Abstract
Background
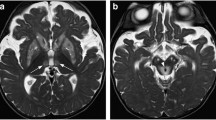
Leukoencephalopathies with prominent involvement of cerebellum and brainstem, henceforward called prominent infratentorial leukoencephalopathies (PILs), encompass a variety of inherited and acquired white matter diseases. Erdheim–Chester disease (ECD) is a rare non-Langerhans cell histiocytosis likely under-diagnosed as cause of adult PIL.
Methods
We reviewed the clinical and laboratory information of ten consecutive sporadic adult patients with PIL of unknown origin, who were investigated for ECD.
Results
There were seven males and three females; mean age at clinical onset was 49.6 years (range 38–59); cerebellar ataxia with or without other neurological symptoms was the only or the main clinical manifestation; diabetes insipidus was present in three individuals. Eight patients had white matter focal supratentorial abnormalities, in addition to the infratentorial white matter changes. Six out of eight patients had spinal cord lesions. Thoraco-abdominal CT showed periaortic sheathing in two patients, whole-body FDG-PET revealed increased glucose uptake in the long bones of the legs in five patients, brain FDG-PET showed overt infratentorial hypermetabolism in one patient. In eight patients, ECD was confirmed by bone scintigraphy, pathological data, or both. Two ECD patients treated with vemurafenib showed a marked improvement of neurological symptoms and brain MRI abnormalities at 1 year follow-up.
Conclusions
Symptoms of PIL can be the only clinical manifestation of ECD. Adult patients with PIL of unknown origin should undergo investigations aimed at unveiling ECD, including bone scintigraphy and whole-body FDG-PET. The early diagnosis allows starting disease-modifying therapies of an otherwise life-threatening disease.



Similar content being viewed by others
References
Schiffmann R, van der Knaap MS (2009) Invited article: an MRI-based approach to the diagnosis of white matter disorders. Neurology 72:750–759
Gass A, Filippi M, Grossman RI (2000) The contribution of MRI in the differential diagnosis of posterior fossa damage. J NeurolSci 172(Suppl 1):S43–S49
Rovira À, Sastre-Garriga J, Auger C et al (2013) Idiopathic inflammatory demyelinating diseases of the brainstem. Semin Ultrasound CT MR 34:123–130
Akman-Demir G, Bahar S, Coban O et al (2003) Cranial MRI in Behçet’s disease: 134 examinations of 98 patients. Neuroradiology 45:851–859
Pittock SJ, Debruyne J, Krecke KN et al (2010) Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS). Brain 133:2626–2634
Tateishi U, Terae S, Ogata A et al (2001) MR imaging of the brain in lymphomatoidgranulomatosis. AJNR Am J Neuroradiol 22:1283–1290
Landolfi JC, Thaler HT, DeAngelis LM (1998) Adult brainstem gliomas. Neurology 51:1136–1139
Grimm SA, Chamberlain MC (2013) Brainstem glioma: a review. Curr Neurol Neurosci Rep 13:346
Singh TD, Fugate JE, Rabinstein AA (2014) Central pontine and extrapontine myelinolysis: a systematic review. Eur J Neurol 21:1443–1450
van der Knaap MS, Arts WF, Garbern JY et al (2008) Cerebellar leukoencephalopathy: most likely histiocytosis-related. Neurology 71:1361–1367
Diamond EL, Dagna L, Hyman DM et al (2014) Consensus guidelines for the diagnosis and clinical management of Erdheim–Chester disease. Blood 124:483–492
Cavalli G, Guglielmi B, Berti A et al (2013) The multifaceted clinical presentations and manifestations of Erdheim–Chester disease: comprehensive review of the literature and of 10 new cases. Ann Rheum Dis 72:1691–1695
Salsano E, Savoiardo M, Nappini S et al (2008) Late-onset sporadic ataxia, pontine lesion, and retroperitoneal fibrosis: a case of Erdheim–Chester disease. Neurol Sci 29:263–267
Cangi MG, Biavasco R, Cavalli G et al (2015) BRAFV600E-mutation is invariably present and associated to oncogene-induced senescence in Erdheim–Chester disease. Ann Rheum Dis 74:1596–1602
Cavalli G, Biavasco R, Borgiani B et al (2014) Oncogene-induced senescence as a new mechanism of disease: the paradigm of Erdheim–Chester disease. Front Immunol 5:281
Arnaud L, Hervier B, Néel A et al (2011) CNS involvement and treatment with interferon-α are independent prognostic factors in Erdheim–Chester disease: a multicenter survival analysis of 53 patients. Blood 117:2778–2782
Euskirchen P, Haroche J, Emile JF et al (2015) Complete remission of critical neurohistiocytosis by vemurafenib. Neurol Neuroimmunol Neuroinflamm 2:e78. https://doi.org/10.1212/NXI.0000000000000078
Haroche J, Cohen-Aubart F, Emile JF et al (2015) Reproducible and sustained efficacy of targeted therapy with vemurafenib in patients with BRAF(V600E)-mutated Erdheim–Chester disease. J Clin Oncol 33:411–418
López RF, Báñez IA, Robles MB et al (2017) 18F-FDG PET/CT in Erdheim–Chester disease. Eur J Nucl Med Mol Imaging 44:1247–1248
Ayrignac X, Boutiere C, Carra-Dalliere C et al (2016) Posterior fossa involvement in the diagnosis of adult-onset inherited leukoencephalopathies. J Neurol 263:2361–2368
Campochiaro C, Tomelleri A, Cavalli G et al (2015) Erdheim–Chester disease. Eur J Intern Med 26:223–229
Lachenal F, Cotton F, Desmurs-Clavel H et al (2006) Neurological manifestations and neuroradiological presentation of Erdheim–Chester disease: report of 6 cases and systematic review of the literature. J Neurol 253:1267–1277
Bianco F, Iacovelli E, Tinelli E et al (2009) Characteristic brain MRI appearance of Erdheim–Chester disease. Neurology 73:2120–2122
Adle-Biassette H, Chetritt J, Bergemer-Fouquet AM et al (1997) Pathology of the central nervous system in Chester-Erdheim disease: report of three cases. J Neuropathol Exp Neurol 56:1207–1216
Diamond EL, Hatzoglou V, Patel S et al (2016) Diffuse reduction of cerebral grey matter volumes in Erdheim–Chester disease. Orphanet J Rare Dis 11:109
Tien R, Kucharczyk J, Kucharczyk W (1991) MR imaging of the brain in patients with diabetes insipidus. AJNR Am J Neuroradiol 12:533–542
Prosch H, Grois N, Bökkerink J et al (2006) Central diabetes insipidus: is it Langerhans cell histiocytosis of the pituitary stalk? A diagnostic pitfall. Pediatr Blood Cancer 46:363–366
Drier A, Haroche J, Savatovsky J et al (2010) Cerebral, facial, and orbital involvement in Erdheim–Chester disease: CT and MR imaging findings. Radiology 255:586–594
Grois N, Prayer D, Prosch H et al (2005) Neuropathology of CNS disease in Langerhans cell histiocytosis. Brain 128:829–838
Ferrero E, Corti A, Haroche J et al (2016) Plasma Chromogranin A as a marker of cardiovascular involvement in Erdheim–Chester disease. Oncoimmunology 5:e1181244
Bargagli E, Maggiorelli C, Rottoli P (2008) Human chitotriosidase: a potential new marker of sarcoidosis severity. Respiration 76:234–238
Mossetti G, Rendina D, Numis FG et al (2003) Biochemical markers of bone turnover, serum levels of interleukin-6/interleukin-6 soluble receptor and bisphosphonate treatment in Erdheim–Chester disease. Clin Exp Rheumatol 21:232–236
Tiacci E, Trifonov V, Schiavoni G et al (2011) BRAF mutations in hairy-cell leukemia. N Engl J Med 364:2305–2315
Sedrak P, Ketonen L, Hou P et al (2011) Erdheim–Chester disease of the central nervous system: new manifestations of a rare disease. AJNR Am J Neuroradiol 32:2126–2131
Shamburek RD, Brewer HB Jr, Gochuico BR (2001) Erdheim–Chester disease: a rare multisystem histiocytic disorder associated with interstitial lung disease. Am J Med Sci 321:66–75
Birnbaum DC, Shields D, Lippe B et al (1989) Idiopathic central diabetes insipidus followed by progressive spastic cerebral ataxia. Report of four cases. Arch Neurol 46:1001–1003
Acknowledgements
We wish to dedicate this manuscript to Dr. Mario Savoiardo, passed away on January 2014. His love for life taught us not to observe things superficially, but to investigate in depth all clinical and instrumental data of the patients, because even a small detail can be decisive for their care.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Source of financial support
None.
Conflicts of interest
All authors declare that they have no conflict of interest.
Ethical standards
This study was performed as per local ethics committee-approved guidelines in accordance with the Declaration of Helsinki principles, and all the involved patients gave their written informed consent.
Rights and permissions
About this article
Cite this article
Chiapparini, L., Cavalli, G., Langella, T. et al. Adult leukoencephalopathies with prominent infratentorial involvement can be caused by Erdheim–Chester disease. J Neurol 265, 273–284 (2018). https://doi.org/10.1007/s00415-017-8692-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8692-8