Abstract
Purpose
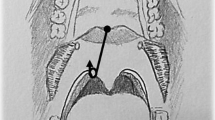
To evaluate the efficacy of barbed reposition pharyngoplasty (BRP) on sleepiness, anxiety, and depression o adult patients with obstructive sleep apnea (OSA).
Methods
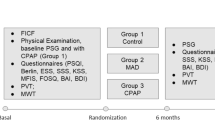
We performed a prospective multicentric study to assess functional outcomes in 20 OSA patients treated with BRP and compare the results with an observational group of 20 subjects. All recruited subjects performed at baseline and 6-months postoperative follow-up Polysomnography (PSG), daytime sleepiness scoring using the Epworth Sleepiness Scale (ESS), and anxiety and depression evaluation via the Beck Anxiety Inventory (BAI) and the Beck Depression Inventory-II (BDI-II) questionnaires.
Results
At follow-up the BRP demonstrated greater improvements in AHI (8.92 ± 2.29 vs. 30.66 ± 2.56; p < 0.001) and ODI (7.65 ± 2.39 vs. 24.55 ± 3.20; p < 0.001) than control at intergroup analysis. Surgical group reported significant data in daytime sleepiness (5.15 ± 1.19 vs. 13.15 ± 1.35; p < 0.001), anxiety (12.65 ± 3.11 vs. 24.2 ± 2.37; p < 0.001), and depression domains (5.85 ± 1.19 vs. 17.55 ± 3.24; p < 0.001). AHI, ODI, and advanced age have been shown to multiple regression as independent predictors of treatment response for mood domains (p < 0.001; p = 0.02; p = 0.041, respectively).
Conclusions
Patients with OSA may benefit from palate surgery, reducing not only the apnea and hypopnea index, daytime sleepiness but also associated mood comorbidities. However, further studies are needed to confirm our preliminary results to validate the evidence to date reported.



Similar content being viewed by others
References
Kapur VK, Auckley DH, Chowdhuri S et al (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506 (Published 2017 Mar 15)
Iannella G, Maniaci A, Magliulo G et al (2020) Current challenges in the diagnosis and treatment of obstructive sleep apnea syndrome in the elderly. Pol Arch Intern Med 130(7–8):649–654. https://doi.org/10.20452/pamw.15283
Rana D, Torrilus C, Ahmad W, Okam NA, Fatima T, Jahan N (2020) Obstructive sleep apnea and cardiovascular morbidities: a review article. Cureus 12(9):e10424. https://doi.org/10.7759/cureus.10424 (Published 2020 Sep 13)
Iannella G, Vicini C, Colizza A et al (2019) Aging effect on sleepiness and apneas severity in patients with obstructive sleep apnea syndrome: a meta-analysis study. Eur Arch Otorhinolaryngol 276(12):3549–3556. https://doi.org/10.1007/s00405-019-05616-0
Vicini C, De Vito A, Iannella G et al (2018) The aging effect on upper airways collapse of patients with obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 275(12):2983–2990. https://doi.org/10.1007/s00405-018-5163-5
Iannella G, Magliulo G, Maniaci A, Meccariello G, Cocuzza S, Cammaroto G, Gobbi R, Sgarzani R, Firinu E, Corso RM, Pace A, Gulotta G, Visconti IC, Di Luca M, Pelucchi S, Bianchi G, Melegatti M, Abita P, Solito C, La Mantia I, Grillo C, Vicini C (2021) Olfactory function in patients with obstructive sleep apnea: a meta-analysis study. Eur Arch Otorhinolaryngol 278(3):883–891. https://doi.org/10.1007/s00405-020-06316-w (Epub 2020 Sep 10 PMID: 32914257)
May AM, Van Wagoner DR, Mehra R (2017) OSA and cardiac arrhythmogenesis: mechanistic insights. Chest 151(1):225–241. https://doi.org/10.1016/j.chest.2016.09.014
Pace A, Iannella G, Rossetti V et al (2020) Diagnosis of obstructive sleep apnea in patients with allergic and non-allergic rhinitis. Medicina (Kaunas) 56(9):454. https://doi.org/10.3390/medicina56090454 (Published 2020 Sep 8)
Pollicina I, Maniaci A, Lechien JR, Iannella G, Vicini C, Cammaroto G, Cannavicci A, Magliulo G, Pace A, Cocuzza S, Di Luca M, Stilo G, Di Mauro P, Bianco MR, Murabito P, Bannò V, La Mantia I (2021) Neurocognitive performance improvement after obstructive sleep apnea treatment: state of the art. Behav Sci (Basel) 11(12):180
Althoff MD, Ghincea A, Wood LG, Holguin F, Sharma S (2021) Asthma and three colinear comorbidities: obesity, OSA, and GERD. J Allergy Clin Immunol Pract 9(11):3877–3884. https://doi.org/10.1016/j.jaip.2021.09.003
Reutrakul S, Mokhlesi B (2017) Obstructive sleep apnea and diabetes: a state of the art review. Chest 152(5):1070–1086. https://doi.org/10.1016/j.chest.2017.05.009
Hobzova M, Prasko J, Vanek J et al (2017) Depression and obstructive sleep apnea. Neuroendocrinol Lett 38:343–352
Aloia MS, Arnedt JT, Smith L et al (2005) Examining the construct of depression in obstructive sleep apnea syndrome. Sleep Med 6(2):115–121. https://doi.org/10.1016/j.sleep.2004.09.003
Dalmases M, Solé-Padullés C, Torres M et al (2015) Effect of CPAP on cognition, brain function, and structure among elderly patients with OSA: a randomized pilot study. Chest 148(5):1214–1223. https://doi.org/10.1378/chest.15-0171
Zheng D, Xu Y, You S et al (2019) Effects of continuous positive airway pressure on depression and anxiety symptoms in patients with obstructive sleep apnoea: results from the sleep apnoea cardiovascular endpoint randomised trial and meta-analysis. EClinicalMedicine 11:89–96
Ponce S, Pastor E, Orosa B et al (2019) The role of CPAP treatment in elderly patients with moderate obstructive sleep apnoea: a multicentre randomised controlled trial. Eur Respir J 54(2):1900518. https://doi.org/10.1183/13993003.00518-2019 (Published 2019 Aug 22)
Campos-Rodriguez F, Queipo-Corona C, Carmona-Bernal C et al (2016) Continuous positive airway pressure improves quality of life in women with obstructive sleep apnea. A randomized controlled trial. Am J Respir Crit Care Med 194(10):1286–1294
Labarca G, Saavedra D, Dreyse J, Jorquera J, Barbe F (2020) Efficacy of CPAP for improvements in sleepiness, cognition, mood, and quality of life in elderly patients with OSA: systematic review and meta-analysis of randomized controlled trials. Chest 158(2):751–764. https://doi.org/10.1016/j.chest.2020.03.049
Wang Y, Gao W, Sun M, Chen B (2012) Adherence to CPAP in patients with obstructive sleep apnea in a Chinese population. Respir Care 57(2):238–243. https://doi.org/10.4187/respcare.01136
Avellan-Hietanen H, Maasilta P, Bachour A (2020) Restarting CPAP therapy for sleep apnea after a previous failure. Respir Care 65(10):1541–1546. https://doi.org/10.4187/respcare.07766
Iannella G, Magliulo G, Di Luca M, De Vito A, Meccariello G, Cammaroto G, Pelucchi S, Bonsembiante A, Maniaci A, Vicini C (2020) Lateral pharyngoplasty techniques for obstructive sleep apnea syndrome: a comparative experimental stress test of two different techniques. Eur Arch Otorhinolaryngol 277(6):1793–1800
Iannella G, Magliulo G, Cammaroto G, Meccariello G, De Vito A, Pelucchi S, Ciorba A, Maniaci A, Cocuzza S, Gulotta G, Pace A, Corso RM, Bahgat A, Vicini C (2021) Effectiveness of drug-induced sleep endoscopy in improving outcomes of barbed pharyngoplasty for obstructive sleep apnea surgery: a prospective randomized trial. Sleep Breath. https://doi.org/10.1007/s11325-021-02528-4
von Elm E, Altman DG, Egger M et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Xie HS, Chen GP, Huang JF et al (2021) Impact of upper airway configuration on CPAP titration assessed by CT during Müller’s maneuver in OSA patients. Respir Physiol Neurobiol 284:103559. https://doi.org/10.1016/j.resp.2020.103559
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268(8):1233–1236. https://doi.org/10.1007/s00405-011-1633-8
Fydrich T, Dowdall D, Chambless DL (1993) Reliability and validity of the Beck Anxiety Inventory. J Anx Disord 6:55–61
Wang YP, Gorenstein C (2013) Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Braz J Psychiatry 35(4):416–431. https://doi.org/10.1590/1516-4446-2012-1048
Iannella G, Lechien JR, Perrone T et al (2022) Barbed reposition pharyngoplasty (BRP) in obstructive sleep apnea treatment: State of the art. Am J Otolaryngol 43(1):103197. https://doi.org/10.1016/j.amjoto.2021.103197
Chiu HY, Chen PY, Chuang LP et al (2017) Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev 36:57–70. https://doi.org/10.1016/j.smrv.2016.10.004
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177. https://doi.org/10.1093/sleep/19.2.156
Vicini C, Meccariello G, Montevecchi F et al (2020) Effectiveness of barbed repositioning pharyngoplasty for the treatment of obstructive sleep apnea (OSA): a prospective randomized trial. Sleep Breath 24(2):687–694. https://doi.org/10.1007/s11325-019-01956-7
Pang KP, Vicini C, Montevecchi F et al (2020) Long-term complications of palate surgery: a multicenter study of 217 patients. Laryngoscope 130(9):2281–2284. https://doi.org/10.1002/lary.28432
Gulotta G, Iannella G, Meccariello G et al (2021) Barbed suture Extrusion and Exposure in palatoplasty for OSA: What does it mean? Am J Otolaryngol 42(4):102994. https://doi.org/10.1016/j.amjoto.2021.102994
Maniaci A, Di Luca M, Lechien JR, Iannella G, Grillo C, Grillo CM, Merlino F, Calvo-Henriquez C, De Vito A, Magliulo G, Pace A, Vicini C, Cocuzza S, Bannò V, Pollicina I, Stilo G, Bianchi A, La Mantia I (2022) Lateral pharyngoplasty vs. traditional uvulopalatopharyngoplasty for patients with OSA: systematic review and meta-analysis. Sleep Breath. https://doi.org/10.1007/s11325-021-02520-y
Rashwan MS, Montevecchi F, Firinua E et al (2018) Let’s know from our patients: PPOPS score for palate surgery evaluation/a pilot study. Eur Arch Otorhinolaryngol 275(1):287–291. https://doi.org/10.1007/s00405-017-4795-1
Lin HC, Lee CY, Friedman M et al (2018) Effects of minimally invasive surgery for patients with OSA on quality of life. Ann Otol Rhinol Laryngol 127(2):118–123. https://doi.org/10.1177/0003489417750164
Quintana-Gallego E, Carmona-Bernal C, Capote F et al (2004) Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients. Respir Med 98(10):984–989
Pillar G, Lavie P (1998) Psychiatric symptoms in sleep apnea syndrome: effects of gender and respiratory disturbance index. Chest 114(3):697–703
Smith R, Ronald J, Delaive K et al (2002) What are obstructive sleep apnea patients being treated for prior to this diagnosis? Chest 121(1):164–172
Shepertycky MR, Banno K, Kryger MH (2005) Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Sleep 28(3):309–314
Ishman SL, Benke JR, Cohen AP, Stephen MJ, Ishii LE, Gourin CG (2014) Does surgery for obstructive sleep apnea improve depression and sleepiness? Laryngoscope 124(12):2829–2836. https://doi.org/10.1002/lary.24729
Burlon G, Tepedino M, Laurenziello M et al (2020) Evaluation of factors that influence the success rate of OSA treatment with a customised adjustable MAD device - a retrospective study. Acta Otorhinolaryngol Ital 40(4):297–303. https://doi.org/10.14639/0392-100X-N0307
Evans SS, Richman J, Cho DY, Withrow K (2020) Increasing preoperative apnea severity improves upper airway stimulation response in OSA treatment. Laryngoscope 130(2):556–560. https://doi.org/10.1002/lary.28009
Petri N, Christensen IJ, Svanholt P, Sonnesen L, Wildschiødtz G, Berg S (2019) Mandibular advancement device therapy for obstructive sleep apnea: a prospective study on predictors of treatment success. Sleep Med 54:187–194. https://doi.org/10.1016/j.sleep.2018.09.033
Bakker JP, O’Keeffe KM, Neill AM, Campbell AJ (2014) Continuous positive airway pressure treatment for obstructive sleep apnoea: Maori, Pacific and New Zealand European experiences. J Prim Health Care 6(3):221–228 (Published 2014 Sep 1)
Elsobki A, Moussa HH, Eldeeb ME, Fayed A, Elzayat S (2022) Efficacy, predictors of success and failure of an updated lateral pharyngoplasty approach as an independent procedure in treating obstructive sleep apnea with CPAP failures. Eur Arch Otorhinolaryngol 279(2):945–953. https://doi.org/10.1007/s00405-021-06825-2
Shie DY, Tsou YA, Tai CJ, Tsai MH (2013) Impact of obesity on uvulopalatopharyngoplasty success in patients with severe obstructive sleep apnea: a retrospective single-center study in Taiwan. Acta Otolaryngol 133(3):261–269. https://doi.org/10.3109/00016489.2012.741328
Vroegop AV, Vanderveken OM, Boudewyns AN et al (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1249 cases. Laryngoscope 124(3):797–802. https://doi.org/10.1002/lary.24479
Ravesloot MJ, de Vries N (2011) One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope 121(12):2710–2716. https://doi.org/10.1002/lary.22369
Martínez-Ruíz de Apodaca P, Carrasco-Llatas M, Matarredona-Quiles S, Valenzuela-Gras M, Dalmau-Galofre J (2022) Long-term stability of results following surgery for obstructive sleep apnea (OSA). Eur Arch Otorhinolaryngol 279(1):373–380. https://doi.org/10.1007/s00405-021-06781-x
Friberg D, Sundman J, Browaldh N (2020) Long-term evaluation of satisfaction and side effects after modified uvulopalatopharyngoplasty. Laryngoscope 130(1):263–268. https://doi.org/10.1002/lary.27917
Funding
Any funding did not support this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were following the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maniaci, A., Ferlito, S., Lechien, J.R. et al. Anxiety, depression and sleepiness in OSA patients treated with barbed reposition pharyngoplasty: a prospective study. Eur Arch Otorhinolaryngol 279, 4189–4198 (2022). https://doi.org/10.1007/s00405-022-07369-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07369-9