Abstract
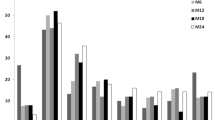
Rituximab (RTX) efficacy in NMO is suggested by several case series. No consensus exists on optimal dosing strategies. At present the treatment schedules more frequently used are 375 mg/m2/week iv for 4 weeks (RTX-A) and 1000 mg iv twice, 2 weeks apart (RTX-B). Aim of this study is to confirm RTX efficacy and safety in the treatment of NMO and to evaluate whether a most favourable dosage regimen exists. Data on RTX-treated NMO patients were collected from 13 Italian Hospitals. 73 patients (64 F), were enlisted. RTX-A was administered in 42/73 patients, RTX-B in 31/73. Median follow-up was 27 months (range 7–106). Mean relapse rate in the previous year before RTX start was 2.2 ± 1.3 for RTX-A and 2.3 ± 1.2 for RTX-B. ARR in the first year of treatment was 0.8 ± 0.9 for RTX-A and 0.2 ± 0.4 for RTX-B, in the second year of treatment was 0.9 ± 1.5 for RTX-A and 0.4 ± 0.8 for RTX-B patients (p = 0.001 for the first year, ns (0.09) for the second year). RTX-B was more effective in delaying the occurrence of a relapse (HR 2.2 (95 % IC 1.08–4.53) p = 0.02). Adverse events were described in 19/73 patients (mainly urinary tract and respiratory infections, and infusion reactions). Two deaths were reported in severely disabled patients. Though with the limitations of an observational study, our data support RTX efficacy in NMO and suggest that high dose pulses might be more effective than a more fractioned dose.



Similar content being viewed by others
References
Wingerchuk DM, Banwell B, Bennett JL et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Wingerchuk DM, Weinshenker BG (2014) Neuromyelitis optica (Devic’s syndrome). Handb Clin Neurol 122:581–599
Sellnera J, Boggild M, Clanet M et al (2010) EFNS guidelines on diagnosis and management of neuromyelitis optica. Eur J Neurol 17:1019–1032
Kimbrough DJ, Fujihara K, Jacob A et al (2012) Treatment of neuromyelitis optica: review and recommendations. Mult Scler Relat Disord 1:180–187
Pescovitz MD (2006) Rituximab, an anti-cd20 monoclonal antibody: history and mechanism of action. Am J Transplant 5:859–866
Weiner GJ (2010) Rituximab: mechanism of action. Semin Haematol 47:115–123
Lucchinetti CF, Guo Y, Popescu BF, Fujihara K, Itoyama Y, Misu T (2014) The pathology of an autoimmune astrocytopathy: lessons learned from neuromyelitis optica. Brain Pathol 24:83–97
Cree BA, Lamb S, Morgan K, Chen A, Waubant E, Genain C (2005) An open label study of the effects of rituximab in neuromyelitis optica. Neurology 64:1270–1272
Capobianco M, Malucchi S, di Sapio A et al (2007) Variable responses to rituximab treatment in neuromyelitis optica (Devic’s disease). Neurol Sci 28:209–211
Jacob A, Weinshenker BG, Violich I et al (2008) Treatment of neuromyelitis optica with rituximab: retrospective analysis of 25 patients. Arch Neurol 65:1443–1448
Bedi GS, Brown AD, Delgado SR, Usmani N, Lam BL, Sheremata WA (2011) Impact of rituximab on relapse rate and disability in neuromyelitis optica. Mult Scler 17:1225–1230
Bomprezzi R, Postevka E, Campagnolo D, Vollmer TL (2011) A review of cases of neuromyelitis optica. Neurologist 17:98–104
Pellkofer HL, Krumbholz M, Berthele A et al (2011) Long-term follow-up of patients with neuromyelitis optica after repeated therapy with rituximab. Neurology 76:1310–1315
Greenberg BM, Graves D, Remington G et al (2012) Rituximab dosing and monitoring strategies in neuromyelitis optica: creating strategies for therapeutic success. Mult Scler 18:1022–1026
Lindsey JW, Meulmester KM, Brod SA, Nelson F, Wolinsky JS (2012) Variable results after rituximab in neuromyelitis optica. J Neurol Sci 317:103–105
Ip VH, Lau AY, Au LW et al (2013) Rituximab reduces attacks in Chinese patients with neuromyelitis optica spectrum disorders. J Neurol Sci 324:38–39
Kim SH, Huh SY, Lee SJ, Joung A, Kim HJ (2013) A 5-year follow-up of rituximab treatment in patients with Neuromyelitis Optica spectrum disorder. JAMA Neurol 70:1110–1117
Yang CS, Yang L, Li T et al (2013) Responsiveness to reduced dosage of rituximab in Chinese patients with neuromyelitis optica. Neurology 81:710–713
Mealy MA, Wingerchuk DM, Palace J, Greenberg BM, Levy M (2014) Comparison of relapse and treatment failure rates among patients with neuromyelitis optica: multicenter study of treatment efficacy. JAMA Neurol 71:324–330
Torres J, Pruitt A, Balcer L, Galetta S, Markowitz C, Dahodwala N (2015) Analysis of the treatment of neuromyelitis optica. J Neurol Sci 351:31–35
Radaelli M, Moiola L, Sangalli F et al. (2016) Neuromyelitis optica spectrum disorders: long-term safety and efficacy of rituximab in caucasian patients. Mult Scler 22(4):511–519. doi:10.1177/1352458515594042
Collongues N, Brassat D, Maillart E, et al. (2015) Efficacy of rituximab in refractory neuromyelitis optica. Mult Scler 22(7):955–959. doi: 10.1177/1352458515602337
Zèphir H, Bernard-Valnet R, Lebrun C et al (2015) Rituximab as first-line therapy in Neuromyelitis optica: efficiency and tolerability. J Neurol 262:2329–2335
Kim SH, Jeong IH, Hyun JW et al. (2015) Treatment outcomes with rituximab in 100 patients with neuromyelitis optica: influence of FCGR3A polymorphisms on the therapeutic response to rituximab. JAMA Neurol 72(9):989–995. doi:10.1001/jamaneurol.2015.1276
Hauser SL, Waubant E, Arnold DL et al (2015) B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med 358:676–688
Del Poeta G, Del Principe MI, Buccisano F et al (2008) Consolidation and maintenance immunotherapy with rituximab improve clinical outcome in patients with B-cell chronic lymphocytic leukemia. Cancer 112:119–128
Miravalle AA, Kinkel R, Langer-Gould A et al. (2009) B Cell depletion and safety of low dose Rituximab in patients with Relapsing Remitting Multiple Sclerosis. Presented at the LXI AAN congress; Seattle, WA
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an Expanded Disability Status Scale (EDSS). Neurology 33:1444–1452
Wingerchuck DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG (2006) Revised diagnostic criteria for neuromyelitis optica. Neurology 66:1485–1489
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Kitley J, Elsone L, George J et al (2013) Methotrexate is an alternative to azathioprine in neuromyelitis optica spectrum disorders with aquaporin-4 antibodies. JNNP 84:918–921
Ramanathan RS, Malhotra K, Scott T (2014) Treatment of neuromyelitis optica/neuromyelitis optica spectrum disorders with methotrexate. BMC Neurol 14:51
Provan D, Butler T, Evangelista ML et al (2007) Activity and safety profile of low-dose rituximab for the treatment of autoimmune cytopenias in adults. Haematologica 92:1695–1698
Blum S, Gillis D, Brown H et al (2010) Use and monitoring of low dose rituximab in myasthenia gravis. J Neurol Neurosurg Psychiatry 82:659–663
Chay J, Donovan P, Cummins L, Kubler P, Pillans P (2013) Experience with low-dose rituximab in off-label indications at two tertiary hospitals. Intern Med J 43:871–882
Bredemeier M, de Oliveira FK, Rocha CM (2014) Low- versus high-dose rituximab for rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res 66:228–235
Bredemeier M, Campos GG, de Oliveira FK (2015) Updated systematic review and meta-analysis of randomized controlled trials comparing low- versus high-dose rituximab for rheumatoid arthritis. Clin Rheumatol 34:1801–1805
Van Vollenhoven RF, Emery P, Bingham CO 3rd et al (2013) Long-term safety of rituximab in rheumatoid arthritis: 9.5-year follow-up of the global clinical trial programme with a focus on adverse events of interest in RA patients. Ann Rheum Dis 72:1496–1502
Lan L, Han F, Chen JH (2012) Efficacy and safety of rituximab therapy for systemic lupus erythematosus: a systematic review and meta-analysis. J Zhejiang Univ Sci B 13:731–744
Molloy ES, Calabrese LH (2012) Progressive multifocal leukoencephalopathy associated with immunosuppressive therapy in rheumatic diseases: evolving role of biologic therapies. Arthritis Rheum 64:3043–3051
Etemadifar M, Nasr Z, Khalili B, Taherioun M, Vosoughi R (2015) Epidemiology of neuromyelitis optica in the world: a systematic review and meta-analysis. Mult Scler Int 2015:174720. doi:10.1155/2015/174720
Wingerchuk DM, Hogancamp WF, O’Brien PC, Weinshenker BG (1999) The clinical course of neuromyelitis optica (Devic’s syndrome). Neurology 53:1107–1114
Weinshenker BG, Barron G, Behne JM et al (2015) Challenges and opportunities in designing clinical trials for neuromyelitis optica. Neurology 84:1805–1815
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Annovazzi received honoraria for advisory and speaking activities by Biogen, Merck Serono, Novartis, Sanofi Genzyme and TEVA. Dr. Capobianco speaking honoraria from Biogen, Almirall and Sanofi Genzyme; advisory board honoraria from Biogen and web paper production fees from Serono Foundation. Dr. Moiola received honoraria for speaking from Sanofi Aventis, Merck Serono and Biogen Idec. Prof. Patti received honoraria for advisory and speaking activities by Almirall, Bayer, Biogen, Merck Serono, Novartis Sanofi Genzyme and TEVA; He also received travel grants for congress participation by the same companies. He received unrestricted grants by the University of Catania, MIUR and FISM. Dr. Frau serves on scientific advisory boards for Biogen, received honoraria for speaking from Merck Serono and Teva, received research grant from Merck Serono. Prof. Uccelli received consultancy fees and support for travel expenses and participation to Congresses from Sanofi-Avemtis, Biogen, Merck-Serono, Novartis, and Roche. Prof. Centonze is an Advisory Board member of Almirall, Bayer Schering, Biogen, Genzyme, GW Pharmaceuticals, Merck-Serono, Novartis, Teva and received honoraria for speaking or consultation fees from Almirall, Bayer Schering, Biogen Idec, Genzyme, GW Pharmaceuticals, Merck Serono, Novartis, Sanofi-Aventis, Teva. He is also an external expert consultant of the European Medicine Agency (EMA), and the principal investigator in clinical trials for Bayer Schering, Biogen Idec, Merck Serono, Mitsubishi, Novartis, Roche, Sanofi-aventis, Teva. His preclinical and clinical research was supported by grants from Bayer, Biogen, Merck Serono, Novartis e Teva. Dr. Perini received honoraria from Biogen, Serono, Novartis, Teva, Genzyme for lectures or advisory boards. Dr. Tortorella received honoraria for speaking from Biogen, Sanofi-Aventis, Serono and Bayer Schering, Teva, Genzyme and Novartis. Dr. Prosperini received honoraria for advisory and speaking activities by Biogen, Teva, Novartis, Sanofi Genzyme and research grant from FISM. Prof Lus received speaking honoraria and/or consultant fees from Biogen, Merck-Serono, Bayer, Novartis, Genzyme and Almirall. Dr. Fuiani received honoraria for speaking and advisory boards from Biogen and Sanofi-Aventis. Dr. Falcini reports no competing interests. Dr. Martinelli received honoraria for speaking and/or for consultancy and support for travel expenses and participation to Congresses from Bayer, Biogen-Idec, Merck-Serono, Novartis, Genzyme and Teva Pharma. Prof Comi serves on scientific advisory boards for Bayer Schering Pharma, Merck Serono, Teva, Sanofi Aventis, Novartis and Biogen-Idec; has received speaker honoraria from Teva, Sanofi Aventis, Serono Sumposia International Foundation, Biogen-Idec, Merck Serono, Novartis, Bayer Schering and Sanofi Aventis. Dr. Ghezzi serves on scientific advisory boards or as a consultant for Merck Serono, Novartis, Genzyme, Biogen Idec, Teva; received honoraria for speaking form Merck Serono, Serono Symposia International Foundation, Biogen Idec, Allmirall, Genzyme, Teva, and Novartis.
Ethical standard
The study was approved by the Ethical Committee of the coordinating centre in Gallarate Hospital (VA), Italy. The study was conducted complying with Helsinki Declaration.
Rights and permissions
About this article
Cite this article
Annovazzi, P., Capobianco, M., Moiola, L. et al. Rituximab in the treatment of Neuromyelitis optica: a multicentre Italian observational study. J Neurol 263, 1727–1735 (2016). https://doi.org/10.1007/s00415-016-8188-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8188-y