Abstract
Purpose
Several studies have been performed using recently developed smartphone-based acoustic analysis techniques. We investigated the effects of septoplasty and turbinoplasty in patients with nasal septal deviation and turbinate hypertrophy accompanied by snoring by recording the sounds of snoring using a smartphone and performing acoustic analysis.
Methods
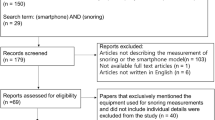
A total of 15 male patients who underwent septoplasty with turbinoplasty for snoring and nasal obstruction were included in this prospective study. Preoperatively and 2 months after surgery, their bed partners or caregivers were instructed to record the snoring sounds. The intensity (dB), formant frequencies (F1, F2, F3, and F4), spectrogram pattern, and visual analog scale (VAS) score were analyzed for each subject.
Results
Overall snoring sounds improved after surgery in 12/15 (80%) patients, and there was significant improvement in the intensity of snoring sounds after surgery (from 64.17 ± 12.18 dB to 55.62 ± 9.11 dB, p = 0.018). There was a significant difference in the F1 formant frequency before and after surgery (p = 0.031), but there were no significant differences in F2, F3, or F4. The change in F1 indicated that patients changed from mouth breathing to normal breathing. The degree of subjective snoring sounds improved significantly after surgery (VAS: from 5.40 ± 1.55 to 3.80 ± 1.26, p = 0.003).
Conclusion
Our results confirm that snoring is reduced when nasal congestion is improved, and they demonstrate that smartphone-based acoustic analysis of snoring sounds can be useful for diagnosis.


Similar content being viewed by others
References
Pevernagie D, Aarts RM, De Meyer M (2010) The acoustics of snoring. Sleep Med Rev 14(2):131–144. https://doi.org/10.1016/j.smrv.2009.06.002
Young T, Palta M, Dempsey J et al (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. https://doi.org/10.1056/nejm199304293281704
Stradling J (1995) Obstructive sleep apnoea: definitions, epidemiology, and natural history. Thorax 50(6):683–689. https://doi.org/10.1136/thx.50.6.683
Stallman JS, Lobo JN, Som PM (2004) The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR AmJ Neuroradiol 25(9):1613–1618
Kao YH, Shnayder Y, Lee KC (2003) The efficacy of anatomically based multilevel surgery for obstructive sleep apnea. Otolaryngol Head Neck Surg 129(4):327–335. https://doi.org/10.1016/s0194-5998(03)00711-3
Hytonen ML, Lilja M, Makitie AA, Sintonen H, Roine RP (2012) Does septoplasty enhance the quality of life in patients? Eur Arch Otorhinolaryngol 269(12):2497–2503. https://doi.org/10.1007/s00405-012-1931-9
Meen EK, Chandra RK (2013) The role of the nose in sleep disordered breathing. Am J Rhinol Allergy 27(3):213–220. https://doi.org/10.2500/ajra.2013.27.3876
Olszewska E, Rutkowska J, Czajkowska A, Rogowski M (2012) Selected surgical managements in snoring and obstructive sleep apnea patients. Med Sci Monit 18(1):CR13–R18. https://doi.org/10.12659/msm.882193
Li HY, Lee LA, Wang PC, Fang TJ, Chen NH (2009) Can nasal surgery improve obstructive sleep apnea: subjective or objective? Am J Rhinol Allergy 23(6):51–55. https://doi.org/10.2500/ajra.2009.23.3358
Ben Israel N, Tarasiuk A, Zigel Y (2012) Obstructive apnea hypopnea index estimation by analysis of nocturnal snoring signals in adults. Sleep 35:1299–1305. https://doi.org/10.5665/sleep.2092
Shin H, Cho J (2014) Unconstrained snoring detection using a smartphone during ordinary sleep. Biomed Eng Online 15(13):116. https://doi.org/10.1186/1475-925x-13-116
Koo SK, Kwon SB, Moon JS, Lee SH, Lee HB, Lee SJ (2018) Comparison of snoring sounds between natural and drug-induced sleep recorded using a smartphone. Auris Nasus Larynx 45(4):777–782. https://doi.org/10.1016/j.anl.2017.09.005
Koo SK, Kwon SB, Kim YJ, Moon JIS, Kim YJ, Jung SH (2017) Acoustic analysis of snoring sounds recorded with a smartphone according to obstruction site in OSAS patients. Eur Arch Otorhinolaryngol 274(3):1735–1740. https://doi.org/10.1007/s00405-016-4335-4
Park S (1993) Flow-regulatory function of upper airway in health and disease: a unified pathogenetic view of sleep-disordered breathing. Lung 171(6):311–333. https://doi.org/10.1007/bf00165698
Fitzpatrick M, McLean H, Urton A, Tan A, Donnell D, Driver H (2003) Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J 22(5):827–832. https://doi.org/10.1183/09031936.03.00047903
Li H, Wang P, Chen Y, Lee L, Fang T, Lin H (2011) Critical appraisal and meta-analysis of nasal surgery for obstructive sleep apnea. Am J Rhinol Allergy 25:45–49. https://doi.org/10.2500/ajra.2011.25.3558
Choi J, Kim E, Kim Y, Kim T, Choi J, Kwon S et al (2011) Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol Allergy 25:338–341. https://doi.org/10.2500/ajra.2011.25.3654
Virkkula P, Bachour A, Hytönen M, Salmi T, Malmberg H, Hurmerinta K et al (2006) Snoring is not relieved by nasal surgery despite improvement in nasal resistance. Chest 129(1):81–87. https://doi.org/10.1378/chest.129.1.81
Sufioglu M, Ozmen O, Kasapoglu F, Demir U, Ursavas A, Erisen L et al (2012) The efficacy of nasal surgery in obstructive sleep apnea syndrome: a prospective clinical study. Eur Arch Otorhinolaryngol 269(2):487–494. https://doi.org/10.1007/s00405-011-1682-z
Hormann K, Verse T, Nasal surgery. In Surgery for Sleep Disordered Breathing (2005) Berlin. Springer, Heidelberg, New York, pp 13–17
Hume K (2010) Sleep disturbance due to noise: current issues and future research. Noise Health 12(47):70–76
Wilson K, Stoohs RA, Mulrooney TF, Johnson LJ, Guilleminault C, Huang Z (1999) The snoring spectrum: acoustic assessment of snoring sound intensity in 1139 individuals undergoing polysomnography. Chest 115(3):762–770. https://doi.org/10.1378/chest.115.3.762
Koo SK, Park GH, Koh TK, Jung SH, Lee HB, Ji CR (2020) Effect of mouth closure on upper airway obstruction in patients with obstructive sleep apnoea exhibiting mouth breathing: a drug-induced sleep endoscopy study. Eur Arch Otorhinolaryngol. 277(6):1823–1828. https://doi.org/10.1007/s00405-020-05904-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no potential conflict of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent: Informed consent was obtained from all individual participants included in the study. The study was approved by the Institutional Review Board of Busan Saint Mary’s medical center (Approval No. BSM-2017-06).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koo, S.K., Kwon, S.B., Koh, T.K. et al. Acoustic analyses of snoring sounds using a smartphone in patients undergoing septoplasty and turbinoplasty. Eur Arch Otorhinolaryngol 278, 257–263 (2021). https://doi.org/10.1007/s00405-020-06268-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06268-1