regression analysis based on univariate analysis, which shows that the proportion of CD8+ Tn cells (P < 0.05), LD CD4+ T cells (P < 0.05), and ED CD8+ T cells are associated with PD condition, after adjustment for confounding factors, such as diabetes mellitus status, smoking consumption, alcohol consumption, and tea consumption (Table 2). To further confirm the roles of these lymphocyte subsets in independent predictive for PD, we then built logistic regression models based on their absolute cell counts. The models established a firm position of CD8+ Tn cells (P < 0.05) and LD CD4+ T cells (P < 0.05) as independent correlation factors for PD, while the ED CD8+ T cells were eliminated in this model due to the unstable performance (Table 2).
To clarify whether this cellular discrepancy is due to medication administration in PD patients, we further analyzed the peripheral lymphocyte characteristics of drug-naïve patients in the cohort versus those who had been treated with stable medication for 8 weeks. The results showed that the proportion of CD8+ Tn cells and the proportion of LD CD4+ T cells did not differ between those two groups. Moreover, the changes in cell numbers and their proportions shared a similar trend (Online Resource 4). Our data suggest that CD8+ Tn cells and LD CD4+ T cells are potentially critical factors for PD prediction.
The association between T lymphocyte subset indicators and clinical characteristics of PD
To further determine the relevant clinical features of CD8+ Tn cells and LD CD4+ T cells, we used multiple regression models to explore the association between their proportions and characteristics of PD patients (age of disease onset, course of the disease, LEDD, H&Y, scores of motor symptoms scales included MDS-UPDRS, BBS, Mini-BEST, SPES/SCOPA, scores of non-motor symptoms included NMSS, HRS, CSI, PSQI, RBDSQ, ESS, RLS, HAD, HAMD-17, MMSE, SCOPA-AUT, SCOPA-PC, and scores of life quality from PDQ-39). All the features of our PD patients are summarized in Online Resource 5. We found that the proportion of CD8+ Tn cells in peripheral blood were positively correlated with severity of autonomic dysfunction (SCOPA-AUT) (correlation coefficient 0.398, 95% CI 0.119–0.676, P = 0.006) and psychiatric complications (SCOPA-PC) (correlation coefficient 2.883, 95% CI 0.179–5.587, P = 0.037), and negatively associated with severity of RBD (RBDSQ) (correlation coefficient − 1.193, 95% CI − 1.886 to − 0.501, P = 0.001) (adjusted R-squared 0.118, F = 6.061, P = 0.001). And LD CD4+ T cells are negatively correlated with age of disease onset (correlation coefficient -0.428, 95% CI − 0.650 to − 0.206, P < 0.001) (adjusted R-squared 0.106, F = 14.563, P < 0.001) (Fig. 3). These results indicated that clinical phenotyping connects with cellular change, which further exhibited the possibility of using CD8+ Tn cells and LD CD4+ T cells as predictors of PD condition.
The chord diagram shows the normalized coefficients among lymphocyte subpopulations and indicators associated with Parkinson’s disease. The red line represents a positive correlation between the percentage of lymphocyte subsets in the blood and the severity of non-motor symptoms, while the green line represents a negative correlation between the percentage of lymphocyte subsets and the severity of non-motor symptoms or age at onset. The width of the connecting line represents the normalized correlation coefficient. P < 0.05 was regarded as statistically significant. PD Parkinson’s disease, CD8+ Tn cells naïve CD8+ T cells, LD CD4+ T cells late-differentiated CD4+ T cells, SCOPA-AUT Scales for outcomes in Parkinson’s disease for autonomic symptoms, RBDSQ REM sleep behavior disorder screening questionnaire, SCOPA-PC Scales for outcomes in Parkinson’s disease for psychiatric complications
Development of nomograms to assess the relationship between T lymphocyte subsets and PD risk
To quantify the contribution of T lymphocyte subsets in increasing the risk of PD, we developed the nomogram for PD risk prediction by assigning a weighted point to each of the independent risk factors, including the level of CD8+ Tn cells, level of LD CD4+ T cells, and status of diabetes mellitus, smoking, alcohol consumption, and tea consumption. For clinical application, two separate models were constructed for cell proportions and absolute cell counts, respectively. The highest total score of the nomogram contained the cell proportions of 280 points, and the scale of PD risk probability ranged from 0.3 to 0.9. The highest total score of the nomogram contained the cell counts of 160 points, and the scale of PD risk probability ranged from 0.1 to 0.9. A higher total score calculated from the sum of the assigned points for each predictive factor in the nomogram corresponded to a higher risk for the development of PD (Fig. 4). The exact nomogram scores were recorded in Online Resource 6. These models can be developed as visual tools for identifying PD patients who are clinically difficult to diagnose by symptoms.
Nomograms for calculating risk score of Parkinson’s disease in aged 40–80 year subjects. The predictive nomograms for PD risk are developed with diabetes, smoking, alcohol consumption, tea consumption, LD CD4+ T cells, and CD8+ Tn cells. a. The variables of LD CD4+ T cells and CD8+ Tn cells show in a the percentage of LD CD4+ T cells in CD4+ T cells and the percentage of CD8+ Tn cells in CD8+ T cells; b their absolute cells number in peripheral blood. Weight points were assigned for six variables by the vertical line between the top points scale and each variable. The sum of all these scores, plotted on the ‘Total point’ line, corresponds to predictions of PD occurrence probability in aged 40–80 year subjects. PD Parkinson’s disease, CD8+ Tn cells naïve CD8+ T cells, LD CD4+ T cells late-differentiated CD4+ T cells
Furthermore, we conducted calibration and discrimination to estimate the reliability and accuracy of these two nomograms for PD risk prediction in subjects aged 40–80 years. Both plotted calibration curves corresponded to the ideal plots, revealing a favorable agreement on the nomogram estimation and actual observation regarding the probability of PD risk prediction. From the distance of the actual curve to the ideal plot, we noticed that the model that included the absolute number of cells performed better than the model that included the percentage of cells. Both models showed high accuracy, with a C-index of 0.712 (95% CI 0.625–0.786) in the nomogram of cell proportion, and with a C-index of 0.733 (95% CI 0.649–0.803) in the nomogram of cell counts (Fig. 5), suggesting that these nomograms for PD risk prediction are reliable and accurate.
Calibration curves of nomograms estimating Parkinson’s disease risk in aged 40–80 year subjects. a Calibration curves of nomograms included diabetes, smoking, alcohol consumption, tea consumption, percentage of LD CD4+ T cells, and percentage of CD8+ Tn cells. b Calibration curves of nomograms diabetes, smoking, alcohol consumption, tea consumption, counts of LD CD4+ T cells, and counts of CD8+ Tn cells. The horizontal axis represents the nomogram-predicted probability of PD occurrence, and the vertical axis represents the actual PD diagnosis. The red line represents ideal calibration. The black line represents actual calibration, which is shaded with a 95% confidence interval. The intercept and slope of calibration curves, C-index of discrimination ability, and their 95% confidence interval are marked in the upper right corner. C-index concordance index, PD Parkinson’s disease, CD8+ Tn cells naïve CD8+ T cells, LD CD4+ T cells late-differentiated CD4+ T cells
Discussion
T cells play a critical role in the pathogenesis of PD [6, 25]. Since the heterogeneity and plasticity of T cells, it is promising to study the disturbed subpopulations of T lymphocytes in PD. In this study, we investigated up to 22 subsets of peripheral T lymphocytes in 175 participants using flow cytometry. We found that PD patients exhibited decreased CD8+ Tn cells and increased LD CD4+ T cells compared to HC subjects. Moreover, the proportions of CD8+ Tn cells and LD CD4+ T cells were associated with the clinical characteristics of PD. We further generated a predictive nomogram model, which reveals that both these two lymphocytes can be potential indicators of PD condition. The current work identified the key cellular components that contribute to altered immune function in PD, and laid the foundation for exploring biomarkers for disease surveillance or targeted intervention.
T cells at various differentiation stages possess distinct proliferative capacity and cytotoxicity, yet a few studies have addressed the differentiated subsets of T lymphocytes. In this study, we used CD27 and CD28 to discriminate the differentiated subsets of T lymphocytes. CD27 and CD28 are co-stimulatory molecular receptors that play an important role in antigen-specific differentiation [26, 27]. CD28 + CD27 + cells, which represent the early stage of T-cell differentiation, have a high proliferative capacity and a lower cytotoxic effect, while loss of the CD27 and CD28 is associated with the acquisition of the senescent phenotype [28].
Our study identified that LD CD4+ T cells, expressing CD3+ CD4+ CD27− CD28−, increased in PD populations. Notably, increased LD CD4+ T cells are one of the features of senescence [29, 30], which is involved in multiple diseases, especially cytomegalovirus infection [31]. Notably, in neurodegenerative disease, late-differentiated T cells marked with CD28−, significantly expanded in the peripheral blood of patients with Alzheimer’s Disease (AD) [32], implying that PD and AD share a common cell pathology in immunosenescence. However, the function of LD CD4+ T cells remains unclear, despite mediating antigen-specific cytotoxicity against infected target cells and displaying immunosuppressive or regulatory functions in certain conditions [30], Nevertheless, our results suggest that PD is closely correlated to the aging of the adaptive immune system. Since the function of senescence T cells is reversible by the treatment of a supramolecular complex containing AMPK, TAB1, and p38 [33], the LD CD4+ T cells may be a potential target for PD intervention.
Previous studies have investigated functional subpopulations of T lymphocytes, such as naïve T cells [34], memory T cells [17, 34, 35], activated T cells [21], and regulatory T cells [14, 17, 19, 22, 35, 36]in the PD population. Naïve T cells, labeled with the high-molecular-weight isoform of leukocyte common antigen CD45 containing the A exon (CD45RA) [37], represent the ability of the organism to renew T lymphocytes. In our cohort, another subset that was significantly altered in PD patients was CD8+ Tn cell, marked with CD3+ CD8+ CD45RA+ CD45RO−. Compared to HC, PD patients showed a consistent decline of CD8+ Tn cells, which was also independent of the therapeutic agents. This result was in agreement with the latest studies performed in the United States and Mexico separately [38, 39], suggesting the consistent changes of CD8+ Tn cells in PD among different races. As the proliferation of naïve T cells and their differentiation into memory T cells are related to cellular senescence [40], the decrease of CD8+ Tn cells may reflect abnormal aging in PD patients.
CD45RA are replaced by the low-molecular-weight isoform CD45RO after naïve T cells activation, and then, memory T cells are formed [37]. Memory T cells respond to reinvading pathogens quickly and can be further divided into central memory T cells (Tcm) and affect memory T cells (Tem) according to their homing to different tissues [41]. Tcm cells show high proliferative capacity, while Tem cells show high killing capacity. Regulatory T cells are a subset of T cells that control autoimmune responsiveness and play an important role in maintaining the dynamic balance of the body’s immune system. However, we did not observe the significant difference in memory T cells and regulatory T cells between PD patients and the control population. The expression of CD38 and HLA-DR molecules on T lymphocytes represents the activation status of the immune cells. Chiba et al. reported that activated T cells were upregulated in PD patients [21], implying the continuous over-activation of the immune system in PD condition, which may cause immune damage and disease progression. Our study observed a similar upward trend of activated T cells in PD patients, although that change did not reach statistical significance.
The peripheral inflammatory responses correlate with the progression of PD [42,43,44], inferring that the pathological changes in the brain can be reflected in the blood. However, only a small number of studies were performed to investigate the changes of lymphocytes on account of the diverse clinical manifestations [20, 36, 45, 46]. In this study, we evaluated various clinical features of PD and identified independent correlations between lymphocyte subsets and PD symptoms. We then identified several non-motor factors significantly associated with CD8+ Tn cells, which further support the involvement of peripheral inflammation in the non-motor symptoms of PD [47]. In addition, the onset age of PD may also affect the peripheral immune system, such as LD CD4+ cells [48]. Our study provided candidates of cellular markers for clinical applications and potential mechanisms underlying the pathophysiology of PD.
Nomogram is a pictorial representation of statistical models constructed by clinical variables, and is proposed as a means to improve disease prognostication [49]. Recently, it has been applied for survival prediction [50] and the early diagnosis of PD [51]. Using the nomogram, we developed individualized PD risk prediction models including CD8+ Tn cells, LD CD4+ T cells, and independent risk factors such as the status of diabetes mellitus, smoking, alcohol consumption, and tea consumption. According to calibration curves, the nomogram that included absolute cells number performs better than the model included cell proportion in predicting PD risk. To the best of our knowledge, it is the first time that circulation lymphocyte subsets have been incorporated into the nomograms for PD risk prediction. Moreover, this study indicated that lymphocyte subsets in peripheral blood, especially CD8+ Tn cells and LD CD4+ T cells, are promising factors in the prediction of PD. Though we performed the discrimination and calibration, the sample size of our cohort is not large enough to validate the two nomogram models in the internal cohort and no external validation was applied either. Besides, a wide variety of exogenous factors were associated with PD risks, such as anxiety or depression, head injury, serum uric acid, and calcium channel blocker medication [52]. These known or unknown factors were not taken into consideration, which might have resulted in some bias in multivariate regression analyses. In the future, expanding the sample size and validating these nomograms in another cohort of patients at different disease stages are necessary. When possible, prospective cohort studies may be conducted to analyze the causal relationship between the alterations of two identified subsets (CD8+ Tn cells and LD CD4+ T cells) and PD.
Besides, we found that both the proportion and the absolute number of CD8+ Tn cells and LD CD4+ T cells did not differ between drug-naïve patients and drug-treated patients, suggesting that the administration of antiparkinsonian drugs does not affect the peripheral adaptive immunity, similar to the conclusion from a previous study [14]. Indeed, it is difficult to fully exclude the contribution of therapeutic agents to these cellular alterations, as medication and disease progression usually change in parallel. Rigorous prospective cohort studies are essential to clarify the association between antiparkinsonian drugs and peripheral immunity.
Conclusion
In this study, we characterized up to 22 subpopulations of T lymphocytes in PD patients and age-matched healthy subjects. Generally, PD patients exhibit altered CD8+ Tn cells and LD CD4+ T cells in the peripheral blood, associated with their non-motor symptoms and onset age of disease. Moreover, we developed the nomogram models for PD risk prediction, which unveiled the strong relationship between T lymphocyte subsets and PD. In addition, the model that included the absolute number of cells was more reliable in predicting PD risk compared to the model that incorporated two cells percentage. These data suggest that peripheral cellular immunity is disturbed in PD patients, and the two lymphocyte subsets are important for PD prediction. Last but not least, we consider CD8+ Tn cells and LD CD4+ T cells as candidates for multicentric clinical study and underlying pathomechanism study of PD.
Abbreviations
- PD:
-
Parkinson’s disease
- HC:
-
Healthy controls
- LEDD:
-
Levodopa-equivalent daily dose
- MDS-UPDRS:
-
Movement Disorder Society Unified Parkinson’s Disease Rating Scale
- BBS:
-
Berg Balance Scale
- Mini-BEST:
-
Mini version of Balance Evaluation Systems Test
- SPES/SCOPA:
-
Short Parkinson’s Evaluation Scale/Scales for Outcomes in Parkinson’s disease
- NMSS:
-
Non-motor Symptom Scale
- HRS:
-
Hyposmia Rating Scale
- CSI:
-
Constipation Severity Instrument
- PSQI:
-
Pittsburgh Sleep Quality Index
- RBDSQ:
-
REM sleep Behavior Disorder Screening Questionnaire
- ESS:
-
Epworth Sleeping Scale
- RLS:
-
Restless Leg Syndrome
- HAD-A/D:
-
Hospital Anxiety and Depression Scale-Anxiety part/Depression part
- HAMD-17:
-
17-Item Hamilton Depression Scale
- MMSE:
-
Mini-mental State Examination
- SCOPA-AUT:
-
Scales for Outcomes in Parkinson's disease for Autonomic symptoms
- SCOPA-PC:
-
Scales for Outcomes in Parkinson's disease for Psychiatric Complications
- PDQ-39:
-
39-Item Parkinson’s Disease Questionnaire
- NK:
-
Natural killer
- Tn:
-
Naïve T cells
- Tm:
-
Memory T cells
- Tcm:
-
Central memory T cells
- Tem:
-
Effector memory T cells
- ED:
-
Early-differentiated
- MD:
-
Medium-differentiated
- LD:
-
Late-differentiated
References
Brochard V, Combadiere B, Prigent A, Laouar Y, Perrin A, Beray-Berthat V, Bonduelle O, Alvarez-Fischer D, Callebert J, Launay JM, Duyckaerts C, Flavell RA, Hirsch EC, Hunot S (2009) Infiltration of CD4+ lymphocytes into the brain contributes to neurodegeneration in a mouse model of Parkinson disease. J Clin Invest 119(1):182–192. https://doi.org/10.1172/JCI36470
Pasciuto E, Burton OT, Roca CP, Lagou V, Rajan WD, Theys T, Mancuso R, Tito RY, Kouser L, Callaerts-Vegh Z, de la Fuente AG, Prezzemolo T, Mascali LG, Brajic A, Whyte CE, Yshii L, Martinez-Muriana A, Naughton M, Young A, Moudra A, Lemaitre P, Poovathingal S, Raes J, De Strooper B, Fitzgerald DC, Dooley J, Liston A (2020) Microglia require CD4 T cells to complete the fetal-to-adult transition. Cell 182(3):625–640. https://doi.org/10.1016/j.cell.2020.06.026 (e24)
Sulzer D, Alcalay RN, Garretti F, Cote L, Kanter E, Agin-Liebes J, Liong C, McMurtrey C, Hildebrand WH, Mao X, Dawson VL, Dawson TM, Oseroff C, Pham J, Sidney J, Dillon MB, Carpenter C, Weiskopf D, Phillips E, Mallal S, Peters B, Frazier A, Lindestam Arlehamn CS, Sette A (2017) T cells from patients with Parkinson’s disease recognize alpha-synuclein peptides. Nature 546(7660):656–661. https://doi.org/10.1038/nature22815
Lindestam Arlehamn CS, Dhanwani R, Pham J, Kuan R, Frazier A, Rezende Dutra J, Phillips E, Mallal S, Roederer M, Marder KS, Amara AW, Standaert DG, Goldman JG, Litvan I, Peters B, Sulzer D, Sette A (2020) alpha-Synuclein-specific T cell reactivity is associated with preclinical and early Parkinson’s disease. Nat Commun 11(1):1875. https://doi.org/10.1038/s41467-020-15626-w
Theodore S, Cao S, McLean PJ, Standaert DG (2008) Targeted overexpression of human alpha-synuclein triggers microglial activation and an adaptive immune response in a mouse model of Parkinson disease. J Neuropathol Exp Neurol 67(12):1149–1158. https://doi.org/10.1097/NEN.0b013e31818e5e99
Garretti F, Agalliu D, Lindestam Arlehamn CS, Sette A, Sulzer D (2019) Autoimmunity in Parkinson’s disease: the role of α-Synuclein-Specific T cells. Front Immunol 10:303. https://doi.org/10.3389/fimmu.2019.00303
Williams GP, Schonhoff AM, Jurkuvenaite A, Gallups NJ, Standaert DG, Harms AS (2021) CD4 T cells mediate brain inflammation and neurodegeneration in a mouse model of Parkinson’s disease. Brain 144(7):2047–2059. https://doi.org/10.1093/brain/awab103
Galiano-Landeira J, Torra A, Vila M, Bove J (2020) CD8 T cell nigral infiltration precedes synucleinopathy in early stages of Parkinson’s disease. Brain 143(12):3717–3733. https://doi.org/10.1093/brain/awaa269
Williams GP, Schonhoff AM, Jurkuvenaite A, Gallups NJ, Standaert DG, Harms AS (2021) CD4 T cells mediate brain inflammation and neurodegeneration in a mouse model of Parkinson disease. Brain. https://doi.org/10.1093/brain/awab103
Reynolds AD, Banerjee R, Liu J, Gendelman HE, Mosley RL (2007) Neuroprotective activities of CD4+CD25+ regulatory T cells in an animal model of Parkinson’s disease. J Leukoc Biol 82(5):1083–1094. https://doi.org/10.1189/jlb.0507296
Kortekaas R, Leenders KL, van Oostrom JC, Vaalburg W, Bart J, Willemsen AT, Hendrikse NH (2005) Blood-brain barrier dysfunction in Parkinsonian midbrain in vivo. Ann Neurol 57(2):176–179. https://doi.org/10.1002/ana.20369
Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, Derecki NC, Castle D, Mandell JW, Lee KS, Harris TH, Kipnis J (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523(7560):337–341. https://doi.org/10.1038/nature14432
Chen Y, Qi B, Xu W, Ma B, Li L, Chen Q, Qian W, Liu X, Qu H (2015) Clinical correlation of peripheral CD4+cell subsets, their imbalance and Parkinson’s disease. Mol Med Rep 12(4):6105–6111. https://doi.org/10.3892/mmr.2015.4136
Kustrimovic N, Comi C, Magistrelli L, Rasini E, Legnaro M, Bombelli R, Aleksic I, Blandini F, Minafra B, Riboldazzi G, Sturchio A, Mauri M, Bono G, Marino F, Cosentino M (2018) Parkinson’s disease patients have a complex phenotypic and functional Th1 bias: cross-sectional studies of CD4+ Th1/Th2/T17 and Treg in drug-naive and drug-treated patients. J Neuroinflammation 15(1):205. https://doi.org/10.1186/s12974-018-1248-8
Jiang S, Gao H, Luo Q, Wang P, Yang X (2017) The correlation of lymphocyte subsets, natural killer cell, and Parkinson’s disease: a meta-analysis. Neurol Sci 38(8):1373–1380. https://doi.org/10.1007/s10072-017-2988-4
Chen S, Liu Y, Niu Y, Xu Y, Zhou Q, Xu X, Wang J, Yu M (2017) Increased abundance of myeloid-derived suppressor cells and Th17 cells in peripheral blood of newly-diagnosed Parkinson’s disease patients. Neurosci Lett 648:21–25. https://doi.org/10.1016/j.neulet.2017.03.045
Saunders JA, Estes KA, Kosloski LM, Allen HE, Dempsey KM, Torres-Russotto DR, Meza JL, Santamaria PM, Bertoni JM, Murman DL, Ali HH, Standaert DG, Mosley RL, Gendelman HE (2012) CD4+ regulatory and effector/memory T cell subsets profile motor dysfunction in Parkinson’s disease. J Neuroimmune Pharmacol 7(4):927–938. https://doi.org/10.1007/s11481-012-9402-z
Gruden MA, Sewell RD, Yanamandra K, Davidova TV, Kucheryanu VG, Bocharov EV, Bocharova OA, Polyschuk VV, Sherstnev VV, Morozova-Roche LA (2011) Immunoprotection against toxic biomarkers is retained during Parkinson’s disease progression. J Neuroimmunol 233(1–2):221–227. https://doi.org/10.1016/j.jneuroim.2010.12.001
Rocha NP, Assis F, Scalzo PL, Vieira ELM, Barbosa IG, de Souza MS, Christo PP, Reis HJ, Teixeira AL (2018) Reduced activated T lymphocytes (CD4+CD25+) and plasma levels of cytokines in Parkinson’s disease. Mol Neurobiol 55(2):1488–1497. https://doi.org/10.1007/s12035-017-0404-y
Niwa F, Kuriyama N, Nakagawa M, Imanishi J (2012) Effects of peripheral lymphocyte subpopulations and the clinical correlation with Parkinson’s disease. Geriatr Gerontol Int 12(1):102–107. https://doi.org/10.1111/j.1447-0594.2011.00740.x
Chiba S, Matsumoto H, Saitoh M, Kasahara M, Matsuya M, Kashiwagi M (1995) A correlation study between serum adenosine deaminase activities and peripheral lymphocyte subsets in Parkinson’s disease. J Neurol Sci 132(2):170–173. https://doi.org/10.1016/0022-510x(95)00136-p
Baba Y, Kuroiwa A, Uitti RJ, Wszolek ZK, Yamada T (2005) Alterations of T-lymphocyte populations in Parkinson disease. Parkinsonism Relat Disord 11(8):493–498. https://doi.org/10.1016/j.parkreldis.2005.07.005
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601. https://doi.org/10.1002/mds.26424
Salzman GC, Crowell JM, Martin JC, Trujillo TT, Romero A, Mullaney PF, LaBauve PM (1975) Cell classification by laser light scattering: identification and separation of unstained leukocytes. Acta Cytol 19(4):374–377
Stone DK, Reynolds AD, Mosley RL, Gendelman HE (2009) Innate and adaptive immunity for the pathobiology of Parkinson’s disease. Antioxid Redox Signal 11(9):2151–2166. https://doi.org/10.1089/ARS.2009.2460
Harding FA, McArthur JG, Gross JA, Raulet DH, Allison JP (1992) CD28-mediated signalling co-stimulates murine T cells and prevents induction of anergy in T-cell clones. Nature 356(6370):607–609. https://doi.org/10.1038/356607a0
Hendriks J, Gravestein LA, Tesselaar K, van Lier RA, Schumacher TN, Borst J (2000) CD27 is required for generation and long-term maintenance of T cell immunity. Nat Immunol 1(5):433–440. https://doi.org/10.1038/80877
Banica L, Vlaicu O, Jipa R, Abagiu A, Nicolae I, Neaga E, Otelea D, Paraschiv S (2021) Exhaustion and senescence of CD4 and CD8 T cells that express co-stimulatory molecules CD27 and CD28 in subjects that acquired HIV by drug use or by sexual route. Germs 11(1):66–77. https://doi.org/10.18683/germs.2021.1242
Fletcher JM, Vukmanovic-Stejic M, Dunne PJ, Birch KE, Cook JE, Jackson SE, Salmon M, Rustin MH, Akbar AN (2005) Cytomegalovirus-specific CD4+ T cells in healthy carriers are continuously driven to replicative exhaustion. J Immunol 175(12):8218–8225. https://doi.org/10.4049/jimmunol.175.12.8218
Strioga M, Pasukoniene V, Characiejus D (2011) CD8+ CD28− and CD8+ CD57+ T cells and their role in health and disease. Immunology 134(1):17–32. https://doi.org/10.1111/j.1365-2567.2011.03470.x
Tovar-Salazar A, Patterson-Bartlett J, Jesser R, Weinberg A (2010) Regulatory function of cytomegalovirus-specific CD4+CD27−CD28− T cells. Virology 398(2):158–167. https://doi.org/10.1016/j.virol.2009.11.038
Barbe-Tuana F, Funchal G, Schmitz CRR, Maurmann RM, Bauer ME (2020) The interplay between immunosenescence and age-related diseases. Semin Immunopathol. https://doi.org/10.1007/s00281-020-00806-z
Akbar AN, Henson SM, Lanna A (2016) Senescence of T lymphocytes: implications for enhancing human immunity. Trends Immunol 37(12):866–876. https://doi.org/10.1016/j.it.2016.09.002
Fiszer U, Mix E, Fredrikson S, Kostulas V, Link H (1994) Parkinson’s disease and immunological abnormalities: increase of HLA-DR expression on monocytes in cerebrospinal fluid and of CD45RO+ T cells in peripheral blood. Acta Neurol Scand 90(3):160–166. https://doi.org/10.1111/j.1600-0404.1994.tb02699.x
Stevens CH, Rowe D, Morel-Kopp MC, Orr C, Russell T, Ranola M, Ward C, Halliday GM (2012) Reduced T helper and B lymphocytes in Parkinson’s disease. J Neuroimmunol 252(1–2):95–99. https://doi.org/10.1016/j.jneuroim.2012.07.015
Cen L, Yang C, Huang S, Zhou M, Tang X, Li K, Guo W, Wu Z, Mo M, Xiao Y, Chen X, Yang X, Huang Q, Chen C, Qu S, Xu P (2017) Peripheral lymphocyte subsets as a marker of Parkinson’s disease in a Chinese population. Neurosci Bull 33(5):493–500. https://doi.org/10.1007/s12264-017-0163-9
Henson SM, Riddell NE, Akbar AN (2012) Properties of end-stage human T cells defined by CD45RA re-expression. Curr Opin Immunol 24(4):476–481. https://doi.org/10.1016/j.coi.2012.04.001
Yan Z, Yang W, Wei H, Dean MN, Standaert DG, Cutter GR, Benveniste EN, Qin H (2021) Dysregulation of the adaptive immune system in patients with early-stage Parkinson disease. Neurol Neuroimmunol Neuroinflamm. https://doi.org/10.1212/NXI.0000000000001036
Alvarez-Luquin DD, Guevara-Salinas A, Arce-Sillas A, Espinosa-Cardenas R, Leyva-Hernandez J, Montes-Moratilla EU, Adalid-Peralta L (2021) Increased Tc17 cell levels and imbalance of naive/effector immune response in Parkinson’s disease patients in a two-year follow-up: a case control study. J Transl Med 19(1):378. https://doi.org/10.1186/s12967-021-03055-2
Goronzy JJ, Fang F, Cavanagh MM, Qi Q, Weyand CM (2015) Naive T cell maintenance and function in human aging. J Immunol 194(9):4073–4080. https://doi.org/10.4049/jimmunol.1500046
Mueller SN, Gebhardt T, Carbone FR, Heath WR (2013) Memory T cell subsets, migration patterns, and tissue residence. Annu Rev Immunol 31:137–161. https://doi.org/10.1146/annurev-immunol-032712-095954
Nissen SK, Shrivastava K, Schulte C, Otzen DE, Goldeck D, Berg D, Moller HJ, Maetzler W, Romero-Ramos M (2019) Alterations in blood monocyte functions in Parkinson’s disease. Mov Disord 34(11):1711–1721. https://doi.org/10.1002/mds.27815
Yazdani S, Mariosa D, Hammar N, Andersson J, Ingre C, Walldius G, Fang F (2019) Peripheral immune biomarkers and neurodegenerative diseases: a prospective cohort study with 20 years of follow-up. Ann Neurol 86(6):913–926. https://doi.org/10.1002/ana.25614
Sun C, Yu W, Zhao Z, Song C, Liu Y, Jia G, Wang X, Liu Y (2019) Peripheral humoral immune response is associated with the non-motor symptoms of Parkinson’s disease. Front Neurosci 13:1057. https://doi.org/10.3389/fnins.2019.01057
Zhang S, Sun C, Zhang L, Cen L, Mo M, Liu Z, Huang W, Zhu F, Kang P, Chen Z, Yi L, Xu P (2014) Clinical analysis of subpopulation of peripheral T and B lymphocytes in Chinese Parkinson’s disease patients. Zhonghua Yi Xue Za Zhi 94(47):3726–3730
Sun C, Zhao Z, Yu W, Mo M, Song C, Si Y, Liu Y (2019) Abnormal subpopulations of peripheral blood lymphocytes are involved in Parkinson’s disease. Ann Transl Med 7(22):637. https://doi.org/10.21037/atm.2019.10.105
Menza M, Dobkin RD, Marin H, Mark MH, Gara M, Bienfait K, Dicke A, Kusnekov A (2010) The role of inflammatory cytokines in cognition and other non-motor symptoms of Parkinson’s disease. Psychosomatics 51(6):474–479. https://doi.org/10.1176/appi.psy.51.6.474
Jiang S, Wang Y, Gao H, Luo Q, Wang D, Li Y, Yong Y, Yang X (2019) Cell ratio differences in peripheral blood between early- and late-onset Parkinson’s disease: a case-control study. Biomed Res Int 2019:2072635. https://doi.org/10.1155/2019/2072635
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16(4):e173–e180. https://doi.org/10.1016/S1470-2045(14)71116-7
Tang Y, Wang J, Chen G, Ye W, Yan N, Feng Z (2021) A simple-to-use web-based calculator for survival prediction in Parkinson’s disease. Aging (Albany NY) 13(4):5238–5249. https://doi.org/10.18632/aging.202443
Shu Z, Pang P, Wu X, Cui S, Xu Y, Zhang M (2020) An integrative nomogram for identifying early-stage Parkinson’s disease using non-motor symptoms and white matter-based radiomics biomarkers from whole-brain MRI. Front Aging Neurosci 12:548616. https://doi.org/10.3389/fnagi.2020.548616
Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP (2016) Environmental risk factors and Parkinson’s disease: an umbrella review of meta-analyses. Parkinsonism Relat Disord 23:1–9. https://doi.org/10.1016/j.parkreldis.2015.12.008
Acknowledgements
We would like to thank Prof. Yi Eve Sun for technical guidance, Dr. Longbing Ren and Dr. Kunshan Zhang for analysis assistance, and Dr. Bolin Zheng and Dr. Yunping Song for revising the manuscript.
Funding
This study was sponsored by the National Key R&D Program of China (2018YFC1314700, 2018YFA0108000), National Natural Science Foundation of China (82172545, 81873779, 81974196), Program of Shanghai Academic Research Leader (20XD1403400), Shanghai Sailing Program (22YF1442100) and Fundamental Research Funds for the Central Universities (22120180511).
Author information
Authors and Affiliations
Contributions
LJ and QG contributed to the conception and design of the study. YH, KW, and ZZ conducted clinical evaluation. RY, LP, and TZ collected samples and conducted flow cytometry analysis. AL and RH recruited subjects. LJ and ZN supervised the project. YH performed the statistical analysis and wrote the first draft of the manuscript. All authors contributed to manuscript revision, and read and approved the submitted version.
Corresponding authors
Ethics declarations
Conflicts of interest
All the authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Tongji Hospital of Tongji University (Approved ID: KYSB-2017-097). All the participants signed informed consent before enrollment. The study was performed according to the Declaration of Helsinki and the relevant ethical guidelines for research on humans.
Supplementary Information
Below is the link to the electronic supplementary material.
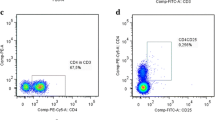
Online Resource 2. Gating strategy used in flow cytometric analysis for evaluating the proportions of each lymphocyte subpopulations in peripheral blood. a
Dotplot of size FSC vs SSA for lymphocytes, inside P2 gate. b Dotplot of CD3 vs CD19, inside lymphocytes gate, where Q1-UL represents B cells (CD3- CD19+). c Dotplot of CD3 vs CD(16+ 56), inside lymphocytes gate, where Q1-UL represents NK cells (CD3- CD(16+ 56)+) and Q1-UR represents NKT cells (CD3+ CD(16+ 56)+). d Dotplot of CD3 vs SSC, inside lymphocytes gate, where R3 represents T cells (CD3+). e Dotplot of CD57 vs CD3, inside lymphocytes gate, where U4-UR represents senescent T cells (CD3+ CD57+). f Dotplot of CD3 vs CD4, inside lymphocytes gate, where Q4-UR represents CD4+ T cells (CD3+CD4+). g Dotplot of CD8 vs CD3, inside lymphocytes gate, where Q2-UR represents CD8+ T cells (CD3+ CD8+). h Dotplot of CD8 vs CD28, inside lymphocytes gate, where Q1-UR represents CD8+ Treg cells (CD8+ CD28+). i, j The gating strategy for CD4+ Treg cells. i CD4+ T cells were gated by CD4 and SSC in R8. j Dotplot of CD127 vs CD25, inside CD4+ T cells gate, where Q14-UL represents CD4+ Treg cells (CD4+ CD25+ CD27-). k–m The gating strategy for naïve T cells and memory T cells. k CD8+ T cells were gated by CD3 and CD8 in R1, while the gate of R5 presents CD4+ T cells. l Dotplot of CD45RA vs CD45RO, inside CD8+ T cells gate, where Q8-UL represents CD8+ Tm cells (CD3+ CD8+ CD45RA- CD45RO+) and Q8-LR represents CD8+ Tn cells (CD3+ CD8+ CD45RA+ CD45RO-). m Dotplot of CD45RA vs CD45RO, inside CD4+ T cells gate, where Q9-UL represents CD4+ Tm cells (CD3+ CD4+ CD45RA- CD45RO+) and Q9-LR represents CD4+ Tn cells (CD3+ CD8+ CD45RA+ CD45RO-). n–p The gating strategy for Tem cells and Tcm cells. n CD8+ T cells were gated by CD3 and CD8 in R6, while the gate of R7 presents CD4+ T cells. o Dotplot of CD62L vs CD45RO, inside CD8+ T cells gate, where Q6-UL represents CD8+ Tem cells (CD3+ CD8+ CD45RO+ CD62L-) and Q6-UR represents CD8+ Tcm cells (CD3+ CD8+ CD45RO+ CD62L+). p Dotplot of CD62L vs CD45RO, inside CD4+ T cells gate, where Q7-UL represents CD4+ Tem cells (CD3+ CD4+ CD45RO+ CD62L-) and Q7-UR represents CD4+ Tcm cells (CD3+ CD4+ CD45RO+ CD62L+). q–s The gating strategy for activated T cells. q CD8+ T cells were gated by CD3 and CD8 in R1, while the gate of R5 presents CD4+ T cells. r Dotplot of CD38 vs HLA-DR, inside CD8+ T cells gate, where Q8-UR represents activated CD8+ T cells (CD3+ CD8+ CD38+ HLA-DR+). s Dotplot of CD38 vs HLA-DR, inside CD4+ T cells gate, where Q9-UR represents activated CD4+ T cells (CD3+ CD4+ CD38+ HLA-DR+). t–v The gating strategy for differentiated subgroups of T cells. t CD8+ T cells were gated by CD3 and CD8 in R6, while the gate of R7 presents CD4+ T cells. u Dotplot of CD28 vs CD27, inside CD8+ T cells gate, where Q6-UR represents ED CD8+ T cells (CD3+ CD8+ CD28+ CD27+), Q6-LR represents MD CD8+ T cells (CD3+ CD8+ CD28+ CD27-) and Q6-LL represents LD CD8+ T cells (CD3+ CD8+ CD28- CD27-). v Dotplot of CD28 vs CD27, inside CD4+ T cells gate, where Q7-UR represents ED CD4+ T cells (CD3+ CD4+ CD28+ CD27+), Q7-LR represents MD CD4+ T cells (CD3+ CD4+ CD28+ CD27-) and Q7-LL represents LD CD4+ T cells (CD3+ CD4+ CD28- CD27-) (TIF 5457 KB)
Online Resource 3. Level of leukocyte and lymphocyte in peripheral blood between groups of patients with Parkinson’s disease and healthy controls. a
Number of leukocytes. b Percentage of lymphocytes. c Number of lymphocytes. Data were presented as a box plot, with the center, box, and whiskers, corresponding to the median, interquartile range, and extremum range, respectively. P-values were calculated by Student’s t-test (variable of Lymphocyte (%)) or Mann-Whitney test (variable of Leukocyte(×1012/L) and Lymphocyte (×109/L)). PD: n=115, HC: n=60. * indicates P<0.05, ** indicates P<0.01. PD Parkinson’s disease, HC healthy control (PDF 434 KB)
Online Resource 4. The difference in the percentage of T lymphocyte subpopulations between drug-naïve patients and drug-treated patients with Parkinson’s disease. a
Scatter plot of percentage of CD8+ Tn cells and LD CD4+ T cells. b Scatter plot of the absolute number of CD8+ Tn cells and LD CD4+ T cells. Data are presented as the median and standard error of mean in the scatter plot and are compared with a Mann-Whitney test. Drug-naïve patients: n=25, Drug-treated patients: n=90. CD8+ Tn cells, naïve CD8+ T cells. LD CD4+ T cells late-differentiated CD4+ T cells (PDF 148 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
He, Y., Peng, K., Li, R. et al. Changes of T lymphocyte subpopulations and their roles in predicting the risk of Parkinson’s disease. J Neurol 269, 5368–5381 (2022). https://doi.org/10.1007/s00415-022-11190-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11190-z