Abstract
Visual pursuit (VP) and visual fixation (VF) have been recognized as the first signs of emerging consciousness and, therefore, are considered indicative of the minimally conscious state (MCS). However, debate exists about their status as they are considered either conscious reactions or reflexes. The aim of this study is to review the evidence of the definition, operationalization, and assessment of VP and VF in unconscious patients. PubMed and EMBASE were searched for relevant papers between May 26, 1994 and October 1, 2016. In addition, an internet search was done to identify other relevant papers, reports and manuals of assessment methods. Papers were included if the definition, operationalization, or assessment method of VP and VF was discussed in patients with disorders of consciousness. We identified 2364 articles, of which 38 were included. No uniform definitions of VP and VF were found. VP and VF were operationalized differently, depending on which scale was used. The Coma Recovery Scale-revised and the Sensory Tool to Assess Responsiveness were the only diagnostic scales found; the other scales were developed to monitor DOC patients. The use of a mirror was the most sensitive method for detecting VP and VF. The literature about the importance VP and VF in relation with consciousness is controversial. This integrative review shows a lack of consensus regarding the definition, operationalization, and assessment of VP and VF. International consensus development about the definition, operationalization, and assessment of VP and VF is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The unresponsive wakefulness syndrome, previously named vegetative state (UWS/VS) [1], and the minimally conscious state (MCS) are one of the worst possible outcomes of acquired brain injury. Patients in UWS/VS show no signs of consciousness [2], whereas MCS patients demonstrate minimal signs of consciousness such as following simple commands, gestural and/or verbal yes/no responses, intelligible verbalization, and purposeful behavior [3]. Complexity of behavior varies between MCS patients; therefore, subcategorization into MCS − (minus) and MCS+ (plus) was proposed. Patients in MCS − only demonstrate non-reflex behavior, whereas MCS+ patients demonstrate command following [4]. Differentiating between UWS/VS and MCS is difficult, as demonstrated by misdiagnosis rates of around 40% [5,6,7,8]. A correct diagnosis of MCS is important for several reasons. First, prognosis is more favorable compared to UWS/VS. A follow-up study showed that improvement beyond a year was absent in UWS/VS patients, whereas 1/3 of MCS patients emerged to consciousness beyond a year [9]. Second, MCS patients might have pain perception capacity, which has consequences for pain management [10]. Third, MCS patients have better outcomes from early intensive neurorehabilitation [11,12,13], recently confirmed in a long-term follow-up study [14]. Fourth, MCS patients may benefit from promising treatment options such as deep brain stimulation [15, 16] and pharmacologic therapies [17,18,19]. Compared to UWS/VS, other ethical dilemmas may arise in MCS patients, e.g., regarding suffering or withdrawing or withholding medical treatment [20].
Currently, an accurate diagnosis of MCS is based on behavioral assessment. Techniques, like neuroimaging, have not been implemented in clinical practice yet. Visual pursuit (VP), which has also been described as visual tracking,Footnote 1 and visual fixation (VF) are considered the first signs of emergence of consciousness [21, 22]. According to the Coma Recovery Scale-Revised (CRS-R), which is the most used assessment scale, VP and VF are clinical signs denoting MCS [23]. According to the CRS-R, VP is present when a moving mirror is followed for 45° without loss of fixation in two of four directions, whereas VF is present when the eyes move from the initial fixation point and re-fixate more than 2 s in two of four trials [24].
Previously, it was demonstrated that failure to detect VP and VF caused misdiagnosis of MCS [7]. This was confirmed in a Dutch prevalence study about UWS/VS [8]: 39% of the reported UWS/VS were misdiagnosed and were at least in MCS. In the 15 MCS patients, VP was seen in 8 of them and VF in one. It remains subject of debate whether or not VP and VF are clearly discernible signs of consciousness. In 1994, the Multi-society Task Force on Persistent Vegetative State (MSTF) reported that VP and VF could be either considered as signs of consciousness or as brief visual orienting reflexes. The MSTF advised to be cautious in diagnosing UWS/VS if VP and/or VF are observed [2]. In 1996, an International Working Party doubted the relation of VP with the conscious state, considering the sole presence of VP not as a reliable sign of consciousness [25, 26]. In 2002, the definition and diagnostic criteria for MCS were published [3]. These criteria were consensus based due to the lack of scientific evidence about diagnosis and prognosis of MCS. VP was incorporated into the criteria as it was considered an example of purposeful behavior based on the following data: VP was associated with late improvement [27], more prevalent in MCS patients [21], and preceded interactive and social behavior later in the recovery course [28]. Regarding the incorporation of VF into the criteria of MCS, no supporting data were reported. Currently, the question whether VP and VF are signs of consciousness still remains debatable. However, in daily practice and in the most recommended assessment scale [23, 24], VP and VF are considered important signs of MCS.
To determine if VP and VF are indicative of consciousness, data about their diagnostic validity are necessary. In 2014, a review about eye movement measurement in the diagnostic assessment in disorders of consciousness (DOC) [29] focused on quantitative techniques to measure eye movements rather than on behavioral assessment. However, this review did not address the question whether VP and/or VF are diagnostic signs of consciousness.
The aim of this study is to review the evidence about definition, operationalization and assessment of VP and VF in relation with the state of consciousness.
Methods
We performed an integrative review, which provides a comprehensive understanding of a particular phenomenon or healthcare problem. This method has the possibility to include a variety of data [30, 31].
Search strategy
The databases of PubMed and EMBASE were searched from May 26, 1994 until October 1, 2016. The publication of the position paper of the Multi-society Task Force on the Persistent Vegetative State was chosen as start date, because they discussed the significance of VP and VF for both UWS/VS and higher levels of consciousness [2]. We searched on the internet for guidelines, reports and for manuals of assessment scales and searched the websites of international taskforces on DOC for relevant papers. The bibliographies of the selected articles were searched for additional relevant papers. Searches were limited to the English, German, French, and Dutch languages.
Two search strategies were used: a broad, general search regarding diagnosis and prognosis in DOC patients and a more specific search related to the use of VP and VF in the diagnosis of DOC.
For the broad general search, we combined patient-related terms like ‘persistent vegetative state’ and ‘minimally conscious state’ with a diagnostic filter and the terms ‘misdiagnosis’, ‘assessment’, and ‘prognosis’. For the specific search, we combined the previously mentioned patient-related terms with terms like ‘visual pursuit’, ‘visual tracking’, ‘visual fixation’, ‘visual perception’, and ‘vision disorders’. Finally, we combined the results of the broad and the specific searches (Supplement 1).
Study selection
Papers were selected if they met one or more of the following inclusion criteria: (1) VP and VF were discussed, either described as DOC in general or described as UWS/VS and/or MCS; (2) the etiology of UWS/VS and MCS was brain injury caused by an acute incident; (3) discussion of the operational definition of VP and/or VF; (4) discussion of different assessment methods; (5) use of an assessment scale testing VP and/or VF; (6) discussion of assessment items of either VP and/or VF; and (7) discussion of influencing factors on visual responses in the assessment of DOC. Papers were excluded if DOC was caused by neurodegenerative diseases and if VP and VF were discussed in patients without DOC.
Data extraction and validation
The first author (BO) reviewed the papers. In case of doubt, a second reviewer (HE) was consulted. After discussion, a decision about inclusion was reached by consensus.
Before reviewing all citations, agreement about the inclusion and exclusion criteria was investigated. Two researchers (BO, HE) independently screened a sample 200 titles and abstracts. After extracting 2 duplicates, 198 papers were checked. Agreement about direct inclusion or papers eligible for further analysis of full text was reached in 168 (85%) of the papers.
Since disagreement existed about a considerable number of papers (n = 30, 15%), we added another search strategy. If based on title and abstract no decision could be made, the full text was electronically screened with the term ‘visual’ to find the terms ‘visual pursuit’, ‘visual fixation’, and ‘visual tracking’. If one of these items was discussed in patients with DOC, the article was eligible for screening of the full text. If not, the paper was excluded. Reanalysis of the 30 papers resulted in disagreement in 2 papers. Thus, adding this method to the search strategy decreased disagreement from 15 to 1%. Disagreement about inclusion was resolved through discussion between both reviewers, which led to consensus.
The selected papers were analyzed by the first author with a data extraction form. This form contained information about: type of article, aim, study subjects, outcome measures, main results, and conclusions.
Results
Included studies
Through the database search, 2351 papers and 13 additional documents were found (Fig. 1). After screening all titles and abstracts, 96 papers and documents were selected for full text analysis. No decision based on title and abstract could be made for 169 papers. Electronic full text screening of these papers yielded 111 eligible for further analysis. In total, full text of 207 papers was analyzed. Eventually, 34 papers could be included. After manual searching the bibliographies of the selected papers, four additional papers were included. The final sample consisted of 38 papers.
Definition
Descriptions of VP and VF were found in six papers; however, no uniform definitions of VP and VF were found. The papers provided eight descriptions of VP and 3 of VF [3, 25, 26, 32,33,34] (Table 1). VP was denoted by the terms eye tracking, tracking eye movements, horizontal and vertical tracking and pursuit eye movements [3, 25, 26, 32, 34]. VP was described as following objects or people [25, 26], as localizing to a visual stimulus [32], as the ability to follow in the horizontal and visual fields [32], and as a reaction to a moving stimulus [3]. VF was denoted by eye contact which was further explained as the patient’s gaze during the majority of the assessment session [32], as sustained fixation in response to a salient stimulus [3], and as active looking at or for objects [33].
Assessment and operationalization of VP and VF
Assessment and operationalization of VP were found in 14 papers in which 9 assessment scales were discussed [23, 24, 28, 32, 34,35,36,37,38,39,40,41,42,43] (Table 2). Another scale, the Sensory Modality Assessment Rehabilitation Technique (SMART) was identified [44], but could not be included, since this scale was not available for evaluation. The assessment scales were developed with different purposes and have different testing procedures and variable operational criteria. Scales with a diagnostic purpose are the CRS-R and the Sensory Tool to Assess Responsiveness (STAR) [23, 24, 43]. In these scales, VP indicates MCS. Scales with purposes of detecting and monitoring signs of consciousness are the Western Neuro Sensory Stimulation Profile (WNSSP) [32], Disorders Of Consciousness Scale (DOCS) [35], Loewenstein Communication Scale (LCS) [36], Comprehensive Assessment Measure for Minimally Responsive Individuals (CAMMRI) [37, 38], Sensory Stimulation Assessment Measure (SSAM) [34], Coma Near Coma Scale (CNC) [39, 40] and the Wessex Head Injury Matrix (WHIM) [28, 41, 42]. VP was tested with different stimuli: objects [28, 32, 34,35,36,37,38, 41, 42], pictures and/or photographs [32, 35, 37, 38], mirror [23, 24, 32, 35, 37, 38, 43], and an individual [28, 32, 34, 36, 39,40,41,42]. In the CRS-R [23, 24], VP was operationalized as following a mirror without loss of fixation in 2/4 trials. In the STAR [43], VP is operationalized slightly different from the CRS-R, the number of trials which is 4 compared to 2 in the CRS-R and the duration of fixation on the mirror is set on 2 s or longer. In the Wessex Head Injury Matrix (WHIM) [28, 41, 42], VP is tested in four reactions, which each have a separate operational definition. A reaction is present if the observed reaction is in accordance with the operational definition of the reaction. The other scales score VP by rating the observed reactions with points [32, 34,35,36,37,38,39,40].
VF was assessed and operationalized in 12 papers, which discussed seven assessment scales [23, 24, 28, 32, 35,36,37,38,39,40,41,42] (Table 3). Testing procedures and operationalization varied between the scales. The only scale with a diagnostic purpose is the CRS-R [23, 24]. In this scale, VF indicates MCS. Scales with purposes of detecting and monitoring signs of consciousness are the WNSSP [32], DOCS [35], LCS [36], CAMMRI [37, 38], CNC [39, 40] and the WHIM [28, 41, 42]. VF was tested with different stimuli: an individual [28, 32, 37, 38, 41, 42], pictures of familiar faces [28, 35, 37, 38, 41, 42], brightly colored or illuminated objects [23, 24, 37, 38], a mirror [37, 38], objects [28, 37, 38, 41, 42] and light flashes [39, 40]. The CRS-R operationalizes VF as re-fixation on an object 2 s or longer and indicates MCS [23, 24]. In the WHIM, 8 reactions test VF, each reaction has its own operational definition and VF is considered present if the operational definition is met [28, 41, 42]. The other scales score VF by rating to different observed reactions with points [32, 35,36,37,38,39,40].
Assessment of visual pursuit
Assessment of VP was discussed in seven papers [45,46,47,48,49,50,51] (Table 4). Results were found about the direction of tracking [45, 47], time of assessment [46], different stimuli [47, 50, 51], quantitative assessment with an eye tracker device [48], and the use of personalized stimuli [49].
Regarding direction of tracking, 48% of 76 head injured adults showed a tracking preference: 28% in the horizontal fields and 20% in the vertical fields [45]. Another study investigated the tracking preference in MCS patients and showed that the MCS- group had a preference of tracking in the horizontal field whereas in MCS + no tracking preference was found [47].
Individual variability of VP within the day was investigated and the highest probabilities for detecting VP were seen at 10.30 AM and at 3.00 PM. The lowest probability for detecting VP was at 2.00 PM, being a post-prandial time point [46].
The use of a mirror was the stimulus with the highest scores in DOC patients. In 1995, it was demonstrated that patients following a mirror had significantly higher mean scores on the visual tracking scale of the WNSSP compared to patients following an individual, picture, or object [45]. These results were confirmed by recent studies. VP was investigated in 51 MCS patients. Thirty-eight (75%) of them showed VP, and 11 (29%) only showed VP when a mirror was used [51]. Another study with 88 MCS patients investigated VP with different objects. VP was detected in 61/88 (69%) of patients, and in 16 (26%) of them VP was exclusively detected by a mirror [47].
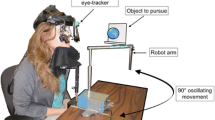
VP was also studied in DOC patients quantitatively with an infrared eye tracker [48, 49]. Patients looked to either a moving red circle or a moving parrot, which were presented on a screen. VP was measured by electronically calculating the percentage of fixations on the target. MCS patients followed the target more frequent (32.9%) compared to UWS/VS patients (4.9%). In a second study from the same authors, a moving photo of a relative was added as an extra stimulus [49]. In MCS patients, a significant higher frequency of following the moving photo of a close relative was found (37.3%) compared to the images of the parrot (29.9%) and the circle (30.6%). In UWS/VS and healthy control subjects, no significant differences were seen between the applied stimuli [49].
Assessment of visual fixation
Assessment of VF was discussed in five papers [50, 52,53,54,55] (Table 5). Different stimuli were discussed: objects like a mirror, a ball, a light [52], familiar photographs and a card [53,54,55]. In the WHIM, VF is mainly tested by looking at a person. In one reaction tested by the WHIM an object was used, but was not further specified. Two studies tested VF in combination with the techniques Brain Computer Interface (BCI) and functional Magnetic Resonance Imaging (fMRI), respectively [53, 55].
Investigation of VF in MCS patients with different stimuli showed that VF was significantly more seen on the mirror (48%) compared to the ball (28%) and a light (25%) [52]. In an analysis of different items of the WHIM, maintaining gaze or gaze shifting reactions were more prevalent in MCS compared to UWS/VS patients [50].
Three studies discussed the use of visual stimuli with images of familiar persons. First, visual attention to a personal stimulus was compared to a neutral stimulus and patients oriented more frequent to the familiar image than to the neutral stimulus [54]. Second, in a BCI study, VF was investigated in patients with UWS/VS, MCS, locked-in syndrome and healthy controls. It was demonstrated that accuracies of attending to one’s own photo were higher than to unfamiliar photos. However, no differences between UWS/VS and MCS were found [53]. Third, an fMRI study investigated visual perception of different pictures in nine MCS patients and ten healthy controls [55]. In 6/9 MCS patients and all healthy controls looking at family pictures had higher activation in the visual networks compared to looking at other pictures.
Influencing factors
Five influencing factors on visual responses were discussed in eight studies: within-day variability [56], inter-rater reliability (IRR) differences due to profession and/or experience [57, 58], presence of an informal caregiver [59], duration of assessment [60], and influences of visual/oculomotor impairments [6, 61, 62] (Table 6). Most of the results of these studies presented CRS-R visual subscale scores, which were not subdivided in VP and/or VF. First, visual subscale scores on the CRS-R were higher in the morning than in the afternoon, which could be explained by individual changes in visual functioning or by the presence of fragmentary cyclic processes [56]. Second, in two studies, IRR was investigated between different professionals and/or different levels of experience [57, 58]. The IRR on the visual subscale of the CRS-R was good (k = 0.73). The IRR of physicians was slightly higher (k = 0.81) compared to psychologists (k = 0.68) and a group of physiotherapists, speech therapists, and nurses (k = 0.73). Assessors who had > 24 months experience in assessing DOC patients showed a higher IRR (k = 0.81) than assessors with less experience (k = 0.62 for experience < 24 months and k = 0.68 for experience < 12 months) [57]. Another study showed a lower IRR for the visual subscale score of the CRS-R in experienced (k = 0.48) as well as in the less experienced assessors (k = 0.47) [58]. Third, the involvement of an informal caregiver in the assessment resulted in higher visual subscale scores on the CRS-R compared to assessment of a clinician alone [59]. Fourth, the duration of the assessment was investigated in 10 DOC patients. When two repeated assessment with the CRS-R (50–60 min) and 10 SMART assessment (600 min) were compared, this led to differences in the level of consciousness in 4/10 patients. In 2/4 patients, these differences were caused by detecting sustained VF with the SMART and not with the CRS-R [60]. Fifth, influences of visual impairments and/or oculomotor defects on assessment of the level of consciousness were found in 3 studies [6, 61, 62]. In misdiagnosed UWS/VS patients, 65% had visual impairments [6], and in MCS patients, 9/52 (17%) scored no visual responses on the CRS-R [62] and analysis of CRS-R subscale scores showed that visual problems such as optical nerve damage, ptosis, ocular apraxia and visual agnosia could cause improbable CRS-R scores [61].
Discussion
To our knowledge, this is the first review that addresses the question whether or not VP and VF are related to consciousness. We found that literature about the importance of these responses in relation with consciousness still is controversial. No agreed-upon definition of VP and VF was found and the assessment methods vary widely regarding procedures and operational criteria. However, the studies generally agreed that the use of a mirror is the most sensitive method to detect VP and VF.
The lack of an agreed-upon definition has led to international differences in interpretations. In the United States, VP and VF are considered signs of MCS, whereas in the United Kingdom (UK) these signs are atypical but viewed as signs of UWS/VS [63,64,65]. In addition, not operationally defined terms like ‘brief’ and ‘sustained’ VP and/or VF, can cause differences in interpretation with a risk of diagnostic inaccuracy. Furthermore, a recent expert opinion stated that there is no rationale why a brief visual response does not require consciousness and a sustained response does [66]. To conclude, evidence for the use of ‘brief’ and ‘sustained’ VP and VF for distinguishing UWS/VS from MCS is lacking.
A wide variety of assessment methods with variable operational criteria of VP and VF were found. Only the CRS-R and the STAR were developed with a diagnostic purpose. The other scales were mainly developed to monitor neurobehavioral functions. Judging the validity of the different scales is difficult because a golden standard is lacking for diagnosis of the level of consciousness. In 2010, 13 DOC assessment scales were reviewed. The CRS-R is the only scale recommended with ‘minor reservations’ because it has acceptable administration and scoring guidelines and good content validity. Despite the recommendations for clinical use, the authors of this review stated that evaluation of diagnostic validity remains problematic. Diagnostic validity was unproven for all assessment scales and interpretation is difficult because of the lack of a standard criterion measure for the assessment of the level of consciousness [67].
The use of a mirror appeared to be the most sensitive method to detect VP and VF [47, 51, 52]. It has been suggested that the use of patient’s own face can be useful to detect residual self-awareness [68] and that personally relevant stimuli increase the probability of detecting a conscious response in DOC patients [69]. However, recent studies published after our search period indicate that the sensitivity of the mirror cannot be explained by a lower cognitive demand [70], neither the self-referential aspect of the mirror is viewed as a complete explanation [71]. Therefore, the rationale for the sensitivity of the mirror has not been clarified yet.
The absence of visual responses in a considerable part of the DOC patients calls for a nuance to the view that VP and VF are important signs for detecting consciousness. Although it was demonstrated that visual responses were the signs most frequently detected in MCS patients, the absence in about 20% of the MCS population cannot be ignored [62]. Examination of the integrity of the visual tract with techniques like visual evoked potentials and imaging is advisable in patients with DOC who do not show visual responses. A closer look into the neurobiology of VP and VF shows that VP is considered to be under volitional control [72]. For VF, however, it remains questionable if this sign is a conscious response because saccadic eye movements are necessary to shift gaze from one position to another. Saccades can be either voluntary or reflexive [73, 74]. The existence of accurate localization in the visual field without consciously processing visual stimuli, which can be present in patients with blindsight and visual form agnosia, further complicates the understanding of the association of VP and VF with consciousness. Since the association of VP and VF with consciousness remains questionable, further research is needed. Longitudinal studies which follow VP and VF during the recovery phase may give insight into the question if and/or how VP and VF are associated with consciousness.
There are some limitations regarding the literature search and the interpretation. First, the methodological quality of the included papers was not systematically assessed. Because we included theoretical, empirical and expert-opinion papers, a uniform quality assessment was not possible. Second, different descriptions that existed for VF such as ‘focusing on the examiner’ and ‘active looking for objects’, might have led to possible misinterpretation of these reactions as VF. Third, the SMART might be a proper scale for assessment; however, we could not evaluate the properties of this scale, since it requires formal training and it must be purchased. Previously, it has also been reported that the SMART may not be accessible for users outside the UK [67].
In conclusion, the question whether or not VP and VF are signs of MCS cannot be answered uniformly yet. This review demonstrates a lack of consensus regarding definition, operationalization and assessment methods. Although VP and VF are widely recognized as signs of emerging consciousness, the supporting evidence is scarce. Moreover, since VP and VF are included into the diagnostic criteria of MCS, it is not surprising that these signs are more prevalent in MCS patients than in UWS/VS patients. One can speak of a circular argument if based on such a prevalence difference, authors conclude that VP and VF are indicative of consciousness. More research is needed to investigate the validity of these signs to measure the level of consciousness before adopting them as important diagnostic signs of MCS. Therefore, we recommend international consensus development about definitions, operational criteria and assessment procedures of VP and VF. Reaching consensus about these first signs of consciousness is highly important for a proper diagnosis and consequently increases the chance for providing rehabilitation to this population. As recently stated by Fins [75], misdiagnosis of MCS patients as UWS/VS, can deny them access to rehabilitation and thereby marginalizes these patients. Proper identification of MCS can pave the way for rehabilitation and thereby breaching the marginalization of these vulnerable patients.
Notes
We will use the term visual pursuit. When we refer to a specific paper, we will use the terminology mentioned in that paper.
References
Laureys S, Celesia GG, Cohadon F, Lavrijsen J, Leon-Carrion J, Sannita WG, Sazbon L, Schmutzhard E, von Wild KR, Zeman A, Dolce G (2010) Unresponsive wakefulness syndrome: a new name for the vegetative state or apallic syndrome. BMC Med 8:68
Multi-Society Task Force on PVS (1994) Medical aspects of the persistent vegetative state (1). N Engl J Med 330:1499–1508
Giacino JT, Ashwal S, Childs N, Cranford R, Jennett B, Katz DI, Kelly JP, Rosenberg JH, Whyte J, Zafonte RD, Zasler ND (2002) The minimally conscious state: definition and diagnostic criteria. Neurology 58:349–353
Bruno MA, Vanhaudenhuyse A, Thibaut A, Moonen G, Laureys S (2011) From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndromes: recent advances in our understanding of disorders of consciousness. J Neurol 258:1373–1384
Childs NL, Mercer WN, Childs HW (1993) Accuracy of diagnosis of persistent vegetative state. Neurology 43:1465–1467
Andrews K, Murphy L, Munday R, Littlewood C (1996) Misdiagnosis of the vegetative state: retrospective study in a rehabilitation unit. BMJ 313(7048):13–16
Schnakers C, Vanhaudenhuyse A, Giacino J, Ventura M, Boly M, Majerus S, Moonen G, Laureys S (2009) Diagnostic accuracy of the vegetative and minimally conscious state: clinical consensus versus standardized neurobehavioral assessment. BMC Neurol 9:35
van Erp WS, Lavrijsen JC, Vos PE, Bor H, Laureys S, Koopmans RT (2015) The vegetative state: prevalence, misdiagnosis, and treatment limitations. J Am Med Dir Assoc 16(85):89–95
Luaute J, Maucort-Boulch D, Tell L, Quelard F, Sarraf T, Iwaz J, Boisson D, Fischer C (2010) Long-term outcomes of chronic minimally conscious and vegetative states. Neurology 75:246–252
Boly M, Faymonville ME, Schnakers C, Peigneux P, Lambermont B, Phillips C, Lancellotti P, Luxen A, Lamy M, Moonen G, Maquet P, Laureys S (2008) Perception of pain in the minimally conscious state with PET activation: an observational study. Lancet Neurol 7:1013–1020
Eilander HJ, van Heugten CM, Wijnen VJ, Croon MA, de Kort PL, Bosch DA, Prevo AJ (2013) Course of recovery and prediction of outcome in young patients in a prolonged vegetative or minimally conscious state after severe brain injury: an exploratory study. J Pediatr Rehabil Med 6:73–83
Dolce G, Lucca LF, Quintieri M, Leto E, Rogano S, Riganello F, Pignolo L (2012) Neurorehabilitation for severe disorder of consciousness: the S. Anna—RAN operational model. J Rehabil Med 44:512–516
Seel RT, Douglas J, Dennison AC, Heaner S, Farris K, Rogers C (2013) Specialized early treatment for persons with disorders of consciousness: program components and outcomes. Arch Phys Med Rehabil 94:1908–1923
Eilander HJ, Wijnen VJ, Schouten EJ, Lavrijsen JC (2016) Ten-to-twelve years after specialized neurorehabilitation of young patients with severe disorders of consciousness: a follow-up study. Brain Inj 30:1302–1310
Schiff ND, Fins JJ (2007) Deep brain stimulation and cognition: moving from animal to patient. Curr Opin Neurol 20:638–642
Giacino J, Fins JJ, Machado A, Schiff ND (2012) Central thalamic deep brain stimulation to promote recovery from chronic posttraumatic minimally conscious state: challenges and opportunities. Neuromodulation 15:339–349
Singh R, McDonald C, Dawson K, Lewis S, Pringle AM, Smith S, Pentland B (2008) Zolpidem in a minimally conscious state. Brain Inj 22:103–106
Whyte J, Rajan R, Rosenbaum A, Katz D, Kalmar K, Seel R, Greenwald B, Zafonte R, Demarest D, Brunner R, Kaelin D (2014) Zolpidem and restoration of consciousness. Am J Phys Med Rehabil 93:101–113
Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, Eifert B, Long D, Katz DI, Cho S, Yablon SA, Luther M, Hammond FM, Nordenbo A, Novak P, Mercer W, Maurer-Karattup P, Sherer M (2012) Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med 366:819–826
Fins JJ, Schiff ND (2017) Differences that make a difference in disorders of consciousness. AJOB Neurosci 8:131–134
Giacino JT, Kalmar K (1997) The vegetative state and minimally conscious states: a comparison of clinical features and functional outcome. J Head Trauma Rehabil 12:36–51
Monti MM, Laureys S, Owen AM (2010) The vegetative state. BMJ 341:3765
Giacino JT, Kalmar K, Whyte J (2004) The JFK coma recovery scale-revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil 85:2020–2029
Giacino JT, Kalmar K (2004) Coma recovery scale-revised. Administration and Scoring Guidelines, Edison
Andrews K (1996) International working party on the management of the vegetative state: summary report. Brain Inj 10:797–806
Andrews K (1996) International working party. Report on the vegetative state. Royal Hospital for Neuro-disability, West Hill
Ansell BJ, Keenan JE (1989) The western neuro sensory stimulation profile: a tool for assessing slow-to-recover head-injured patients. Arch Phys Med Rehabil 70:104–108
Shiel A, Horn SA, Wilson BA, Watson MJ, Campbell MJ, McLellan DL (2000) The Wessex Head Injury Matrix (WHIM) main scale: a preliminary report on a scale to assess and monitor patient recovery after severe head injury. Clin Rehabil 14:408–416
Ting WK, Perez Velazquez JL, Cusimano MD (2014) Eye movement measurement in diagnostic assessment of disorders of consciousness. Front Neurol 5:137
Whittemore R, Knafl K (2005) The integrative review: updated methodology. J Adv Nurs 52:546–553
Broome M (1993) Integrative literature reviews for the development of concepts. WB Saunders Co., Philadelphia
Ansell BJ, Keenan JE, De la Rocha O (1989) Western Neuro Stimulation Profile. Western Neuro Care Center, Tustin, California
Wade DT, Johnston C (1999) The permanent vegetative state: practical guidance on diagnosis and management. BMJ 319:841–844
Rader MA, Ellis DW (1994) The sensory stimulation assessment measure (SSAM): a tool for early evaluation of severely brain-injured patients. Brain Inj 8:309–321
Bender Pape T (2011) Administration manual disorders of consciousness scale. Hines, Illinois
Borer-Alafi N, Gil M, Sazbon L, Korn C (2002) Loewenstein communication scale for the minimally responsive patient. Brain Inj 16:593–609
Gollega A, Ostapovitch MM, Lazoruk AC, Renton S, Haynes E, Lawson D, Lee-Kemp B, Martin S, Jachak A (2014) CAMMRI Comprehensive Assessment Measure for Minimally Responsive Individuals. Associaltion for the Rehabilitation of the Brain Injured, Calgary
Gollega A, Meghji C, Renton S, Lazoruk A, Haynes E, Lawson D, Ostapovitch M (2015) Multidisciplinary assessment measure for individuals with disorders of consciousness. Brain Inj 29:1460–1466
Rappaport M (1990) Rappaport Coma/Near Coma Scale. San José, California
Rappaport M, Dougherty AM, Kelting DL (1992) Evaluation of coma and vegetative states. Arch Phys Med Rehabil 73:628–634
Shiel A, Wilson BA, McLellan L, Watson M, Horn S (2000) The Wessex Head Injury Matrix. Revised Scoring sheet, Pearson Assessment, London
Shiel A, Wilson BA, McLellan L, Horn S, Watson M (2000) The Wessex Head Injury Matrix. Pearson Assessment, London
Stokes V, Gunn S, Schouwenaars K, Badwan D (2016) Neurobehavioural assessment and diagnosis in disorders of consciousness: a preliminary study of the Sensory Tool to Assess Responsiveness (STAR). Neuropsychological Rehabilitation pp 1-18. https://doi.org/10.1080/09602011.2016
Gill-Thwaites H (1997) The Sensory Modality Assessment Rehabilitation Technique–a tool for assessment and treatment of patients with severe brain injury in a vegetative state. Brain Inj 11:723–734
Ansell BJ (1995) Visual tracking behavior in low functioning head-injured adults. Arch Phys Med Rehabil 76:726–731
Candelieri A, Cortese MD, Dolce G, Riganello F, Sannita WG (2011) Visual pursuit: within-day variability in the severe disorder of consciousness. J Neurotrauma 28:2013–2017
Thonnard M, Wannez S, Keen S, Bredart S, Bruno MA, Gosseries O, Demertzi A, Thibaut A, Chatelle C, Charland-Verville V, Heine L, Habbal D, Laureys S, Vanhaudenhuyse A (2014) Detection of visual pursuit in patients in minimally conscious state: a matter of stimuli and visual plane? Brain Inj 28:1164–1170
Trojano L, Moretta P, Loreto V, Cozzolino A, Santoro L, Estraneo A (2012) Quantitative assessment of visual behavior in disorders of consciousness. J Neurol 259:1888–1895
Trojano L, Moretta P, Loreto V, Santoro L, Estraneo A (2013) Affective saliency modifies visual tracking behavior in disorders of consciousness: a quantitative analysis. J Neurol 260:306–308
Turner-Stokes L, Bassett P, Rose H, Ashford S, Thu A (2015) Serial measurement of Wessex Head Injury Matrix in the diagnosis of patients in vegetative and minimally conscious states: a cohort analysis. BMJ Open 5:e006051
Vanhaudenhuyse A, Schnakers C, Bredart S, Laureys S (2008) Assessment of visual pursuit in post-comatose states: use a mirror. J Neurol Neurosurg Psychiatr 79:223
Di H, Nie Y, Hu X, Tong Y, Heine L, Wannez S, Huang W, Yu D, He M, Thibaut A, Schnakers C, Laureys S (2014) Assessment of visual fixation in vegetative and minimally conscious states. BMC Neurol 14:147
Pan J, Xie Q, He Y, Wang F, Di H, Laureys S, Yu R, Li Y (2014) Detecting awareness in patients with disorders of consciousness using a hybrid brain-computer interface. J Neural Eng 11:056007
Whyte J, DiPasquale MC (1995) Assessment of vision and visual attention in minimally responsive brain injured patients. Arch Phys Med Rehabil 76:804–810
Zhu J, Wu X, Gao L, Mao Y, Zhong P, Tang W, Zhou L (2009) Cortical activity after emotional visual stimulation in minimally conscious state patients. J Neurotrauma 26:677–688
Cortese MD, Riganello F, Arcuri F, Pugliese ME, Lucca LF, Dolce G, Sannita WG (2015) Coma recovery scale-r: variability in the disorder of consciousness. BMC Neurol 15:186. https://doi.org/10.1186/s12883-015-0455-5
Estraneo A, Moretta P, De Tanti A, Gatta G, Giacino JT, Trojano L (2015) An Italian multicentre validation study of the coma recovery scale-revised. Eur J Phys Rehabil Med 51(5):627–634
Lovstad M, Froslie KF, Giacino JT, Skandsen T, Anke A, Schanke AK (2010) Reliability and diagnostic characteristics of the JFK coma recovery scale-revised: exploring the influence of rater’s level of experience. J Head Trauma Rehabil 25(5):349–356. https://doi.org/10.1097/HTR.0b013e3181cec841
Sattin D, Giovannetti AM, Ciaraffa F, Covelli V, Bersano A, Nigri A, Ferraro S, Minati L, Rossi D, Duran D, Parati E, Leonardi M (2014) Assessment of patients with disorder of consciousness: do different coma recovery scale scoring correlate with different settings? J Neurol 261(12):2378–2386. https://doi.org/10.1007/s00415-014-7478-5
Godbolt AK, Stenson S, Winberg M, Tengvar C (2012) Disorders of consciousness: preliminary data supports added value of extended behavioural assessment. Brain Inj 26(2):188–193. https://doi.org/10.3109/02699052.2011.648708
Chatelle C, Bodien YG, Carlowicz C, Wannez S, Charland-Verville V, Gosseries O, Laureys S, Seel RT, Giacino JT (2016) Detection and interpretation of impossible and improbable coma recovery scale-revised scores. Arch Phys Med Rehabil 97(8):1295–1300.e1294. https://doi.org/10.1016/j.apmr.2016.02.009
Estraneo A, Moretta P, Cardinale V, De Tanti A, Gatta G, Giacino JT, Trojano L (2015) A multicentre study of intentional behavioural responses measured using the coma recovery scale-revised in patients with minimally conscious state. Clin Rehabil 29(8):803–808. https://doi.org/10.1177/0269215514556002
Giacino JT, Smart CM (2007) Recent advances in behavioral assessment of individuals with disorders of consciousness. Curr Opin Neurol 20:614–619
Laureys S, Boly M (2007) What is it like to be vegetative or minimally conscious? Curr Opin Neurol 20:609–613
Schnakers C, Perrin F, Schabus M, Majerus S, Ledoux D, Damas P, Boly M, Vanhaudenhuyse A, Bruno MA, Moonen G, Laureys S (2008) Voluntary brain processing in disorders of consciousness. Neurology 71:1614–1620
Wade D (2017) Back to the bedside? Making clinical decisions in patients with prolonged unconsciousness. J Med Ethics 43:457–458
Seel RT, Sherer M, Whyte J, Katz DI, Giacino JT, Rosenbaum AM, Hammond FM, Kalmar K, Pape TL, Zafonte R, Biester RC, Kaelin D, Kean J, Zasler N (2010) Assessment scales for disorders of consciousness: evidence-based recommendations for clinical practice and research. Arch Phys Med Rehabil 91:1795–1813
Laureys S, Perrin F, Bredart S (2007) Self-consciousness in non-communicative patients. Conscious Cogn 16:722–741 (discussion 742-725)
Perrin F, Castro M, Tillmann B, Luaute J (2015) Promoting the use of personally relevant stimuli for investigating patients with disorders of consciousness. Front Psychol 6:1102
Cruse D, Fattizzo M, Owen AM, Fernandez-Espejo D (2017) Why use a mirror to assess visual pursuit in prolonged disorders of consciousness? Evidence from healthy control participants. BMC Neurol 17:14
Wannez S, Vanhaudenhuyse A, Laureys S, Bredart S (2017) Mirror efficiency in the assessment of visual pursuit in patients in minimally conscious state. Brain Inj 31:1–7
Lisberger SG (2015) Visual Guidance of smooth pursuit eye movements. Annu Rev Vis Sci 1:447–468
Pierrot-Deseilligny C, Milea D, Muri RM (2004) Eye movement control by the cerebral cortex. Curr Opin Neurol 17:17–25
Leigh RJA, Zee DSA (2015) The neurology of eye movements. Oxford University Press, New York
Fins JJ (2017) Brain injury and the civil right we don’t think about. The New York Times. https://www.nytimes.com/2017/08/24/opinion/minimally-conscious-brain-civil-rights.html. Accessed 21 Dec 2017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Overbeek, B.U.H., Eilander, H.J., Lavrijsen, J.C.M. et al. Are visual functions diagnostic signs of the minimally conscious state? an integrative review. J Neurol 265, 1957–1975 (2018). https://doi.org/10.1007/s00415-018-8788-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8788-9