Abstract
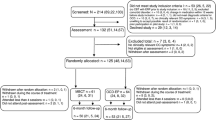
Obsessive–compulsive disorder (OCD) and major depression disorder (MDD) are underdiagnosed and undertreated mental disorders. Prior studies have verified the efficacy of the self-help manual My Metacognitive Training (myMCT) for patients with primary OCD. As depression and OCD share a number of (meta)cognitive biases and dysfunctional coping strategies, we examined the efficacy of myMCT in a mixed patient sample with OCD and/or depression. A total of 80 Italian-speaking individuals with symptoms of OCD and/or depression were randomized to either myMCT or to a waitlist control group (both groups had access to care as usual during the intervention). Post-assessment was carried out 6 weeks after inclusion. Scores on the Beck Depression Inventory-II scale (BDI-II) served as the primary outcome. Adverse effects were assessed with a newly devised self-report scale. Participants in the myMCT condition showed significant symptom improvement on the BDI-II scale at a medium to large effect size compared to the control group (using intention-to-treat and per protocol analyses). The intention-to-treat analyses yielded significant positive effects on the PHQ-9 scores and psychological as well as environmental well-being in favor of myMCT; for the OCI-R total score, group differences bordered significance in favor of the myMCT. The most prevalent adverse effects were feeling pressured by the suggested exercises or feeling bad due to not performing the exercises correctly. Our results indicate that the myMCT manual represents an effective program for patients with OCD as well as those with depressive symptoms in an Italian-speaking population. Adverse events due to unguided self-help deserve more attention in the future.

Similar content being viewed by others
References
Öst L-G, Havnen A, Hansen B, Kvale G (2015) Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clin Psychol Rev. 40:156–169
Olatunji BO, Davis ML, Powers MB, Smits JAJ (2013) Cognitive-behavioral therapy for obsessive–compulsive disorder: a meta-analysis of treatment outcome and moderators. J Psychiatr Res 47:33–41
Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS (2013) A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry 58:376–385
Stein DJ (2002) Obsessive-compulsive disorder. Lancet 2002:397–405
Veldhuis J, Dieleman JP, Wohlfarth T, Storosum JG, van Den Brink W, Sturkenboom MCJM et al (2012) Incidence and prevalence of ‘diagnosed OCD’ in a primary care, treatment seeking, population. Int J Psychiatry Clin Pract 16:85–92
Wahl K, Ertle A, Bohne A, Zurowski B, Kordon A (2011) Relations between a ruminative thinking style and obsessive-compulsive symptoms in non-clinical samples. Anxiety Stress Coping 24:217–225
Kohn R, Saxena S, Levav I, Saraceno B (2004) The treatment gap in mental health care. Bull World Health Organ 82:858–866
Rebello TJ, Marques A, Gureje O, Pike KM (2014) Innovative strategies for closing the mental health treatment gap globally. Curr Opin Psychiatry 27:308–314
Marques L, LeBlanc NJ, Wegarden HM, Timpano KR, Jenike M, Wilhelm S (2010) Barriers to treatment and service utilization in an internet sample of individuals with obsessive–compulsive symptoms. Depress Anxiety 27:470–475
Moritz S, Schröder J, Meyer B, Hauschildt M (2013) The more it is needed, the less it is wanted: attitudes toward face-to-face intervention among depressed patients undergoing online treatment. Depress Anxiety 30:157–167
García-Soriano G, Rufer M, Delsignore A, Weidt S (2014) Factors associated with non-treatment or delayed treatment seeking in OCD sufferers: a review of the literature. Psychiatry Res 220:1–10
Schwartz C, Schlegl S, Kuelz AK, Voderholzer U (2013) Treatment-seeking in OCD community cases and psychological treatment actually provided to treatment-seeking patients: a systematic review. J Obsessive Compuls Relat Disord 2:448–456
Mataix-Cols D, Marks IM (2006) Self-help with minimal therapist contact for obsessive-compulsive disorder: a review. Eur Psychiatry 21:75–80
Dèttore D, Pozza A, Andersson G (2015) Efficacy of technology-delivered cognitive behavioural therapy for OCD versus control conditions, and in comparison with therapist-administered CBT: meta-analysis of randomized controlled trials. Cogn Behav Ther 44:190–211
McIngvale E, Bakos-Block C, Hart J, Bordnick P (2012) Technology and obsessive compulsive disorder: an interactive self-help website for OCD. J Technol Hum Serv 30:128–136
Moritz S, Kersten JF, Dietl C, Aardema F, O’Connor K (2015) Evaluation of inference-based therapy (doubt therapy) as a self-help tool for obsessive-compulsive disorder. J Cogn Psychother 29:315–330
Tolin DF, Hannan S, Maltby N, Diefenbach GJ, Worhunsky P, Brady RE (2007) A randomized controlled trial of self-directed versus therapist-directed cognitive-behavioral therapy for obsessive–compulsive disorder patients with prior medication trials. Behav Ther 38:179–191
Mahoney AEJ, Mackenzie A, Williams AD, Smith J, Andrews G (2014) Internet cognitive behavioural treatment for obsessive compulsive disorder: a randomised controlled trial. Behav Res Ther 63:99–106
Andersson E, Enander J, Andrén P, Hedman E, Ljótsson B, Hursti T et al (2012) Internet-based cognitive behaviour therapy for obsessive–compulsive disorder: a randomized controlled trial. Psychol Med 42:2193–2203
Wootton BM, Dear BF, Johnston L, Terides MD, Titov N (2013) Remote treatment of obsessive–compulsive disorder: a randomized controlled trial. J Obsessive Compuls Relat Disord 2:375–384
Richards D, Richardson T (2012) Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev 32:329–342
Herbst N, Voderholzer U, Stelzer N, Knaevelsrud C, Hertenstein E, Schlegl S et al (2012) The potential of telemental health applications for obsessive–compulsive disorder. Clin Psychol Rev 32:454–466
Karyotaki E, Riper H, Twisk J, Hoogendoorn A, Kleiboer A, Mira A et al (2017) Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms a meta-analysis of individual participant data. JAMA Psychiatry 74:351–359
Obsessive Compulsive Cognitions Working Group (1997) Cognitive assessment of obsessive–compulsive disorder. Behav Res Ther 35:667–681
Obsessive Compulsive Cognitions Working Group (2003) Psychometric validation of the and the Interpretation of Intrusions Inventory: Part I. Behav Res Ther 41:863–878
Obsessive Compulsive Cognitions Working Group (2005) Psychometric validation of the obsessive belief questionnaire and interpretation of intrusions inventory—Part 2: factor analyses and testing of a brief version. Behav Res Ther 43:1527–1542
Hayes SC, Masuda A, DeMey H (2003) Acceptance and commitment therapy and the third wave of behavior therapy. Dutch J Behav Ther 2:69–96
Hofmann SG, Asmundson GJG (2008) Acceptance and mindfulness-based therapy: new wave or old hat? Clin Psychol Rev 28:1–16
Kahl KG, Winter L, Schweiger U (2012) The third wave of cognitive behavioural therapies. Curr Opin Psychiatry 25:522–528
Moritz S, Jelinek L (2007) Association splitting—self-help guide for reducing obsessive thoughts. VanHam Campus Verlag, Hamburg
Moritz S, Jelinek L, Klinge R, Naber D (2007) Fight fire with fireflies! Association splitting: a novel cognitive technique to reduce obsessive thoughts. Behav Cogn Psychother 35:631–635
Rodríguez-Martín BC, Moritz S, Molerio-Pérez O, Gil-Pérez P (2012) Effectiveness of association splitting in reducing unwanted intrusive thoughts in a nonclinical sample. Behav Cogn Psychother 41:1–8
Moritz S, Russu R (2013) Further evidence for the efficacy of association splitting in obsessive-compulsive disorder. An internet study in a Russian-speaking sample. J Obsessive Compuls Relat Disord 2:91–98
Moritz S, Jelinek L (2011) Further evidence for the efficacy of association splitting as a self-help technique for reducing obsessive thoughts. Depress Anxiety 28:574–581
Moritz S, Hauschildt M, Murray SC, Pedersen A, Krausz M, Jelinek L (2018) New wine in an old bottle? Evaluation of myMCT as an integrative bibliotherapy for obsessive–compulsive disorder. J Obsessive Compuls Relat Disord 16:88–97
Rüegg N, Moritz S, Westermann S (2018) Metacognitive training online: a pilot study of an internet-based intervention for people with Schizophrenia. Z Neuropsychol. 29:1. https://doi.org/10.1024/1016-264X/a000213
Moritz S, Aravena SC, Guczka SR, Schilling L, Eichenberg C, Raubart G et al (2011) Knock, and it will be opened to you? An evaluation of meridian-tapping in obsessive–compulsive disorder (OCD). J Behav Ther Exp Psychiatry 42:81–88
Hauschildt M, Schröder J, Moritz S (2016) Randomized-controlled trial on a novel (meta-)cognitive self-help approach for obsessive–compulsive disorder (‘myMCT’). J Obsessive Compuls Relat Disord 10:26–34
Philipp R, Kriston L, Lanio J, Kühne F, Härter M, Moritz S et al (2019) Effectiveness of metacognitive interventions for mental disorders in adults—a systematic review and meta-analysis (METACOG). Clin Psychol Psychother 26:227–240
Barbui C, Papola D, Saraceno B (2018) Forty years without mental hospitals in Italy. Int J Ment Health Syst 12:43
Lora A (2009) An overview of the mental health system in Italy. Ann Ist Super Sanita 45:5–16
Ferrannini L, Ghio L, Gibertoni D, Lora A, Tibaldi G, Neri G et al (2014) Thirty-five years of community psychiatry in Italy. J Nerv Ment Dis 202:432–439
Osland S, Arnold PD, Pringsheim T (2018) The prevalence of diagnosed obsessive compulsive disorder and associated comorbidities: a population-based Canadian study. Psychiatry Res 268:137–142
Abramowitz JS, Storch EA, Keeley M, Cordell E (2007) Obsessive–compulsive disorder with comorbid major depression: what is the role of cognitive factors? Behav Res Ther 45:2257–2267
Brown TA, Antony MM, Barlow DH (1992) Psychometric properties of the Penn state worry questionnaire in a clinical anxiety disorders sample. Behav Res Ther 30:33–37
Shaw AM, Carbonella JY, Arditte Hall KA, Timpano KR (2017) Obsessive–compulsive and depressive symptoms: the role of depressive cognitive styles. J Psychol 151:532–546
Sun X, Zhu C, So SHW (2017) Dysfunctional metacognition across psychopathologies: a meta-analytic review. Eur Psychiatry 45:139–153
Yap K, Mogan C, Kyrios M (2012) Obsessive–compulsive disorder and comorbid depression: the role of OCD-related and non-specific factors. J Anxiety Disord 26:565–573
Dar KA, Iqbal N (2015) Worry and rumination in generalized anxiety disorder and obsessive compulsive disorder. J Psychol 149:866–880
Exner C, Martin V, Rief W (2009) Self-focused ruminations and memory deficits in obsessive–compulsive disorder. Cognit Ther Res 33:163–174
Ghamari Kivi H, Mohammadipour Rik N, Sadeghi MF (2013) Explanation of obsessive–compulsive disorder and major depressive disorder on the basis of thought–action fusion. Iran J Psychiatry Behav Sci 7:44–50
Halvorsen M, Hagen R, Hjemdal O, Eriksen MS, Sørli ÅJ, Waterloo K et al (2015) Metacognitions and thought control strategies in unipolar major depression: a comparison of currently depressed, previously depressed, and never-depressed individuals. Cognit Ther Res 39:31–40
Hansmeier J, Exner C, Rief W, Glombiewski JA (2016) A test of the metacognitive model of obsessive–compulsive disorder. J Obsessive Compuls Relat Disord 10:42–48
Jacoby RJ, Leonard RC, Riemann BC, Abramowitz JS (2014) Predictors of quality of life and functional impairment in obsessive–compulsive disorder. Compr Psychiatry 55:1195–1202
Moradi M, Fata L, Ahmadi Abhari A, Abbasi I (2014) Comparing attentional control and intrusive thoughts in obsessive–compulsive disorder, generalized anxiety disorder and non clinical population. Iran J Psychiatry 9:69–75
Motivala SJ, Arellano M, Greco RL, Aitken D, Hutcheson N, Tadayonnejad R et al (2018) Relationships between obsessive-compulsive disorder, depression and functioning before and after exposure and response prevention therapy. Int J Psychiatry Clin Pract 22:40–46
Moritz S, Fieker M, Hottenrott B, Seeralan T, Cludius B, Kolbeck K et al (2015) No pain, no gain? Adverse effects of psychotherapy in obsessive–compulsive disorder and its relationship to treatment gains. J Obsessive Compuls Relat Disord 5:1. https://doi.org/10.1016/j.jocrd.2015.02.002
Beck AT, Steer RA, Brown GK (1996) Beck depression inventory, 2nd edn. The Psychological Corporation, San Antonio
Sica C, Ghisi M (2007) The Italian versions of the Beck Anxiety Inventory and the Beck Depression Inventory-II: psychometric properties and discriminant power. In: Lang MA (ed) Leading-edge psychological tests and testing research. Nova Science Publishers, Hauppauge, pp 27–50
Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G et al (2002) The Obsessive–Compulsive Inventory: development and validation of a short version. Psychol Assess 14:485–496
Abramowitz JS, Deacon BJ (2006) Psychometric properties and construct validity of the Obsessive–Compulsive Inventory-Revised: replication and extension with a clinical sample. J Anxiety Disord 20:1016–1035
Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB et al (2007) The OCI-R: validation of the subscales in a clinical sample. J Anxiety Disord 21:394–406
Coles ME, Cook LM, Blake TR (2007) Assessing obsessive compulsive symptoms and cognitions on the internet: evidence for the comparability of paper and Internet administration. Behav Res Ther 45:2232–2240
Sica C, Ghisi M, Altoè G, Chiri LR, Franceschini S, Coradeschi D et al (2009) The Italian version of the Obsessive Compulsive Inventory: its psychometric properties on community and clinical samples. J Anxiety Disord 23:204–211
Baer L, Brown-Beasley MW, Sorce J, Henriques AI (1993) Computer-assisted telephone administration of a structured interview for obsessive–compulsive disorder. Am J Psychiatry 150:1737–1738
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR et al (1989) The Yale–Brown Obsessive Compulsive Scale II. validity. Arch Gen Psychiatry 46:1012–1016
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al (1989) The Yale–Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 46:1006–1011
Melli G, Avallone E, Moulding R, Pinto A, Micheli E, Carraresi C (2015) Validation of the Italian version of the Yale-Brown Obsessive Compulsive Scale-Second Edition (Y-BOCS-II) in a clinical sample. Compr Psychiatry 60:86–92
Schaible R, Armbrust M, Nutzinger DO (2001) Yale-Brown Obsessive Compulsive Scale: sind Selbst- und Fremdrating äquivalent? [Yale-Brown Obsessive Compulsive Scale: are self-rating and interview equivalent measures?]. Verhaltenstherapie 11:298–303
Steketee G, Frost R, Bogart K (1996) The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behav Res Ther 34:675–684
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9. J Gen Intern Med 16:605–613
Rizzo R, Piccinelli M, Mazzi MA, Bellantuono C, Tansella M (2000) The Personal Health Questionnaire: a new screening instrument for detection of ICD-10 depressive disorders in primary care. Psychol Med 30:831–840
Skevington SM, Lotfy M, O’Connell KA (2004) The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL Group. Qual Life Res 13:299–310
De Girolamo G, Rucci P, Scocco P, Becchi A, Coppa F, D’Addario A et al (2000) Quality of life assessment: validation of the Italian version of the WHOQOL-Brief. Epidemiol Psichiatr Soc 9:45–55
Rosenberg M (1965) Society and the adolescent self-image. Princeton University Press, Princeton
Schmidt J, Wittman WW (2008) Fragebogen zur Messung der Patientenzufriedenheit—ZUF-8. Diagn Verfahren Rehabil 255:248–255
Schmidt J, Nübling R, Lamprecht F, Wittmann W (1994) Patientenzufriedenheit am Ende psychosomatischer Rehabehandlungen. Zusammenhänge mit Behandlungs- und Ergebnisvariablen und prognostische Bedeutung. In: Lamprecht F, Johnen R (eds) Salutogenese. Ein neues Konzept in der Psychosomatik? VAS-Verlag: Frankfurt am Main, pp 271–28.
Kriz D, Nübling R, Steffanowski A, Rieger J, Schmidt J (2008) Patientenzufriedenheit: psychometrische reanalyse des ZUF-8. Deutsche Rentenversicherung Bund, Berlin
Borm GF, Fransen J, Lemmens WA (2007) A simple sample size formula for analysis of covariance in randomized clinical trials. J Clin Epidemiol 60:1234–1238
Kenward MG, Roger JH (1997) Small sample inference for fixed effects from restricted maximum likelihood. Biometrics 53:983–997
Hayes AF (2013) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press, New York
Storch EA, De Nadai AS, Conceição Do Rosário M, Shavitt RG, Torres AR, Ferrão YA et al (2015) Defining clinical severity in adults with obsessive–compulsive disorder. Compr Psychiatry. 1:4. https://doi.org/10.1016/j.comppsych.2015.08.007
Hezel DM, McNally RJ (2016) A theoretical review of cognitive biases and deficits in obsessive–compulsive disorder. Biol Psychol 121:221–232
Joormann J, Stanton CH (2016) Examining emotion regulation in depression: a review and future directions. Behav Res Ther 86:35–49
Moritz S, Stepulovs O, Schröder J, Hottenrott B, Meyer B, Hauschildt M (2016) Is the whole less than the sum of its parts? Full versus individually adapted metacognitive self-help for obsessive–compulsive disorder: a randomized controlled trial. J Obsessive Compuls Relat Disord 9:107–115
Acknowledgements
The authors wish to thank Kathy McKay for copyediting the manuscript.
Funding
The study was financed by internal funds.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Moritz, S., Bernardini, J. & Lion, D. Effects and side effects of a transdiagnostic bias modification intervention in a mixed sample with obsessive–compulsive and/or depressive symptoms—a randomized controlled trial. Eur Arch Psychiatry Clin Neurosci 270, 1025–1036 (2020). https://doi.org/10.1007/s00406-019-01080-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01080-3