Abstract
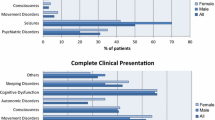
Anti-N-Methyl-d-Aspartate receptor (NMDAR) encephalitis is an acute neurological disorder affecting children and adults. We aimed to compare the clinical characteristics, treatments, and outcomes between children and adults with anti-NMDAR encephalitis and to assess the probable risk factors. In this observational study, patients who tested positive for anti-NMDAR antibody in the cerebrospinal fluid were enrolled. The patients were divided into children and adults group on the basis of age (whether <16 or not). Clinical outcomes were assessed at onset, 1, 3, 6, 9, and 12 months after the patients received treatment and were scored based on whether they required hospitalization and intensive care. A total of 15 children and 14 adults were examined. The adults more likely manifested status epilepticus, central hypoventilation, and pneumonia but less likely exhibited movement disorder than the children did. All of the patients were subjected to corticosteroid treatment, 11 children and 9 adults were treated with intravenous immunoglobulin, and only the adults received plasma exchange or cyclophosphamide. The children recovered faster than the adults, especially in the first 6 months. Risk factors included age, status epilepticus, changes in consciousness, central hypoventilation, and pneumonia. Adults exhibit worse outcomes than children mostly because of status epilepticus.




Similar content being viewed by others
References
Graus F, Titulaer MJ, Balu R et al (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Zekeridou A, Karantoni E, Viaccoz A et al (2015) Treatment and outcome of children and adolescents with N-methyl-d-aspartate receptor encephalitis. J Neurol 262:1859–1866
Dalmau J, Tuzun E, Wu HY et al (2007) Paraneoplastic anti-N-methyl-d-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:25–36
Gable MS, Sheriff H, Dalmau J et al (2012) The frequency of autoimmune N-methyl-d-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis 54:899–904
Titulaer MJ, McCracken L, Gabilondo I et al (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165
Irani SR, Bera K, Waters P et al (2010) N-methyl-d-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133:1655–1667
Brzek A, Nowak Z, Plewa M (2002) Modified programme of in-patient (phase I) cardiac rehabilitation after acute myocardial infarction. Int J Rehabil Res 25:225–229
Johnston SC, Siedenberg R, Min JK et al (1997) Central apnea and acute cardiac ischemia in a sheep model of epileptic sudden death. Ann Neurol 42:588–594
Claassen J, Riviello JJ Jr, Silbergleit R (2015) Emergency neurological life support: status epilepticus. Neurocrit Care 23(Suppl 2):S136–S142
Veciana M, Becerra JL, Fossas P et al (2015) EEG extreme delta brush: an ictal pattern in patients with anti-NMDA receptor encephalitis. Epilepsy Behav 49:280–285
Kim H, Ryu H, Kang JK (2015) Anti-NMDA receptor antibody encephalitis presenting with unilateral non-convulsive status epilepticus in a male patient. J Epilepsy Res 5:17–19
Foff EP, Taplinger D, Suski J et al (2016) EEG Findings May Serve as a Potential Biomarker for Anti-NMDA Receptor Encephalitis. Clin EEG Neurosci. doi:10.1177/1550059416642660
Tobin WO, Strand EA, Clark HM et al (2014) NMDA receptor encephalitis causing reversible caudate changes on MRI and PET imaging. Neurol Clin Pract 4:470–473
Ellis ME, Diehl LF, Granger E et al (1989) Trephine needle bone marrow biopsy in the initial staging of Hodgkin disease: sensitivity and specificity of the Ann Arbor staging procedure criteria. Am J Hematol 30:115–120
Wright S, Hacohen Y, Jacobson L et al (2015) N-methyl-d-aspartate receptor antibody-mediated neurological disease: results of a UK-based surveillance study in children. Arch Dis Child 100:521–526
Locasciulli A, Bacigalupo A, Van Lint MT et al (1990) Hepatitis B virus (HBV) infection and liver disease after allogeneic bone marrow transplantation: a report of 30 cases. Bone Marrow Transpl 6:25–29
Kuroda Y (2016) Neurocritical care update. J Intensive Care 4:36
Leitinger M, Kalss G, Rohracher A et al (2015) Predicting outcome of status epilepticus. Epilepsy Behav 49:126–130
Chanson E, Bicilli E, Lauxerois M et al (2016) Anti-NMDA-R encephalitis: should we consider extreme delta brush as electrical status epilepticus? Neurophysiol Clin 46:17–25
Matoq AA, Rappoport AS, Yang Y et al (2015) Anti-NMDA-receptor antibody encephalitis in infants. Epilepsy Behav Case Rep 4:99–101
Alsaadi T, Shakra M, Turkawi L et al (2015) VNS terminating refractory nonconvulsive SE secondary to anti-NMDA encephalitis: a case report. Epilepsy Behav Case Rep 3:39–42
Kadoya M, Onoue H, Kadoya A et al (2015) Refractory status epilepticus caused by anti-NMDA receptor encephalitis that markedly improved following combination therapy with rituximab and cyclophosphamide. Intern Med 54:209–213
Barros P, Brito H, Ferreira PC et al (2014) Resective surgery in the treatment of super-refractory partial status epilepticus secondary to NMDAR antibody encephalitis. Eur J Paediatr Neurol 18:449–452
Marques IB, Teotonio R, Cunha C et al (2014) Anti-NMDA receptor encephalitis presenting with total insomnia–a case report. J Neurol Sci 336:276–280
Finne Lenoir X, Sindic C, van Pesch V et al (2013) Anti-N-methyl-d-aspartate receptor encephalitis with favorable outcome despite prolonged status epilepticus. Neurocrit Care 18:89–92
Pinho J, Rocha J, Rodrigues M et al (2012) Diversity in anti-N-methyl-d-aspartate receptor encephalitis: case-based evidence. Psychiatry Clin Neurosci 66:153–156
Goldberg EM, Taub KS, Kessler SK et al (2011) Anti-NMDA receptor encephalitis presenting with focal non-convulsive status epilepticus in a child. Neuropediatrics 42:188–190
Kirkpatrick MP, Clarke CD, Sonmezturk HH et al (2011) Rhythmic delta activity represents a form of nonconvulsive status epilepticus in anti-NMDA receptor antibody encephalitis. Epilepsy Behav 20:392–394
Adamec C (1966) The use of Spearman’s correlation order coefficient in validation. Cesk Zdrav 14:100–102
Acknowledgments
This work was supported by grants from National Natural Science Foundation, China (81360201).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical standards
This study was conducted in compliance with the ethical standards.
Informed consent
Written consents were obtained from the patients.
Rights and permissions
About this article
Cite this article
Huang, Q., Wu, Y., Qin, R. et al. Clinical characteristics and outcomes between children and adults with anti-N-Methyl-d-Aspartate receptor encephalitis. J Neurol 263, 2446–2455 (2016). https://doi.org/10.1007/s00415-016-8282-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8282-1