Abstract
Background
The lacking awareness of healthcare providers bears the risk of delayed or false diagnoses in rare diseases. No systematic data about misdiagnoses of Moyamoya angiopathy (MMA) are available.
Objective
To evaluate the rate and pattern of missed diagnoses in MMA.
Methods
Retrospective analysis of a consecutive case series from a single German referral center. Rates of missed or delayed diagnoses in Caucasian MMA patients were calculated based on discharge letters from other hospitals and systematic chart review.
Results
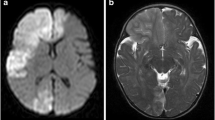
Out of 192 Caucasian patients eventually diagnosed with MMA at our center, an initial misdiagnosis was identified in 119 patients (62%). The time between onset and diagnosis was 1 year in 24 patients, 2 years in 23 patients, 3 years in 10 patients, and > 3 years in 49 patients (mean 5.28, median 3, standard deviation 5.11, and range 4–26 years). The most common misdiagnoses were cerebral vasculitis (31%), etiologically ill-defined stroke diagnoses (30.2%), and MS (3.6%).
Conclusions
This is the first systematic report which shows that patients with MMA are at high risk to be falsely diagnosed and treated. Depiction of typical vascular abnormalities in angiopathy is essential. Normal CSF cell counts, negative oligoclonal bands, and lack of infratentorial lesions as well as gadolinium-positive T1 lesions on MRI may be red flags differentiating this vasculopathy from vasculitis and MS.




Similar content being viewed by others
References
Kleinloog R, Regli L, Rinkel GJ, Klijn CJ (2012) Regional differences in incidence and patient characteristics of moyamoya disease: a systematic review. J Neurol Neurosurg Psychiatry 83(5):531–536. https://doi.org/10.1136/jnnp-2011-301387
Baba T, Houkin K, Kuroda S (2008) Novel epidemiological features of moyamoya disease. J Neurol Neurosurg Psychiatry 79(8):900–904. https://doi.org/10.1136/jnnp.2007.130666
Kraemer M, Heienbrok W, Berlit P (2008) Moyamoya disease in Europeans. Stroke 39(12):3193–3200. https://doi.org/10.1161/STROKEAHA.107.513408
Kim JM, Lee SH, Roh JK (2009) Changing ischaemic lesion patterns in adult moyamoya disease. J Neurol Neurosurg Psychiatry 80(1):36–40. https://doi.org/10.1136/jnnp.2008.145078
Calviere L, Ssi Yan Kai G, Catalaa I, Marlats F, Bonneville F, Larrue V (2012) Executive dysfunction in adults with moyamoya disease is associated with increased diffusion in frontal white matter. J Neurol Neurosurg Psychiatry 83(6):591–593. https://doi.org/10.1136/jnnp-2011-301388
Health Labour Sciences Research Grant for Research on Measures for Infractable D (2012) Treatment of Spontaneous Occlusion of the Circle of W. Guidelines for diagnosis and treatment of moyamoya disease (spontaneous occlusion of the circle of Willis). Neurol Med Chir (Tokyo) 52(5):245–266
Houkin K, Ito M, Sugiyama T, Shichinohe H, Nakayama N, Kazumata K, Kuroda S (2012) Review of past research and current concepts on the etiology of moyamoya disease. Neurol Med Chir (Tokyo) 52(5):267–277
Guey S, Tournier-Lasserve E, Herve D, Kossorotoff M (2015) Moyamoya disease and syndromes: from genetics to clinical management. Appl Clin Genet 8:49–68. https://doi.org/10.2147/TACG.S42772
Preziosa P, Martinelli V, Ferre L, Guaschino C, Simionato F, Moiola L, Comi G, Filippi M (2017) Moyamoya disease mimicking the first attack of multiple sclerosis. J Neurol 264(5):1005–1007. https://doi.org/10.1007/s00415-017-8458-3
Zaheer F, Berger JR (2012) Moyamoya: another multiple sclerosis mimic. Mult Scler Relat Disord 1(2):100–103. https://doi.org/10.1016/j.msard.2011.10.001
Dorfman LJ, Fischbein NJ, Woodard JI, Choudhri O, Bell-Stephens TE, Steinberg GK (2012) Moyamoya disease can masquerade as multiple sclerosis. Neurologist 18(6):398–403. https://doi.org/10.1097/NRL.0b013e31826a99a1
Kraemer M, Berlit P (2010) Primary central nervous system vasculitis and moyamoya disease: similarities and differences. J Neurol 257(5):816–819. https://doi.org/10.1007/s00415-009-5425-7
Heijmen L, van Dijk EJ, Goraj B, van Laarhoven HW (2012) Moyamoya disease misdiagnosed as leptomeningeal metastases. J Clin Oncol 30(36):e382–e385. https://doi.org/10.1200/JCO.2012.43.3227
Gaa J, Weidauer S (2004) Unusual differential diagnosis of leptomeningeal enhancement: moyamoya disease. J Neurol Neurosurg Psychiatry 75(8):1170. https://doi.org/10.1136/jnnp.2003.031393
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12):1226–1237. https://doi.org/10.1056/NEJMra0804622
Kim T, Oh CW, Kwon OK, Hwang G, Kim JE, Kang HS, Cho WS, Bang JS (2016) Stroke prevention by direct revascularization for patients with adult-onset moyamoya disease presenting with ischemia. J Neurosurg 124(6):1788–1793. https://doi.org/10.3171/2015.6.JNS151105
Liu X, Zhang D, Shuo W, Zhao Y, Wang R, Zhao J (2013) Long term outcome after conservative and surgical treatment of haemorrhagic moyamoya disease. J Neurol Neurosurg Psychiatry 84(3):258–265. https://doi.org/10.1136/jnnp-2012-302236
Kraemer M, Karakaya R, Matsushige T, Graf J, Albrecht P, Hartung HP, Berlit P, Laumer R, Diesner F (2018) Efficacy of STA-MCA bypass surgery in moyamoya angiopathy: long-term follow-up of the Caucasian Krupp Hospital cohort with 81 procedures. J Neurol 265(10):2425–2433. https://doi.org/10.1007/s00415-018-9031-4
Kraemer M, Sassen J, Karakaya R, Schwitalla JC, Graf J, Albrecht P, Hartung HP, Diehl RR, Berlit P, Laumer R, Diesner F (2018) Moyamoya angiopathy: early postoperative course within 3 months after STA-MCA-bypass surgery in Europe-a retrospective analysis of 64 procedures. J Neurol 265(10):2370–2378. https://doi.org/10.1007/s00415-018-8997-2
Yamada S, Oki K, Itoh Y, Kuroda S, Houkin K, Tominaga T, Miyamoto S, Hashimoto N, Suzuki N, Research Committee on Spontaneous Occlusion of Circle of W (2016) Effects of surgery and antiplatelet therapy in ten-year follow-up from the registry study of research committee on Moyamoya disease in Japan. J Stroke Cerebrovasc Dis 25(2):340–349. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.10.003
Becker J, Horn PA, Keyvani K, Metz I, Wegner C, Bruck W, Heinemann FM, Schwitalla JC, Berlit P, Kraemer M (2017) Primary central nervous system vasculitis and its mimicking diseases—clinical features, outcome, comorbidities and diagnostic results—a case control study. Clin Neurol Neurosurg 156:48–54. https://doi.org/10.1016/j.clineuro.2017.03.006
Kraemer M, Horn PA, Roder C, Khan N, Diehl RR, Berlit P, Heinemann FM (2012) Analysis of human leucocyte antigen genes in Caucasian patients with idiopathic moyamoya angiopathy. Acta Neurochir (Wien) 154(3):445–454. https://doi.org/10.1007/s00701-011-1261-5
Kraemer M, Lee SI, Ayzenberg I, Schwitalla JC, Diehl RR, Berlit P, Bosche B, Katsarava Z, Obermann M (2016) Headache in Caucasian patients with Moyamoya angiopathy—a systematic cohort study. Cephalalgia. https://doi.org/10.1177/0333102416643516
Kraemer M, Trakolis L, Platzen J, Schwitalla JC, Bersano A, Albrecht P, Schlamann M, Berlit P (2017) Movement symptoms in European Moyamoya angiopathy—first systematic questionnaire study. Clin Neurol Neurosurg 152:52–56. https://doi.org/10.1016/j.clineuro.2016.11.017
Fukui M (1997) Guidelines for the diagnosis and treatment of spontaneous occlusion of the circle of Willis (‘moyamoya’ disease). Research committee on spontaneous occlusion of the Circle of Willis (Moyamoya Disease) of the Ministry of Health and Welfare, Japan. Clin Neurol Neurosurg 99(Suppl 2):S238–S240
Herve D, Kossorotoff M, Bresson D, Blauwblomme T, Carneiro M, Touze E, Proust F, Desguerre I, Alamowitch S, Bleton JP, Borsali A, Brissaud E, Brunelle F, Calviere L, Chevignard M, Geffroy-Greco G, Faesch S, Habert MO, De Larocque H, Meyer P, Reyes S, Thines L, Tournier-Lasserve E, Chabriat H (2018) French clinical practice guidelines for Moyamoya angiopathy. Rev Neurol (Paris) 174(5):292–303. https://doi.org/10.1016/j.neurol.2017.12.002
Garg N, Reddel SW, Miller DH, Chataway J, Riminton DS, Barnett Y, Masters L, Barnett MH, Hardy TA (2015) The corpus callosum in the diagnosis of multiple sclerosis and other CNS demyelinating and inflammatory diseases. J Neurol Neurosurg Psychiatry 86(12):1374–1382. https://doi.org/10.1136/jnnp-2014-309649
Berlit P, Kraemer M (2014) Cerebral vasculitis in adults: what are the steps in order to establish the diagnosis? Red flags and pitfalls. Clin Exp Immunol 175(3):419–424. https://doi.org/10.1111/cei.12221
Haghikia A, Dendrou CA, Schneider R, Gruter T, Postert T, Matzke M, Stephanik H, Fugger L, Gold R (2017) Severe B-cell-mediated CNS disease secondary to alemtuzumab therapy. Lancet Neurol 16(2):104–106. https://doi.org/10.1016/S1474-4422(16)30382-9
Solomon AJ, Corboy JR (2017) The tension between early diagnosis and misdiagnosis of multiple sclerosis. Nat Rev Neurol 13(9):567–572. https://doi.org/10.1038/nrneurol.2017.106
The L (2018) End of the road for daclizumab in multiple sclerosis. Lancet 391(10125):1000. https://doi.org/10.1016/S0140-6736(18)30565-8
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, Fazekas F, Filippi M, Freedman MS, Fujihara K, Galetta SL, Hartung HP, Kappos L, Lublin FD, Marrie RA, Miller AE, Miller DH, Montalban X, Mowry EM, Sorensen PS, Tintore M, Traboulsee AL, Trojano M, Uitdehaag BMJ, Vukusic S, Waubant E, Weinshenker BG, Reingold SC, Cohen JA (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17(2):162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Kelly SB, Chaila E, Kinsella K, Duggan M, Walsh C, Tubridy N, Hutchinson M (2012) Using atypical symptoms and red flags to identify non-demyelinating disease. J Neurol Neurosurg Psychiatry 83(1):44–48. https://doi.org/10.1136/jnnp-2011-300679
Solomon AJ, Bourdette DN, Cross AH, Applebee A, Skidd PM, Howard DB, Spain RI, Cameron MH, Kim E, Mass MK, Yadav V, Whitham RH, Longbrake EE, Naismith RT, Wu GF, Parks BJ, Wingerchuk DM, Rabin BL, Toledano M, Tobin WO, Kantarci OH, Carter JL, Keegan BM, Weinshenker BG (2016) The contemporary spectrum of multiple sclerosis misdiagnosis: a multicenter study. Neurology 87(13):1393–1399. https://doi.org/10.1212/WNL.0000000000003152
Miller DH, Weinshenker BG, Filippi M, Banwell BL, Cohen JA, Freedman MS, Galetta SL, Hutchinson M, Johnson RT, Kappos L, Kira J, Lublin FD, McFarland HF, Montalban X, Panitch H, Richert JR, Reingold SC, Polman CH (2008) Differential diagnosis of suspected multiple sclerosis: a consensus approach. Mult Scler 14(9):1157–1174. https://doi.org/10.1177/1352458508096878
Becker J, Geffken M, Diehl R, Berlit P, Kraemer M (2017) Choosing wisely? Multiple sclerosis and laboratory screening for autoimmune differential diagnoses: do the guideline recommendations of the german society of neurology make sense?. Neurol Int Open. https://doi.org/10.1055/s-0043-115429
Acknowledgements
This work is dedicated to our deceased neuroradiological colleague Dr. Petra Schooß (1969–2016). The authors are thankful for the cooperation with the Department of Radiology and Neuroradiology, Alfried Krupp Hospital, Essen, Germany.
Funding
They did not receive funding for preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Authors report no conflicting interests.
Ethical approval
This study was approved by local ethical committee.
Rights and permissions
About this article
Cite this article
Graf, J., Schwitalla, J.C., Albrecht, P. et al. Misdiagnoses and delay of diagnoses in Moyamoya angiopathy—a large Caucasian case series. J Neurol 266, 1153–1159 (2019). https://doi.org/10.1007/s00415-019-09245-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09245-9