Abstract
Cardiac arrhythmia is currently considered to be the direct cause of death in a majority of sudden unexplained death (SUD) cases, yet the genetic predisposition and corresponding endophenotypes contributing to SUD remain incompletely understood. In this study, we aimed to investigate the involvement of Coenzyme Q (CoQ) deficiency in SUD. First, we re-analyzed the exome sequencing data of 45 SUD and 151 sudden infant death syndrome (SIDS) cases from our previous studies, focusing on previously overlooked genetic variants in 44 human CoQ deficiency-related genes. A considerable proportion of the SUD (38%) and SIDS (37%) cases were found to harbor rare variants with likely functional effects. Subsequent burden testing, including all rare exonic and untranslated region variants identified in our case cohorts, further confirmed the existence of significant genetic burden. Based on the genetic findings, the influence of CoQ deficiency on electrophysiological and morphological properties was further examined in a mouse model. A significantly prolonged PR interval and an increased occurrence of atrioventricular block were observed in the 4-nitrobenzoate induced CoQ deficiency mouse group, suggesting that CoQ deficiency may predispose individuals to sudden death through an increased risk of cardiac arrhythmia. Overall, our findings suggest that CoQ deficiency-related genes should also be considered in the molecular autopsy of SUD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The etiology of unexpected sudden death is diverse and highly correlated with age of onset [1]. Coronary artery disease is thought to be the major cause of unexpected sudden death in older people [2]. However, in younger populations, it often strikes apparently healthy children and young adults without prior clinical symptoms or diagnosed diseases [3, 4]. In up to one third of these deceased, no clear cause of death can be established, even after a comprehensive medico-legal investigation, including pathological/toxicological assessment and forensic investigation of the circumstances of death [5, 6]. In such cases, the deaths could be termed as sudden infant death syndrome (SIDS) in an individual younger than one year of age [7], sudden unexplained death (SUD) in an individual older than 1 year of age, or sudden arrhythmic death syndrome (SADS) for cases with a negative pathological and toxicological assessment [8].
Understanding the exact causes of SUD will not only improve the accuracy of pathological diagnosis, but also provide important information about the genetic background of rare cardiovascular diseases. Although the pathophysiological mechanisms of SUD remain incompletely understood, an increasing number of studies have shown that cardiac arrhythmia could be the direct cause of death in the majority of SUD cases. Genetic testing and functional assays have identified numerous pathogenic single nucleotide variants (SNVs) or structural variations (SVs) located in genes associated with primary arrhythmia syndromes [9]. However, there is still a large proportion of SUD cases that remain unexplained even after post-mortem molecular autopsy [10, 11]. It is therefore very likely that the genetic predisposition and corresponding endophenotypes contributing to SUD are more diverse than expected.
Coenzyme Q (CoQ) is a lipophilic molecule synthesized in the mitochondria. It consists of a quinone group and of a polyisoprenoid tail of variable length in different species: yeast has six units (CoQ6), mice nine (CoQ9) and humans ten (CoQ10) [12]. A central role of CoQ is to act as an electron transporter in mitochondrial respiratory chain (MRC) function [13]. CoQ deficiency is a rare mitochondrial disorder associated with heterogeneous phenotypes and a characteristic decrease in CoQ10 levels in human tissues and plasma [14]. In general, CoQ deficiency due to variants in genes encoding proteins of the CoQ biosynthesis pathway or its regulation is defined as primary CoQ deficiency. When CoQ deficiency is caused by other metabolic disorders or genetic defects unrelated to the CoQ biosynthesis pathway, it is referred to as secondary CoQ deficiency [15]. Both primary and secondary CoQ deficiencies can lead to varying degrees of clinical manifestations, with single or multiple organ systems involved.
Sufficient CoQ is essential for normal heart function, as cardiac contraction and activation of ATP-regulated membrane channels depend on energy supply from MRC function. Previous studies have shown that circulating CoQ levels are significantly lower in patients with dilated cardiomyopathy compared to healthy controls [16]. However, it remains unclear whether CoQ deficiency contributes to arrhythmic death. When investigating the genetic predisposition to SUD, previous studies have mainly focused on known susceptibility genes for ion channelopathies, inherited cardiomyopathy or epilepsy, while the involvement of deleterious variants in CoQ deficiency-related genes has always been overlooked [17,18,19]. To comprehensively evaluate the role of CoQ deficiency in SUD, we re-analyzed the available exome sequencing data of our SUD and SIDS cohorts [20, 21], focusing on the CoQ deficiency-related genes that have not been investigated before. In addition, the correlation observed at the genetic level was examined in a mouse model through electrophysiological and morphological experiments, to test whether CoQ deficiency could predispose to SUD.
Materials and methods
Exome sequencing data re-analysis
Initially, 45 SUD cases and 155 SIDS cases from our previous studies were re-evaluated for the purpose of this research. The inclusion criteria, autopsy findings and sequencing procedures have been described previously [20, 21]. The SUD cohort consisted of 45 cases with a mean age (± SD) of 30.2 (± 14.5) years (range: 1–63 years of age) and a mean body mass index (± SD) of 24.9 (± 4.9) (range: 13.7–35.5). 34 (76%) of the deceased were male and the majority were of European origin (89%). As the exome sequencing data of 4 SIDS cases were not available for re-analysis, the SIDS dataset consisted of 151 exomes. The deceased SIDS infants had a mean age (± SD) of 17.6 (± 10.7) weeks (range: 0.6–48.1 weeks), 91 (60%) were boys and all of them were of European origin.
Genetic investigation was confined to a target gene panel consisting of 44 known human CoQ deficiency-related genes (Geneset B) [22]. An overview of the genes and their constraint metrics [23] are shown in Supplementary Table S1. Most of the CoQ deficiency-related genes have not been previously analyzed in the SUD study (Geneset A: consisted of 244 genes [20]) and the SIDS study (Geneset C: consisted of 192 genes [21]), with the exception of 7 genes (ACADVL, BRAF, ETFB, ETFDH, FXN, MT-TL1, and PDSS2) that have been reported to participate in cardiovascular/metabolic diseases. Variant filtering was performed according to the following rules: (1) functional impact-based filtering retaining only exonic variants that are non-synonymous, frameshift, and nonsense, as well as splice-site and untranslated region (UTR) variants; (2) allele frequency-based filtering retaining only variants with a minor allele frequency (MAF) < 0.1% in all populations according to the Genome Aggregation Database (gnomAD) [24]. Subsequently, an automated pathogenicity assessment and variant classification were performed according to the ACMG/AMP guidelines using Varsome v.10.1 [25, 26].
Gene-based burden testing
To further compare the aggregate burden of rare variants in the 44 CoQ deficiency-related genes between our case cohorts and the general population, without considering their predicted functional effects, a burden test including all rare exonic and UTR variants identified in the previous step was performed using the software package TRAPD and 60,706 Exome Aggregation Consortium (ExAC) data sets from gnomAD [27]. Compared to the commonly used single-variant-based tests [28], a gene-based burden test, which assesses the cumulative effect of multiple variants influencing the phenotype in the same direction, could improve the power to detect statistical signals between case and control subjects. Based on the number of case and control subjects carrying and not carrying a qualifying variant in each gene, P values were calculated using the two-sided Fisher’s exact test. For the dominant model, the number of cases carrying at least one qualifying variant in each gene was tabulated. For the recessive model, the case cohort counts were generated by tabulating the number of cases carrying two or more qualifying variants in each gene. P values < 0.05 were considered significant for both models. For a better illustration, quantile-quantile plots of the initial burden test results were generated.
CoQ deficiency mouse model
The CoQ deficiency mouse model was induced using 4-nitrobenzoate (4-NB) [29]. Briefly, 3-week-old C57Bl/6 mice (9 males and 9 females for each group) were treated with 0.05 M 4-NB solution by oral administration for 6 weeks. Soluble 4-NB was prepared by adding 8.36 mg/ml 4-nitrobenzoic acid (Merck KGaA, Darmstadt, Germany) and 4.21 mg/ml sodium bicarbonate (Merck KGaA, Darmstadt, Germany) to the sterile drinking water. Since sodium bicarbonate, which serves to increase the solubility, could be an additional confounding factor, a sex-matched control group A (Ctrl-A) treated with 0.05 M sodium bicarbonate solution was used. In addition, a blank control group B (Ctrl-B) was recruited without any treatment.
Electrophysiological and morphological measurements
Mice were anaesthetized with 1–3% isoflurane in oxygen and kept warm with a heating pad. Surgical steel needle electrodes were then placed under the skin of each limb and the electrocardiogram (ECG) was recorded in lead I and lead II configuration. Baseline ECGs were recorded for approximately 10 min until a stable baseline and heart rate (HR) were achieved. Transthoracic Doppler echocardiograms were measured using the Vinno 6 platform (VINNO Technology, Suzhou, China). M-mode cine loops were acquired in 2-dimensional parasternal short-axis view at the papillary muscle level to measure interventricular septal end-diastole and end-systole (IVSd and IVSs), left ventricular internal diameter end diastole and end systole (LVIDd and LVIDs), left ventricular posterior wall end-diastole and end-systole (LVPWd and LVPWs), left ventricular end-diastolic and end-systolic volume (LVEDV and LVESV), ejection fraction (EF) and fractional shortening (FS) at the time of echocardiography. All measurements were performed in triplicate. Mice were sacrificed and autopsied immediately after the experiments for body and heart weight measurements.
CoQ extraction and quantification
Weighed heart tissue samples were homogenized after mixing with 500 µL methyl tert-butyl ether (MTBE), 100 µL methanol, and 250 µL water. After centrifugation at 12,000 rpm for 15 min, a 300 µL aliquot of the MTBE layer was transferred to a new tube and dried under a gentle nitrogen flow. The residue was reconstituted with 300 µL of 50% acetonitrile/2-propanol and centrifuged at 12,000 rpm for 15 min. A 10 µL aliquot of each sample was then mixed with 290 µL of 50% acetonitrile/2-propanol containing CoQ10-d6 internal standard (Cayman Chemical, Michigan, USA) and transferred to an autosampler vial for UHPLC-MRM-MS analysis. A series of calibration standard solutions were prepared by stepwise dilution of the CoQ9 standard stock solution (Merck KGaA, Darmstadt, Germany) to generate a calibration curve, and the least squares method was used for regression fitting. An Agilent 1290 Infinity II series UHPLC System and an Agilent 6460 triple quadrupole mass spectrometer were applied for UHPLC separation and assay development.
Statistical analysis
Statistical analysis was performed with GraphPad Prism software v 8.3.0 (La Giolla, CA, USA). Continuous variables, such as PR interval, were presented as mean ± standard error. Differences between groups were compared using the one-way ANOVA test for normally distributed continuous variables with homogeneous variance, otherwise the Kruskal-Wallis test was used. All statistical tests were two-sided and a P value < 0.05 was considered statistically significant.
Results
Variants with likely functional effects in CoQ deficiency-related genes
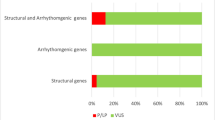
A total of 3 rare pathogenic or likely pathogenic (P/LP) variants were found in 3 different SUD cases (7%). Two of these variants were identified in the exonic region of CFTR and one in the exonic region of PAH. In addition, 16 variants of uncertain significance (VUS) in 12 genes were identified in 14 (31%) SUD cases. Among these VUS, 10 were located in the exonic region and 6 in the UTR. In total, 17 (38%) SUD cases were identified as harboring rare variants with likely functional effects (Supplementary Table S2). A total of 7 and 12 rare variants with likely functional effects were found to affect primary CoQ deficiency-related genes and secondary CoQ deficiency-related genes, respectively. Among the affected genes, HTT has the highest prevalence of variants in the SUD cohort (Fig. 1A). In terms of clinical evidence, 12 (63%) of the variants were not evaluated before, since an interpretation for these variants in the ClinVar database was not available. Additional demographic characteristics of the above mentioned 17 SUD cases can be found in Supplementary Table S3.
Rare variants with likely functional effects in the case cohorts. Genes marked with an asterisk indicate primary CoQ deficiency-related genes. (A) 19 rare P/LP variants or VUS distributed in 12 known human CoQ deficiency-related genes were identified in 17 out of the 45 SUD cases (38%). (B) 76 rare P/LP variants or VUS distributed among 28 known human CoQ deficiency-related genes were identified in 56 out of the 151 SIDS cases (37%). (C) P/LP variants in genes associated with cardiovascular/metabolic diseases were previously identified in 10 SUD cases and 31 SIDS cases, respectively. Among the 3 SUD cases and 16 SIDS cases harboring at least one of the P/LP variants in Geneset B (44 human CoQ deficiency-related genes), P/LP variants in Geneset A (244 genes analyzed in the SUD study) and Geneset C (192 genes analyzed in the SIDS study) were also identified in 1 SUD case and 4 SIDS cases, respectively. (D) Among the P/LP variants or VUS identified, 6 variants occurred in two or more cases (highlighted in bold). These included 2 LP variants (rs140455771 and rs143456784) and 4 VUS (rs1800120, rs754558646, rs779780620, and rs897162037). The 4 VUS were also found to coexist with several other P/LP variants (highlighted in red) or VUS in genes associated with cardiovascular/metabolic diseases or CoQ deficiency
In the SIDS cohort, 18 rare P/LP variants were identified in 8 genes (ACADVL, CFTR, COQ8A, DHCR7, ETFDH, NPC1, PAH, and TBC1D24) in 16 cases (11%), while another 58 rare VUS were identified in 26 genes in 46 (30%) cases. Taken together, a total of 56 (37%) SIDS cases were found to harbor rare variants with likely functional effects. Of the total 76 rare variants with likely functional effects, 40 were located in the exonic region and 36 in the UTR (Supplementary Table S4). As a secondary CoQ deficiency-related gene, CFTR has the highest prevalence of variants in the SIDS cohort (Fig. 1B). In terms of clinical evidence, 40 (53%) of the variants were novel and thus not evaluated in the ClinVar database before.
Within the 3 SUD cases and the 16 SIDS cases harboring at least one of the P/LP variants in the 44 CoQ deficiency-related genes, we had previously identified several P/LP variants in cardiovascular/metabolic disease-associated genes. Since 37 out of the 44 CoQ deficiency-related genes (Geneset B) were not included in either Geneset A or Geneset C, carriers with shared variants from different genesets were further investigated. As shown in Fig. 1C, one of the SUD cases (SUDS112) was found to harbor P/LP variants in the two Genesets A and B. Specifically, one LP variant was detected in Geneset B (CFTR) and 3 P/LP variants in Geneset A (ANK2, CALR3, and MLYCD) (Supplementary Table S5). In addition, 4 SIDS cases (SIDS045, SIDS091, SIDS100, and SIDS156) were found to harbor P/LP variants in the two Genesets B and C (Fig. 1C), with a total of 7 P/LP variants in Geneset B (ACADVL, ANO10, CFTR, DHCR7, and TBC1D24) and a total of 5 P/LP variants in Geneset C (ACADVL, CASQ2, SCN1B, SCN10A, and SYNE1) (Supplementary Table S5).
Among the P/LP variants or VUS identified in our SUD and SIDS cohorts, 6 variants appeared in two or more cases (Fig. 1D and Supplementary Table S6). One of the LP variants, CFTR: rs140455771, was the only variant identified in SIDS030 and SIDS072 after a thorough review of genes associated with cardiovascular/metabolic diseases and CoQ deficiency, suggesting that this variant might be a finding that deserves further functional investigation. Similarly, another LP variant, CFTR: rs143456784, was the only positive finding in SIDS164 and SIDS230. In addition, the 4 VUS identified in this study (CFTR: rs1800120, TBC1D24: rs754558646, HTT: rs779780620, and FDX2: rs897162037) were found to coexist with several other P/LP variants or VUS in genes associated with cardiovascular/metabolic diseases or CoQ deficiency. Thus, it was not possible to associate the phenotypic information of these cases with specific variants due to their complex genetic background.
Burden testing of rare exonic and UTR variants
A gene-based burden test between the SUD cases and 60,706 controls from the gnomAD datasets revealed a significant genetic burden in 17 out of the 18 genes containing at least one rare exonic/UTR variant under the dominant model, indicating a strong association of these genes with SUD in a dominant state. Besides, HTT also reached strong association signals under the recessive model, suggesting that variants in this gene might be pathogenic even in a recessive state (Fig. 2A and Supplementary Table S7). For SIDS cases, a significant genetic burden was observed in 34 out of the 36 genes containing at least one rare exonic/UTR variant under the dominant model. Among these, 3 genes (ANO10, MVK, and NPC1) also reached strong association signals under the recessive model (Fig. 2B and Supplementary Table S8). In general, the significant burden identified in the majority of CoQ deficiency-related genes confirmed that these genes harbor an excess of rare exonic and UTR variants in the SUD and SIDS cohorts compared to the general population.
Burden testing of rare exonic and UTR variants identified in human CoQ deficiency-related genes. The x-axis represents the expected –log10(P) under a uniform distribution of p-values. The y-axis shows the observed –log10(P) from the burden testing data. Each data point represents a single gene. Genes highlighted in red indicate that there is a significant burden under both the dominant and the recessive models. Genes highlighted in orange indicate that there is a significant burden under the dominant model only. Genes in gray indicate that there is no significant burden under either model. (A) Significant genetic burden was observed in 17 genes (16 dominant and one both) in the SUD cohort. (B) Significant genetic burden was observed in 34 genes (31 dominant and 3 both) in the SIDS cohort
Abnormal ECG patterns
A total of 3 male and 2 female mice from the 4-NB group died unexpectedly during the night between week 6 and week 7. For the remaining mice, electrophysiological and morphological measurements were performed during week 9. To investigate the effect of CoQ deficiency on cardiac electrical activity, the ECG and echocardiographic patterns of the 4-NB and control groups were compared under equivalent HR conditions. ECG analysis showed that most parameters were not affected by the decrease in myocardial CoQ concentration. However, the PR interval was significantly prolonged in the 4-NB group compared with the control groups, irrespective of sex (Fig. 3). Moreover, during the same observation period, the 4-NB group developed more frequent isolated arrhythmic events as compared to the Ctrl-B group, including premature ventricular contraction (PVC), premature atrial contraction (PAC) and atrioventricular block (AVB) (Fig. 4).
Comparative analysis of electrocardiographic observations in the 4-NB and control groups. Each data point represents the average value of 3 replicates for the same mice. For both males (A-D) and females (E-H), QRS and QT intervals were similar between groups at steady heart rate, whereas PR interval was significantly longer in the 4-NB group (N male = 6; N female = 7) compared to Ctrl-A (N both = 9) and Ctrl-B (N both = 9) (*P < 0.05; **P < 0.005)
Differences in the occurrence of arrhythmic events and representative surface ECG recordings. (A) Colored cells indicate different scenarios where certain types of arrhythmic events were observed for at least once during the measurements. (B-D) The total number of subjects with different arrhythmic events observed. (E-H) The illustration of normal ECG recordings versus typical AVB, PAC, and PVC
Morphological and histological characteristics
Overall, the body weight increase of the 4-NB group was slower than that of the control groups throughout the growth phase. Significant differences in body weight and heart weight were observed between the 4-NB and control groups at week 9. However, the heart weight to body weight ratio (HW/BW) remained unchanged after 6 weeks of treatment (Supplementary Figure S1). In terms of echocardiographic patterns, the IVS, LVID and LVPW thickness were generally reduced in the 4-NB group. The difference was particularly evident in female mice, as LVPW at end systole was the only parameter with a statistically significant difference between groups (Table 1). Nevertheless, no difference in EF and FS was observed.
In general, no obvious structural defects of the heart or other organs were observed at autopsy. To assess the degree of fibrosis in the different groups, the histological characteristics of the mouse heart sections were further examined using Masson’s trichrome staining. As shown in representative histological images (Supplementary Figure S2A-C), no significant cardiomyocyte changes were observed in the 4-NB group. CoQ quantification of frozen heart tissues was then performed to validate whether the CoQ deficiency model was successfully constructed. The correlation coefficient (R2) of the regression fitting was 0.9991 for CoQ9, indicating a satisfactory quantitative relationship between MS response and CoQ9 concentration. As expected, the myocardial CoQ9 concentration was significantly lower in the 4-NB group compared to the control groups (Supplementary Figure S2D-E).
Discussion
Due to the essential role of CoQ in all energy-dependent processes of the heart, CoQ deficiency is known to be involved in various cardiac diseases [16]. However, the association between CoQ deficiency and SUD has not been investigated. Here, we present evidence from both the genetic level and physiological levels to support that CoQ deficiency is a previously overlooked predisposing factor for SUD. Re-evaluation of our exome sequencing data revealed that both the SUD and SIDS cohorts carried a substantial number of rare variants with likely functional effects in the 44 CoQ deficiency-related genes. Although pathogenic or conflicting clinical evidence has been previously reported for some of these variants, more than half of the variants identified in either the SUD or SIDS cohorts remain unexplored. Combined with the results from the burden tests and the fact that all of these variants were ultra-rare (MAF < 0.1% in gnomAD), it is highly likely that a substantial proportion of them are also clinically relevant for different CoQ deficiency phenotypes. However, since the clinical symptoms of mild CoQ deficiency are very often non-specific and CoQ is not chemically stable [14], it can be difficult to determine whether the variant carriers were suffering from CoQ deficiency by content assay of human CoQ10 in forensic samples.
In terms of cardiac electrical activity, the 4-NB induced CoQ deficiency mouse group had a significantly prolonged PR interval and a higher incidence of arrhythmic events, suggesting that CoQ deficiency is an independent pathophysiological condition that promotes cardiac arrhythmia. Furthermore, the incidence of AVB in the 4-NB group was more than twice that of the two control groups, even though the sample size of the 4-NB group was smaller. Since the AVB events recorded in our study were mostly accompanied by PR prolongation, these observations are most likely to be vagally-mediated AVB rather than paroxysmal AVB [30]. Although vagally-mediated AVB could lead to neutrally-mediated syncope, it is generally considered to be benign. Nevertheless, due to its poor recognition and unpredictability, its prevalence and consequences might be underestimated, especially in apparently healthy young adults [31]. Our findings also highlight the need for further evaluation of the prognostic significance of vagally-mediated AVB. Another important finding of our study is that 3 male mice and 2 female mice of the 4-NB group died at night during week 6 to 7 without any apparent injury. However, since no ECG or symptoms were recorded prior to death, we were unable to determine whether the cause of death was cardiac arrhythmia. According to previous reports, vagally-mediated AVB appears to be more common at night [32], which could be due to an acute increase in vagal tone during sleep. In a recent epidemiological study, Ramireddy et al. reported that female sex and central nervous system-affecting medications were independently associated with nocturnal sudden cardiac death [33]. However, since humans and mice have completely reversed circadian rhythms, there might be little correlation between the death in our 4-NB model and increased vagal tone.
According to previous studies, CoQ deficiency is common in cardiomyopathy and has been reported to be associated with chronic heart failure [16, 34]. However, no indicative echocardiographic features or histological findings were identified in our 4-NB group. This is most likely because our intervention period is too short for obvious morphological changes. Instead, we observed a significant effect of 6 weeks of 4-NB treatment on overall growth rate, resulting in reduced body and heart size and weight. Growth retardation is a commonly observed phenotype in patients with primary CoQ deficiency [35]. Combined with the finding that myocardial CoQ9 concentration was significantly lower in the 4-NB group compared to the control groups, we considered the abnormal growth curves of 4-NB treated mice further confirm that our CoQ deficiency model was able to mimic primary CoQ deficiency in its early stage.
As a typical polygenic disease, both primary and secondary CoQ deficiencies have shown a wide clinical variability, including the age of onset, the severity of phenotype and the degree of CoQ reduction in tissues [36]. Since secondary CoQ deficiency-related genes are not involved in CoQ biosynthesis, the functional effects of P/LP variants in these genes remain unclear. As a secondary CoQ deficiency-related gene and a well-known disease-causing gene for the Huntington’s disease, HTT has recently been associated with progressive cardiac arrhythmia and ECG abnormalities [37]. Although the underlying mechanism of cardiac involvement in Huntington’s disease is not fully understood, these observations suggest that HTT dysfunction is an independent predisposing factor for cardiac arrhythmia and SUD, whether accompanied by CoQ deficiency or not. Similarly, for the other secondary CoQ deficiency-related genes identified in this study, their actual role in SUD and the underlying pathogenic mechanisms deserve further investigation.
In the SUD and SIDS cases where we have identified genetic variants predisposing to CoQ deficiency, a small proportion of P/LP variants or VUS are also present in genes associated with cardiovascular/metabolic diseases [20, 21]. Although the identification of P/LP variants in certain genes is usually considered strong pathogenic evidence [10, 11], there is still no consensus on VUS due to the conflicting interpretations of their deleteriousness [38]. As the number of SUD susceptibility genes increases, a possible explanation for the phenotypic severity difference observed in VUS carriers is that there may be a joint effect of multiple genetic variants. Based on the multifactorial model of SUD [39, 40], there may be multiple genetic variants contributing to lethal arrhythmia. The effect of a single VUS on cardiac function might be limited. However, once combined with other intrinsic or extrinsic predisposing factors (for example, alcohol intake or physical exercise), the threshold for irreversible consequences could be reached. Based on our findings, genetic variants predisposing to CoQ deficiency could be one such intrinsic factor that increases the risk of SUD.
Currently, the interpretation of molecular autopsy findings in SUD still follows the logic of the management of monogenic diseases. Thus, the genetic investigation of SUD is mainly focused on very limited variants with the most prominent functional effects (e.g. P/LP variants in ion channel-encoding genes). However, a polygenic risk score that allows the estimation of combined SUD risk from multiple genetic variants could be developed, similar to the recently proposed strategy for arrhythmia risk assessment [41]. In future studies, efforts should be made to develop such a score, in order to accurately predict individualized SUD risk in suspected deceased. Although our work provided only preliminary evidence that CoQ deficiency may predispose to SUD via an increased risk of cardiac arrhythmia, the genetic and physiological findings suggest that CoQ deficiency-related genes should also be considered in the molecular autopsy of SUD. However, as the dysfunction of these genes might not have the same magnitude of effect as the dysfunction of ion channel-encoding genes, appropriate weights of different genes should be included.
It is also worth noting that one of the LP variants (ACADVL: rs371316167) identified in SIDS100 was previously reported in our study [21], as ACADVL is also a known susceptibility gene for SUD and SIDS. However, this variant was previously classified as VUS. The change of pathogenicity classification in patients with genetic diseases is frequently observed in clinical practice [42], largely due to the rapid emergence of new evidence provided by ongoing genotype-phenotype correlation studies, constantly updated population databases, and rapidly iterated prediction algorithms. Therefore, periodic re-evaluation of rare variants originally classified as ambiguous is encouraged [43], as it might provide the forensic experts with new evidence to explain the previously unexplained death.
Our current study has several limitations. First, we were not able to clarify whether the observed difference in the number of variants between the SUD and SIDS cohorts was simply due to sampling error, or whether there are actually different genetic backgrounds among unexplained death cases at different ages. Besides, our CoQ deficiency mouse model was drug-induced, which might not accurately simulate real patients with endogenously reduced CoQ levels caused by genetic defects. In future studies, telemetry ECG measurements could be performed on a conditional gene knockout mouse model to obtain more comprehensive electrophysiological properties. In addition, it is important for subsequent studies to independently validate the actual contribution of different CoQ deficiency-related genes to SUD through multi-center studies and functional assays.
Conclusion
In conclusion, we observed a significant genetic burden of human CoQ deficiency-related genes in the SUD and SIDS cohorts. Further electrophysiological and morphological investigation revealed a significantly prolonged PR interval and an increased incidence of AVB in the 4-NB-induced CoQ deficiency mouse model, independent of sex. Our results suggest that CoQ deficiency may predispose to sudden death via an increased risk of cardiac arrhythmia. Therefore, CoQ-deficiency-related genes should be considered in the molecular autopsy of SUD.
Data availability
Pathogenic or likely pathogenic variants have been submitted to the Leiden Open Variation Database (http://databases.lovd.nl/shared/diseases). All data will be provided upon request to the first or corresponding authors.
References
Adabag AS, Peterson G, Apple FS et al (2010) Etiology of sudden death in the community: results of anatomical, metabolic, and genetic evaluation. Am Heart J 159:33–39
Hayashi M, Shimizu W, Albert CM (2015) The spectrum of epidemiology underlying sudden cardiac death. Circ Res 116:1887–1906
Bagnall RD, Weintraub RG, Ingles J et al (2016) A prospective study of Sudden Cardiac Death among children and young adults. N Engl J Med 374:2441–2452
Lynge TH, Nielsen JL, Risgaard B et al (2023) Causes of sudden cardiac death according to age and sex in persons aged 1–49 years. Heart Rhythm 20:61–68
Yazdanfard PD, Christensen AH, Tfelt-Hansen J et al (2020) Non-diagnostic autopsy findings in sudden unexplained death victims. BMC Cardiovasc Disord 20:58
Neubauer J, Kissel CK, Bolliger SA et al (2022) Benefits and outcomes of a new multidisciplinary approach for the management and financing of sudden unexplained death cases in a forensic setting in Switzerland. Forensic Sci Int 334:111240
Krous HF, Beckwith JB, Byard RW et al (2004) Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and Diagnostic Approach. Pediatrics 114:234–238
Zeppenfeld K, Tfelt-Hansen J, de Riva M et al (2022) 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 43:3997–4126
Miles CJ, Behr ER (2016) The role of genetic testing in unexplained sudden death. Transl Res 168:59–73
Ackerman MJ, Priori SG, Willems S et al (2011) HRS/EHRA Expert Consensus Statement on the state of genetic testing for the Channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm 8:1308–1339
Stiles MK, Wilde AAM, Abrams DJ et al (2021) 2020 APHRS/HRS expert consensus statement on the investigation of decedents with sudden unexplained death and patients with sudden cardiac arrest, and of their families. Heart Rhythm 18:e1–e50
Acosta MJ, Vazquez Fonseca L, Desbats MA et al (2016) Coenzyme Q biosynthesis in health and disease. Biochim Biophys Acta 1857:1079–1085
Turunen M, Olsson J, Dallner G (2004) Metabolism and function of coenzyme Q. Biochim Biophys Acta 1660:171–199
Alcázar-Fabra M, Trevisson E, Brea-Calvo G (2018) Clinical syndromes associated with Coenzyme Q10 deficiency. Essays Biochem 62:377–398
Rodríguez-Aguilera JC, Cortés AB, Fernández-Ayala DJM et al (2017) Biochemical Assessment of Coenzyme Q(10) Deficiency. J Clin Med 6:27
Zozina IV, Covantev S, Goroshko AO et al (2018) Coenzyme Q10 in Cardiovascular and metabolic diseases: current state of the Problem. Curr Cardiol Rev 14:164–174
Christiansen SL, Hertz CL, Ferrero-Miliani L et al (2016) Genetic investigation of 100 heart genes in sudden unexplained death victims in a forensic setting. Eur J Hum Genet 24:1797–1802
Bagnall RD, Ingles J, Yeates L et al (2017) Exome sequencing-based molecular autopsy of formalin-fixed paraffin-embedded tissue after sudden death. Genet Med 19:1127–1133
Puckelwartz MJ, Pesce LL, Hernandez EJ et al (2024) The impact of damaging epilepsy and cardiac genetic variant burden in sudden death in the young. Genome Med 16:13
Neubauer J, Wang S, Russo G et al (2021) Re-evaluation of single nucleotide variants and identification of structural variants in a cohort of 45 sudden unexplained death cases. Int J Legal Med 135:1341–1349
Neubauer J, Lecca MR, Russo G et al (2017) Post-mortem whole-exome analysis in a large sudden infant death syndrome cohort with a focus on cardiovascular and metabolic genetic diseases. Eur J Hum Genet 25:404–409
Yubero D, Montero R, Santos-Ocaña C et al (2018) Molecular diagnosis of coenzyme Q10 deficiency: an update. Expert Rev Mol Diagn 18:491–498
Karczewski KJ, Francioli LC, Tiao G et al (2020) The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581:434–443
Wang Q, Pierce-Hoffman E, Cummings BB et al (2020) Landscape of multi-nucleotide variants in 125,748 human exomes and 15,708 genomes. Nat Commun 11:2539
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
Kopanos C, Tsiolkas V, Kouris A et al (2019) VarSome: the human genomic variant search engine. Bioinformatics 35:1978–1980
Guo MH, Plummer L, Chan YM et al (2018) Burden Testing of Rare variants identified through Exome sequencing via publicly available Control Data. Am J Hum Genet 103:522–534
Qu D, Schürmann P, Rothämel T et al (2023) Revisiting the association of sudden infant death syndrome (SIDS) with polymorphisms of NHE3 and IL13. Int J Legal Med 138:743–749
Forsman U, Sjoberg M, Turunen M et al (2010) 4-Nitrobenzoate inhibits coenzyme Q biosynthesis in mammalian cell cultures. Nat Chem Biol 6:515–517
Lee S, Wellens HJ, Josephson ME (2009) Paroxysmal atrioventricular block. Heart Rhythm 6:1229–1234
Alboni P, Holz A, Brignole M (2013) Vagally mediated atrioventricular block: pathophysiology and diagnosis. Heart 99:904–908
Rotondi F, Marino L, Lanzillo T et al (2012) Prolonged ventricular pauses in an Asymptomatic Athlete with Apparent Mobitz Type II second-degree atrioventricular block. Pacing Clin Electrophysiol 35:e210–e213
Ramireddy A, Chugh HS, Reinier K et al (2021) Sudden cardiac death during nighttime hours. Heart Rhythm 18:778–784
Mortensen SA, Rosenfeldt F, Kumar A et al (2014) The Effect of Coenzyme Q10 on Morbidity and Mortality in Chronic Heart failure: results from Q-SYMBIO: a Randomized double-blind trial. JACC Heart Fail 2:641–649
Wang N, Zheng Y, Zhang L et al (2021) A family segregating Lethal Primary Coenzyme Q10 Deficiency due to two novel COQ6 variants. Front Genet 12:811833
Mantle D, Millichap L, Castro-Marrero J et al (2023) Primary Coenzyme Q10 Deficiency: an update. Antioxidants 12:1652
Zhu Y, Shamblin I, Rodriguez E et al (2020) Progressive cardiac arrhythmias and ECG abnormalities in the Huntington’s disease BACHD mouse model. Hum Mol Genet 29:369–381
Scheiper-Welling S, Tabunscik M, Gross TE et al (2022) Variant interpretation in molecular autopsy: a useful dilemma. Int J Legal Med 136:475–482
Walsh R, Tadros R, Bezzina CR (2020) When genetic burden reaches threshold. Eur Heart J 41:3849–3855
Zheng J, Zheng D, Su T et al (2018) Sudden unexplained nocturnal death syndrome: the Hundred years’ Enigma. J Am Heart Assoc 7:e007837
Scrocco C, Bezzina CR, Ackerman MJ et al (2021) Genetics and genomics of arrhythmic risk: current and future strategies to prevent sudden cardiac death. Nat Rev Cardiol 18:774–784
Sarquella-Brugada G, Fernandez-Falgueras A, Cesar S et al (2022) Clinical impact of rare variants associated with inherited channelopathies: a 5-year update. Hum Genet 141:1579–1589
Martinez-Barrios E, Sarquella-Brugada G, Perez-Serra A et al (2023) Reevaluation of ambiguous genetic variants in sudden unexplained deaths of a young cohort. Int J Legal Med 137:345–351
Funding
This research was funded by the National Natural Science Foundation of China (82101971), the National Postdoctoral Science Foundation of China (2021M700815), the Swiss National Science Foundation (SNF; project-Nr. 320030_149456) and the Emma Louise Kessler Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval for human sample collection and exome analysis was provided by the local ethics committee in Zurich, Switzerland (KEK-ZH-Nr. 2013-0086). The animal study protocol was approved by the institutional board of animal ethics in Fudan University (20220228-016).
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, S., Haas, C., Wang, Z. et al. Coenzyme Q deficiency may predispose to sudden unexplained death via an increased risk of cardiac arrhythmia. Int J Legal Med (2024). https://doi.org/10.1007/s00414-024-03265-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00414-024-03265-5