Abstract
Background
This retrospective study investigated factors influencing time to treatment initiation (TTI) and the influence of TTI on overall survival (OS) of primary head and neck cancer (HNC) patients in cohorts from 2003, 2008 and 2013.
Methods
Two hundred and ninenty seven patients (78.8% men; median age: 62 years) were included. Kaplan–Meier analyses and multivariate Cox regression were performed to investigate OS.
Results
Mean times to treatment initiation (TTI) of 2003, 2008 and 2013 were 17.11 ± 18.00, 30.26 ± 30.08 and 17.30 ± 37.04 days, respectively. TTI for patients with T3/T4 tumors was higher than for T1/T2 (p = 0.010). In univariable analysis on OS, TTI > 5 days showed lower OS (p = 0.047). In multivariate analysis, longer TTI had no influence on lower OS [hazard ratio (HR) 1.236; 95% CI 0.852–1.791; p = 0.264], but male gender [HR 2.342; 95% CI 1.229–4.466; p = 0.010], increased age [HR 1.026; 95% CI 1.008–1.045; p = 0.005], M1 [HR 5.823; 95% CI 2.252–15.058; p = 0.003], hypopharynx tumor [HR 2.508; 95% CI 1.571–4.003; p < 0.001] and oral cavity tumor [HR 1.712; CI 1.101–2.661; p = 0.017]. The year of treatment showed no significant effect on OS.
Conclusion
Median TTI seemed to be very short compared to other studies. There was no clear trend in the impact of TTI on OS from 2003 to 2013.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancers (HNCs) are often only diagnosed at an advanced stage [1]. Despite advances in diagnostics and treatment methods, the long-term prognosis remains poor with a 5-year survival rate of 68% [2]. Our main objective was to investigate treatment delays and their impact on overall survival (OS). Time to treatment initiation (TTI) describes delays in treatment of a patient, which mainly occur between the first visit to a doctor and the start of treatment. Delay can be caused, e.g., by waiting times for appointments for specialists, waiting times for diagnostic examination procedures, waiting times for therapies, misdiagnoses and repeated examinations. Therefore, recent studies investigated the impact of TTI together with possibilities of optimization. We prefer the term TTI instead of doctor’s delay. Doctor’s delay may also be used when the disease was not recognized by the doctor immediately. TTI is defined as the number of days between the histopathological diagnosis and the start of primary treatment. The main concern of longer intervals between tumor diagnosis and the start of therapy lies in possible tumor progression and reduced tumor control resulting in more extensive therapy and reduced OS as well as higher health costs [3]. Xiao et al. showed that a longer TTI results in tumor progression and the associated increase in mortality [4]. According to Jensen et al., the median tumor size in HNC doubles within 99 days [5]. Nevertheless, it makes sense to take sufficient time for precise tumor staging, planning and coordinating complex multidisciplinary treatment strategies.
Recent studies from the Unites States have shown that TTI has a significant influence on OS [4, 6]. Delays in TTI can be a significant problem for a patient’s prognosis. In this study, patients with HNC treated in 2003, 2008 and 2013 at a tertiary university hospital were included.
For this purpose, the influence of delays and waiting times on curative treatment in 2003, 2008 and 2013 as well as the impact of TTI on OS were analyzed. In addition, the intervals between examinations and the start of treatment were examined in detail.
Methods
Ethical considerations
This study was approved by the Ethics Committee of the Jena University Hospital (IRB No. 3204-07/11). The Ethics Committee waived the requirement for informed consent of the patients because the study had a non-interventional retrospective design and all data were analyzed anonymously.
Patients
This retrospective study was based on a dataset, which was provided by the Thuringian cancer registry in Jena, Germany. In total, 470 cases were registered in 2003, 2008 and 2013. Patients were excluded if they did not have a HNC, if treatment was performed outside the study period, if no treatment was started, if patients were noted twice and if there was insufficient documentation. Additional clinical data from the patients’ health care records were transferred to the dataset. Patients were divided into three groups according to the year in which they were treated. Histopathological confirmation of cancer was defined for the time of diagnosis. The pathological stages of the primary cancer were recorded using the UICC classification and TNM classification, 7th edition [7]. UICC classification was also used to classify tumor stages.
Charlson comorbidity index
The Charlson comorbidity index (CCI) is a method of assessing the influence of different comorbidities on a patient's mortality risk [8]. Depending on their relevance, 19 comorbidities are assigned numerical values which are then added together to evaluate the patient’s mortality risk. The dichotomous variable “CCI < median” or “CCI > median” was created to allow statistical analysis.
Statistical analysis
Descriptive statistics were performed using SPSS Statistics Version 25 (IBM Deutschland GmbH, 71,139 Ehningen, Germany). Absolute and relative frequencies of nominal parameters were calculated using cross tables. For the metric parameters, mean and the standard deviation as well as the median and the range were calculated. Statistical significance was performed using chi-square test for nominal variables. For metric variables, the Kruskal–Wallis test was chosen. Kaplan–Meier calculations were performed to assess the influence of the variables on OS of the patients. The log-rank test was performed to analyze the subgroups for significant differences in survival. P ≤ 0.05 was rated as statistically significant. Multivariable analyses were performed using a Cox proportional hazard ratio (HR) with a 95% confidence interval (CI). Variables were taken into account that showed significant differences in survival in the Kaplan–Meier analyses. Variables that fit together in terms of content were jointly investigated, for example, variables of general patient characteristics, tumor or treatment characteristics were included in several Cox models.
Results
Patient’s characteristics, tumor characteristics and treatment characteristics
In total, 297 HNC patients were included in the study. Of these, the initial diagnosis was made in 84 patients in 2003, in 108 patients in 2008 and in 105 patients in 2013. As shown in Table 1, men formed the majority of HNC patients (234 men, 78.8%). From 2003 to 2013, the proportion of women increased from 13.1% to 27.6%. The mean age at diagnosis was 61.1 years (5–102 years). The age at diagnosis increased from 2003 to 2013 (p = 0.024). Mean CCI was 4.8 ± 3.1. The mean duration of therapy from the first day of treatment to the last day of treatment was 86.4 ± 123.9 days (Stage I/II: 81.25 ± 108.61; Stage III/IV: 189.17 ± 141.92). The 2008 cohort showed a larger duration of therapy (p = 0.042). 41.0% of patients were alcohol drinking, 60.7% were smokers. The 2003 cohort was dominated by smokers (p < 0.001) and alcohol drinking patients (p < 0.001) compared to the 2008 and 2013 cohorts. More than half of the patients showed advanced T classification (T3/T4: 60%). The largest proportion was in 2013 (T3/T4: 74.3%). In all cohorts, UICC stage III/IV was over presented (2003: 77.8%, 2008: 73.3%, 2013: 85.3%). The distribution of HNC patients was mostly divided between oropharynx (20.5%), larynx (18.5%), oral cavity (12.1%), and hypopharynx (10.4%). Surgery was the most frequently used primary treatment modality (261 patients, 87.9%). In 2013, chemotherapy (p < 0.001) and immunotherapy (p = 0.007) were more frequently used than in the cohorts from 2003 to 2008. Chemo-radiation was more often performed in 2008 (p = 0.003).
Time to treatment initiation
The median TTI was 16 days (0–339). There was one patient initially declining treatment. This patient came back for treatment about nine month later explaining most of the 339 days of TTI. The frequency distribution is shown in Fig. 1. Table 2 shows the association of TTI with patients’ characteristics, histopathology and treatment. In 2008, men waited significantly longer than women with an average of 33.0 days compared to 20.2 days (p = 0.023). For men, treatment delay was significantly higher in 2008 than in the other two years (p < 0.001). For alcohol drinking patients (26.8 ± 31.7 days), TTI was significantly higher than for non-alcohol drinking patients (21.7 ± 33.5 days, p = 0.018). Alcohol drinking patients (p < 0.001) and non-alcohol drinking patients (p < 0.001) showed significantly higher waiting time in 2008 than in 2003 and 2013. TTI (26.5 ± 38.0 days) was for smokers significantly higher than for non-smokers (18.5 ± 19.1 days, p = 0.029) and showed higher waiting time in 2008 than in 2003 and 2013 (p < 0.001, p < 0.001). In 2013, a higher CCI showed a longer TTI (24.2 ± 50.4 days) than a lower CCI (11.1 ± 15.9 days, p = 0.046). Considering the UICC classification, patients with a higher stage (stage III/IV) waited significantly longer than patients with a lower stage (stage I/II, p = 0.021) only in 2008. HNC patients with oropharynx (p = 0.047), hypopharynx (p = 0.020) and esophagus (p < 0.001) tumor had significantly longer waiting times than patients with other localization. Patients with HNC of the parotid gland (p = 0.003), ear (p = 0.027), facial skin (p < 0.001) and unspecified HNC (p = 0.002) had a shorter TTI than patients with other localizations. TTI was longer in most of the localizations in 2008 than in 2003 and 2013 (mean TTI 22.0 ± 30.7, p < 0.001). Considering treatment characteristics, average TTI of surgery was 17.9 ± 26.3 days. The longest TTI for surgery was seen in 2008 with 30.3 ± 30.1 days, which was longer than in 2003 and 2013 (p < 0.001). TTI for chemo-radiation was about twice as long as for surgery with an average TTI of 45.77 ± 42.4 days. The TTI for chemo-radiation did not vary significantly between the three cohorts (p = 0.137). In conclusion, HNC patients of 2008 had longer time lags until treatment initiation compared to HNC patients of 2003 and 2013.
Overall survival
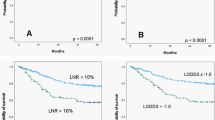
The univariable analysis (Supplementary Table S1) showed that men had lower OS than woman (p = 0.002; Fig. 2). Alcoholic drinking patients (p < 0.001) and smokers (p = 0.002) had also lower OS. A CCI greater than the median also showed a lower survival probability (p < 0.001). OS was significantly higher if the age of HNC diagnosis was below the median than above the median (p = 0.029). HNC patients treated in 2013 showed lower OS (p = 0.013). The estimated two-year OS was 73.7% and the five-year OS was 56.7%. Overall, the different cohorts showed no significant effect on OS (p = 0.119). Additionally, patients with TTI > 5 days showed lower OS than patients with TTI ≤ 5 days (p = 0.047). Significantly longer survival was seen after performing surgical treatment in all cohorts (p < 0.001). Patients with a clinical T1/2 tumor showed significantly higher OS than patients with a clinical T3/4 Tumor (p < 0.001). Patients who had distant metastases (M1) showed lower OS than patients without distant metastases (M0; p < 0.001). Clinical UICC stage I/II was associated with better survival than advanced UICC stage III/IV (p = 0.002). This result was only seen in the cohort of 2008 (p = 0.005), while the cohorts of 2003 and 2013 did not show higher OS for UICC stage I/II. Among HNC localizations, HNC of the cavity of the mouth (p = 0.036) and hypopharynx (p < 0.001) was associated with a significant lower OS. Overall, significant influence of the different variables (gender, CCI, age, clinical T, clinical UICC and hypopharynx) on OS was more seen in the cohort of 2008 than in the cohorts of 2003 and 2013. Overall, there was no clear significant influence on OS between the different cohorts (Fig. 2).
Multivariable analyses (Table 3) were performed for all variables influencing OS significantly in the univariable analysis. Men had a 2.3-fold increased hazard of death than women (HR 2.342; 95% CI 1.229–4.466; p = 0.010). HR for alcohol consumption was 2.054 indicating that HNC patients are more than twice likely to die from alcohol drinking than HNC patients without alcoholism (HR 2.054; 95% 1.319–3.197; p = 0.002). Increased age at diagnosis (HR 1.026; 95% CI 1.008–1.045; p = 0.005] and higher CCI (HR 1.109; 95% CI 1.049–1.173; p = 0.001) showed a slightly increased hazard of death. When the different cohorts were considered as additional parameter, similar results emerged. The year itself did not show a significant influence. The presence of distant metastases (M1) showed a 5.8-fold increased hazard of death than patients without distant metastases (M0) (HR 5.823; 95% CI 2.252–15.058; p = 0.003). Within the cohorts of 2003 and 2013, some factors had significant impact on OS not seen in the cohort of 2008. Patients of 2013 had 0.3-fold increased hazard of death compared to patients of 2003 (HR 0.327; 95% CI 0.139–0.765; p = 0.010). Oral cavity tumors had a 1.7-fold increased hazard of death (HR 1.712; CI 1.101–2.661; p = 0.017) and a hypopharynx tumor had a 2.5-fold increased hazard of death (HR 2.508; 95% CI 1.571–4.003; p < 0.001). A TTI lower or higher the median had no impact on OS (HR 1.236; 95% CI 0.852–1.791; p = 0.264), but TTI ≤ 5 days still showed an effect on OS (HR 1.591; 95% CI 0.997–2.537; p = 0.051).
Discussion
In this retrospective study, median TTI was 16 days. TTI > 5 days showed significantly lower OS in univariable statistics but not in multivariable statistics. A significantly higher TTI was seen in alcoholism, smoking, patients with combined radio-chemotherapy as primary or adjuvant therapy, higher clinical T stage and cancer of the oropharynx, hypopharynx and esophagus. Significantly lower TTI was seen in patients undergoing surgery, tumors of the parotid gland, facial skin, ear and unspecified HNC. Alcohol has been shown to be a risk factor for HNC of oral cavity and pharyngeal tumors [9]. Alcoholism had a significant impact on waiting time, with a median TTI of 21 days for alcoholics and 15 days for non-alcoholics. Alcoholism can negatively influence compliance and missed appointments can lead to a prolongation of TTI. Cigarette smoking patients showed similar results to alcohol drinking patients. Alcohol drinking patients and smoking patients have in general more comorbidity. Therefore, alcohol and smoking could also have an additional effect via the comorbidity of the patients on TTI. This was not analyzed in this study. A high proportion of stage III/IV was seen. These results are in line with the results of the current literature [1, 3, 10,11,12]. It has been suggested that delays are related to lack of awareness of symptoms, the patient's own perception of risk and other psychosocial barriers to treatment in time. In the literature, median TTI varies from 20 to 48 days [3, 6, 10, 11, 13,14,15,16,17,18]. The median TTI of 16 days in this study was shorter. TTI was found to be significantly higher in 2008 than in 2003 and 2013, while there was no continuous trend over the period. In the study of Murphy et al. TTI increased from 19 days in 1998 to 30 days in 2011 [6]. Murphy et al. suggested that the increase in TTI is due to the pursuit of better care, advances in treatment and referral to high-volume centers. Academic facilities are disproportionately more affected to care transitions than comprehensive community health centers. An increase in complexity of treatment (improved surgical reconstruction, preoperative computer-guided reconstruction planning, increase in planning of intensity-modulated radiation) leads to a rising TTI [19]. Lyhne et al. showed that the diagnostic interval was reduced from 20 days in 1992 to 17 days in 2002 and to 13 days in 2010 [10]. In addition, a reduction in waiting times for radiotherapy in Denmark was achieved by the expansion and investment in radiotherapy facilities as a result of the Danish cancer control plans. The introduction of a fast-track system is also believed to have shortened TTI [10]. In a population-based study of 21,623 patients with oral cavity squamous cell carcinoma of the Taiwan Cancer Registry Database, a TTI of less than 30 days was associated to a better survival rate than a TTI of more than 30 days [11]. Surgery was the most common form of therapy with 93.1% in Taiwan. Patients who received primary radiotherapy or chemotherapy tended to have a longer TTI than patients who underwent primary surgery treatment [11].
The geographic regions and medical care are of varying quality and availability in-between the studies. In our study, most examinations were performed directly in the tertiary hospital. In other countries or other health care systems, further examinations may need a referral to another specialists outside the treating center. Treatment organization will be more difficult and requires more time. This may have an impact on TTI. Additionally, the different tumor localizations are not fully comparable. Most studies included a surgical treatment, radiotherapy and chemo-radiation. When only surgery was considered as primary therapy, median TTI was 13 days in the present study. Bilimoria et al. reported a significantly higher median TTI of 23 days for surgical treatment [20]. The waiting time for chemo-radiation as primary therapy was 45.7 days, more than double of the time of surgical treatment. The median was 34 days, similar to Bilimoria et al. with 31 days or Dahlke et al. with 34 days [20, 21]. Primary chemoradiation requires more preparation and organization. In the literature, TTI for primary chemoradiation or primary radiotherapy varies from 31 to 57 days [6, 15, 21,22,23,24].
Patients with a TTI greater than the median versus patients with a TTI less than the median showed no significant difference in OS. In contrast, patients with TTI > 5 days showed lower OS than patients with TTI ≤ 5 days in univariable statistics (p = 0.047) but only a trend in multivariable statistics (p = 0.051). Anyway, a TTI ≤ 5 days was reached in one quarter of the patients (27%). Van Harten et al. showed that the year of diagnosis is related significantly to treatment delay. Median TTI increased from 31 days between 1990 and 1994 to 38 to 41.5 days in the following periods (1995–1999, 2000–2004, 2005–2010) [25]. In another study by van Harten et al., TTI above the median of 37 days showed a significantly higher HR than waiting less than 37 days [3]. TTI of 61–90 days showed a higher mortality risk than a TTI less than 30 days [6]. In Tsai et al., OS was lower with a waiting time of more than 120 days versus a waiting time of less than 30 days [11]. In Xiao et al., HR was higher with a TTI after ≥ 70 days compared to TTI under 70 days [4]. In Polesel et al. 5-year OS decreased from 62% when waiting time was less than 30 days to 39% when waiting time was more than 90 days [17]. In Schutte et al. the 5-year OS was 78% for TTI up to 30 days and 58% for TTI above 30 days [26]. However, Morse et al. showed different results. In a multi-institution retrospective analysis of 33 819 cases of laryngeal squamous cell cancer (LSCC) based on the National Cancer Database (NCDB) from 2004 to 2013, TTI of 28 days in surgical patients was shown to be not associated with poorer OS in the different tumor localizations (cavity of the mouth, oropharynx, salivary glands and hypopharynx) [16]. TTI of 33 days in non-surgical patients and radiation delay were found to have a significant influence on OS. In contrast, Su et al. were able to show in their study from 2004 to 2009 that a TTI of > 6 weeks has a significant influence on OS. In the present study TTI > 5 days showed a significant lower OS, but only in univariate statistics.
Median TTI of 2003, 2008 and 2013 in this study was 13, 26 and 7 days. TTI was relatively short in all three cohorts. This might explain that small differences did not influence OS between the three cohorts.
Retrospective studies have limitations. The socioeconomic situation of the patients was not considered in this study. This is also a limiting factor, as socioeconomic status may also affect OS and TTI [27]. Furthermore, it might be that TTI was shorter in such patients who brought along relevant diagnostics at first presentation in the hospital. Information on brought-along diagnostics was not available. Furthermore, the retrospective design did not allow to analyze the patient’s influence on TTI (for instance, by non-compliance to appointment). Only in the case with a TTI of 339, this could be retraced to an initial therapy denial.
In literature, TTI was investigated to enable a reduction in waiting times. A first approach is the implementation of a fast-track and well-structured multidisciplinary appointment program. OS for HNC patients can be increased by reducing the time needed for patient referral and an early start of treatment [22]. Furthermore, the implementation of fast-track program has been shown to reduce TTI [28]. In Denmark, a fast-track system was introduced in 2007. TTI reduced from 47 days in 2002 to 25 days in 2010. In the Netherlands, a multidisciplinary first-day consultation (MFDC) was introduced in 2007. The MFDC shall establish a preliminary diagnostic plan and determine the diagnostic procedures in a multidisciplinary consultation from the departments of ear, nose and throat (ENT), oral and maxillofacial surgery, radiotherapy and special dental care. Patients are informed of their diagnostic plan at the end of the day. Van Huizen et al. evaluated the impact of MFDC on TTI and its compliance to Dutch health expectations to start treatment within 30 calendar days. TTI could be reduced with 8 days after 1 year of implementation of MFDC. Furthermore, 83% of patients received first treatment within 30 days instead of 52% before implementation of MFDC [29]. Schutte et al. described a fast-track program and showed a reduction of the median of specialist-to-diagnosis interval from 9 to 2 days and a reduction of TTI from 25 to 18 days [26]. 3-year OS was significantly higher for patients in the new system (84% vs. 72%). Such systems have been shown to increase efficiency in the diagnostic algorithm. To prevent delays in treatment, such a system could also be introduced in Germany. Especially HNC patients with significantly higher TTI in our study could benefit from a fast-track and multidisciplinary appointment program.
According to our analysis, longer TTI > 5 showed negative influence on OS of HNC patients. However, the present data analyses do not contradict the current literature. The findings of the present study need to be verified by further analyses in a prospective study.
Conclusion
This study investigated the impact of TTI on OS in a tertiary university hospital comparing three HNC patient cohorts from 2003, 2008, and 2013. TTI > 5 days showed lower OS in univariable but not in multivariable analysis. Overall, there was no clear trend in the impact of TTI on OS from the different cohorts. Mean numbers of TTI of 2003, 2008 and 2013 were 17.11, 30.26 and 17.30 days and showed no influence on OS of HNC. Overall, the waiting time in this study was very short with a median of 16 days. TTI was significantly influenced by variables, such as alcoholism, smoking, T classification and tumor localization. However, the findings of the present study need to be verified by further analyses in a prospective study.
References
Levy DA, Li H, Sterba KR, Hughes-Halbert C, Warren GW, Nussenbaum B et al (2020) Development and validation of nomograms for predicting delayed postoperative radiotherapy initiation in head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg 146:455–464
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM et al (2013) International classification of diseases for oncology (ICD-O)–3rd edition, 1st revision. World Health Organization, Malta
van Harten MC, Hoebers FJ, Kross KW, van Werkhoven ED, van den Brekel MW, van Dijk BA (2015) Determinants of treatment waiting times for head and neck cancer in the Netherlands and their relation to survival. Oral Oncol 51:272–278
Xiao R, Ward MC, Yang K, Adelstein DJ, Koyfman SA, Prendes BL et al (2018) Increased pathologic upstaging with rising time to treatment initiation for head and neck cancer: a mechanism for increased mortality. Cancer 124:1400–1414
Jensen AR, Nellemann HM, Overgaard J (2007) Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol 84:5–10
Murphy CT, Galloway TJ, Handorf EA, Egleston BL, Wang LS, Mehra R et al (2016) Survival impact of increasing time to treatment initiation for patients with head and neck cancer in the United States. J Clin Oncol 34:169–178
Sobin LH, Gospodarowicz MK, Wittekind C, IU Cancer (2009) TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, Hoboken
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Chen L, Gallicchio L, Boyd-Lindsley K, Tao XG, Robinson KA, Lam TK et al (2009) Alcohol consumption and the risk of nasopharyngeal carcinoma: a systematic review. Nutr Cancer 61:1–15
Lyhne NM, Christensen A, Alanin MC, Bruun MT, Jung TH, Bruhn MA et al (2013) Waiting times for diagnosis and treatment of head and neck cancer in Denmark in 2010 compared to 1992 and 2002. Eur J Cancer 49:1627–1633
Tsai WC, Kung PT, Wang YH, Huang KH, Liu SA (2017) Influence of time interval from diagnosis to treatment on survival for oral cavity cancer: A nationwide cohort study. PLoS ONE 12:e0175148
Göllnitz I, Inhestern J, Wendt TG, Buentzel J, Esser D, Böger D et al (2016) Role of comorbidity on outcome of head and neck cancer: a population-based study in Thuringia. Ger Cancer Med 5:3260–3271
Flukes S, Garry S, Hinton-Bayre A, Lindsay A (2019) Pre-treatment wait time for head and neck cancer patients in western Australia: description of a new metric and examination of predictive factors. ANZ J Surg 89:858–862
Hansen O, Larsen S, Bastholt L, Godballe C, Jørgensen KE (2005) Duration of symptoms: impact on outcome of radiotherapy in glottic cancer patients. Int J Radiat Oncol Biol Phys 61:789–794
Ho AS, Kim S, Tighiouart M, Mita A, Scher KS, Epstein JB et al (2018) Quantitative survival impact of composite treatment delays in head and neck cancer. Cancer 124:3154–3162
Morse E, Fujiwara RJT, Judson B, Mehra S (2018) Treatment delays in laryngeal squamous cell carcinoma: a national cancer database analysis. Laryngoscope 128:2751–2758
Polesel J, Furlan C, Birri S, Giacomarra V, Vaccher E, Grando G et al (2017) The impact of time to treatment initiation on survival from head and neck cancer in north-eastern Italy. Oral Oncol 67:175–182
Su WW, Lee YH, Yen AM, Chen SL, Hsu CY, Chiu SY et al (2021) Impact of treatment delay on survival of oral/oropharyngeal cancers: results of a nationwide screening program. Head Neck 43:473–484
Murphy CT, Galloway TJ, Handorf EA, Wang L, Mehra R, Flieder DB et al (2015) Increasing time to treatment initiation for head and neck cancer: an analysis of the National Cancer Database. Cancer 121:1204–1213
Bilimoria KY, Ko CY, Tomlinson JS, Stewart AK, Talamonti MS, Hynes DL et al (2011) Wait times for cancer surgery in the United States: trends and predictors of delays. Ann Surg 253:779–785
Dahlke S, Steinmann D, Christiansen H, Durisin M, Eckardt A, Wegener G et al (2017) Impact of time factors on outcome in patients with head and neck cancer treated with definitive radio(chemo)therapy. In Vivo 31:949–955
Fareed MM, Ishtiaq R, Galloway TJ (2018) Testing the timing: time factor in radiation treatment for head and neck cancers. Curr Treat Options Oncol 19:17
Guttmann DM, Kobie J, Grover S, Lin A, Lukens JN, Mitra N et al (2018) National disparities in treatment package time for resected locally advanced head and neck cancer and impact on overall survival. Head Neck 40:1147–1155
Stoker SD, Wildeman MA, Fles R, Indrasari SR, Herdini C, Wildeman PL et al (2014) A prospective study: current problems in radiotherapy for nasopharyngeal carcinoma in yogyakarta, indonesia. PLoS ONE 9:e85959
van Harten MC, de Ridder M, Hamming-Vrieze O, Smeele LE, Balm AJ, van den Brekel MW (2014) The association of treatment delay and prognosis in head and neck squamous cell carcinoma (HNSCC) patients in a Dutch comprehensive cancer center. Oral Oncol 50:282–290
Schutte HW, van den Broek GB, Steens SCA, Hermens R, Honings J, Marres HAM et al (2020) Impact of optimizing diagnostic workup and reducing the time to treatment in head and neck cancer. Cancer 126:3982–3990
Robertson G, Greenlaw N, Bray CA, Morrison DS (2010) Explaining the effects of socio-economic deprivation on survival in a national prospective cohort study of 1909 patients with head and neck cancers. Cancer Epidemiol 34:682–688
Sorensen JR, Johansen J, Gano L, Sørensen JA, Larsen SR, Andersen PB et al (2014) A “package solution" fast track program can reduce the diagnostic waiting time in head and neck cancer. Eur Arch Otorhinolaryngol 271:1163–1170
van Huizen LS, Dijkstra PU, van der Laan B, Reintsema H, Ahaus KTB, Bijl HP et al (2018) Multidisciplinary first-day consultation accelerates diagnostic procedures and throughput times of patients in a head-and-neck cancer care pathway, a mixed method study. BMC Health Serv Res 18:820
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Committee waived the requirement for informed consent of the patients because the study had a non-interventional retrospective design and all data were analyzed anonymously.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kouka, M., Engelhardt, M., Wittig, A. et al. No impact of time to treatment initiation for head and neck cancer in a tertiary university center in 2003, 2008 and 2013. Eur Arch Otorhinolaryngol 279, 4549–4560 (2022). https://doi.org/10.1007/s00405-022-07392-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07392-w