Abstract
Background and purpose
Seizures represent a core symptom of autoimmune encephalitides with specific therapeutic issues. To date, patients with new-onset seizures or established epilepsy are not systematically tested for autoimmune antibodies. We aimed to identify clinical and paraclinical criterion that could help to select patients requiring additional autoimmune antibodies serum and cerebrospinal fluid (CSF) detection.
Methods
In this retrospective single center study from the French Salpêtrière Hospital, data from 286 adult patients with epilepsy who received an autoantibody assay for the first time were analyzed. All patients were evaluated at our institution between January 2007 and December 2018 for assessment of new-onset epilepsy (n = 90) or established epilepsy (n = 196). We only analyzed patients that were screened for autoimmune antibodies. Demographic, clinical and neuroimaging measures were compared between patients with and without autoimmune encephalitis using Fisher’s exact test for categorical variables and Welch’s t test for continuous variables. Our primary goal was to identify significant factors that differentiated patients with and without autoimmune encephalitis.
Results
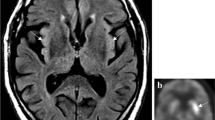
We identified 27 patients with autoimmune epilepsy (9.4% of the patients who had been tested for autoantibodies). The significant factors differentiating patients with and without autoimmune encephalitis were: (i) the existence of a new-onset focal epilepsy + (e.g., newly diagnosed epilepsy < 6 months associated with additional symptoms, mainly cognitive or psychiatric symptoms), (ii) the presence of faciobrachial dystonic seizures very suggestive of anti- Leucine-rich glioma inactivated 1 (LGI1) encephalitis, and (iii) the presence of magnetic resonance imaging (MRI) abnormalities suggestive of encephalitis.
Conclusion
New-onset focal seizures combined with cognitive or psychiatric symptoms support the test for autoimmune antibodies. Further clinical already known red flags for an autoimmune origin are the presence of faciobrachial dystonic seizures and MRI signal changes consistent with encephalitis. On the other hand, isolated new-onset seizures and chronic epilepsy, even with associated symptoms, seem rarely linked to autoimmune encephalitis and should not lead to systematic testing.



Similar content being viewed by others
Data availability
Anonymized data will be shared by request from any qualified investigator.
Code availability
Text and cover letter: Microsoft word.
References
Fisher RS, Acevedo C, Arzimanoglou A et al (2014) ILAE official report: a practical clinical definition of epilepsy. Epilepsia 55:475–482. https://doi.org/10.1111/epi.12550
Scheffer IE, Berkovic S, Capovilla G et al (2017) ILAE classification of the epilepsies: position paper of the ILAE commission for classification and terminology. Epilepsia 58:512–521. https://doi.org/10.1111/epi.13709
De Bruijn MAAM, van Sonderen A, van Coevorden-Hameete MH et al (2019) Evaluation of seizure treatment in anti-LGI1, anti-NMDAR, and anti-GABABR encephalitis. Neurology 92:e2185–e2196. https://doi.org/10.1212/WNL.0000000000007475
Newman MP, Blum S, Wong RCW et al (2016) Autoimmune encephalitis. Intern Med J 46:148–157. https://doi.org/10.1111/imj.12974
Graus F, Titulaer MJ, Balu R et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404. https://doi.org/10.1016/S1474-4422(15)00401-9
Dubey D, Singh J, Britton JW, Pittock SJ (2017) Predictive models in the diagnosis and treatment of autoimmune epilepsy. Epilepsia 58:1181–1189. https://doi.org/10.1111/epi.13797
Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, Sørensen HT, von Elm E, Langan SM, The RECORD Working Committee (2015) The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. https://doi.org/10.1371/journal.pmed.1001885
Macher S, Zimprich F, De Simoni D, Höftberger R, Rommer PS (2018) Management of autoimmune encephalitis: an observational monocentric study of 38 patients. Front Immunol. https://doi.org/10.3389/fimmu.2018.02708
Dalmau J, Gleichman AJ, Hughes EG et al (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098. https://doi.org/10.1016/S1474-4422(08)70224-2
Dubey D, Pittock SJ, Kelly CR et al (2018) Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis: autoimmune encephalitis. Ann Neurol 83:166–177. https://doi.org/10.1002/ana.25131
Brenner T, Sills GJ, Hart Y et al (2013) Prevalence of neurologic autoantibodies in cohorts of patients with new and established epilepsy. Epilepsia 54:1028–1035. https://doi.org/10.1111/epi.12127
Dubey D, Alqallaf A, Hays R et al (2017) Neurological autoantibody prevalence in epilepsy of unknown etiology. JAMA Neurol 74:397–402. https://doi.org/10.1001/jamaneurol.2016.5429
Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA (2012) the frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California encephalitis project. Clin Infect Dis 54:899–904. https://doi.org/10.1093/cid/cir1038
Van Sonderen A, Petit-Pedrol M, Dalmau J, Titulaer MJ (2017) The value of LGI1, Caspr2 and voltage-gated potassium channel antibodies in encephalitis. Nat Rev Neurol 13:290–301. https://doi.org/10.1038/nrneurol.2017.43
Dubey D, Samudra N, Gupta P et al (2015) Retrospective case series of the clinical features, management and outcomes of patients with autoimmune epilepsy. Seizure 29:143–147. https://doi.org/10.1016/j.seizure.2015.04.007
Scheer S, John RM (2016) Anti–N-methyl-D-aspartate receptor encephalitis in children and adolescents. J Pediatr Health Care 30:347–358. https://doi.org/10.1016/j.pedhc.2015.09.004
Lai M, Huijbers MGM, Lancaster E et al (2010) Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol 9:776–785. https://doi.org/10.1016/S1474-4422(10)70137-X
Titulaer MJ, McCracken L, Gabilondo I et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165. https://doi.org/10.1016/S1474-4422(12)70310-1
Gresa-Arribas N, Ariño H, Martínez-Hernández E et al (2015) Antibodies to inhibitory synaptic proteins in neurological syndromes associated with glutamic acid decarboxylase autoimmunity. PLoS ONE. https://doi.org/10.1371/journal.pone.0121364
Irani SR, Michell AW, Lang B et al (2011) Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol 69:892–900. https://doi.org/10.1002/ana.22307
Daif A, Lukas RV, Issa NP et al (2018) Antiglutamic acid decarboxylase 65 (GAD65) antibody-associated epilepsy. Epilepsy Behav 80:331–336. https://doi.org/10.1016/j.yebeh.2018.01.021
de Bruijn MAAM, Bastiaansen AEM, Mojzisova H et al (2021) Antibodies contributing to focal epilepsy signs and symptoms score. Ann Neurol 89:698–710. https://doi.org/10.10002/ana.26013
Britton JW, Dalmau J (2019) Recognizing autoimmune encephalitis as a cause of seizures treating cause and not effect. Neurology 92:877–878. https://doi.org/10.1212/WNL.0000000000007444
Geis C, Planaguma J, Carreño M, Graus F, Dalmau J (2019) Autoimmune seizures and epilepsy. J Clin Invest 129:926–940. https://doi.org/10.1172/JCI125178
Dittrich TD, Baumann SM, Semmlack S, De Marchis GM, Hunziker S, Rüegg S et al (2021) Diagnostic yield of cerebrospinal fluid analysis in status epilepticus: an 8-year cohort study. J Neurol 268(9):3325–3336. https://doi.org/10.1007/s00415-021-10447-3
Vogrig A, Joubert B, Andre-Obadia N, Gigli GL, Rheims S, Honnorat J (2019) Seizure specificities in patients with antibody-mediated autoimmune encephalitis. Epilepsia 60:1508–1525. https://doi.org/10.1111/epi.16282
Ottman R, Lipton RB, Ettinger AB et al (2011) Comorbidities of epilepsy: results from the epilepsy comorbidities and health (EPIC) survey. Epilepsia 52:308–315. https://doi.org/10.1111/j.1528-1167.2010.02927.x
Brooks-Kayal AR, Bath KG, Berg AT et al (2013) Issues related to symptomatic and disease-modifying treatments affecting cognitive and neuropsychiatric comorbidities of epilepsy. Epilepsia 54:44–60. https://doi.org/10.1111/epi.12298
Helmstaedter C, Witt JA (2017) Epilepsy and cognition: a bidirectional relationship? Seizure 49:83–89. https://doi.org/10.1016/j.seizure.2017.02.017
Ettinger A, Reed M, Cramer J (2004) Depression and comorbidity in community-based patients with epilepsy or asthma. Neurology 63:1008–1014. https://doi.org/10.1212/01.wnl.0000138430.11829.61
Baysal-Kirac L, Tuzun E, Altindag E et al (2016) Are there any specific EEG findings in autoimmune epilepsies? Clin EEG Neurosci 47:224–234. https://doi.org/10.1177/1550059415595907
Heine J, Pruss H, Bartsch T, Ploner CJ, Paul F, Finke C (2015) Imaging of autoimmune encephalitis—relevance for clinical practice and hippocampal function. Neuroscience 309:68–83. https://doi.org/10.1016/j.neuroscience.2015.05.037
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by BK (material preparation, data collection), MH (statistical analysis), LC (data collection), NM (data collection), Vincent Navarro (analysis), BH (analysis), and SD (analysis). The first draft of the manuscript was written by SD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, Sophie Dupont states that there is no conflict of interest.
Ethical approval
The study was conducted in accordance with the ethical standards of the AP-HP according to the Declaration of Helsinki and authorized by the CNIL committee (No. 2020051517525).
Consent to participate
Patients provided written informed consent for participation in the study and further publications.
Rights and permissions
About this article
Cite this article
Kambadja, B., Marion, H., Cousyn, L. et al. When should we test patients with epilepsy for autoimmune antibodies? Results from a French retrospective single center study. J Neurol 269, 3109–3118 (2022). https://doi.org/10.1007/s00415-021-10894-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10894-y