Abstract
Objectives
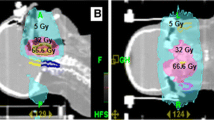
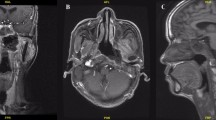
Patients with nasopharyngeal cancer are candidates for proton radiotherapy due to large and comprehensive target volumes, and the necessity for sparing of healthy tissues. The aim of this work is to evaluate treatment outcome and toxicity profile of patients treated with proton pencil-beam scanning radiotherapy.
Materials and methods
Between Jan 2013 and June 2018, 40 patients were treated for nasopharyngeal cancer (NPC) with IMPT (proton radiotherapy with modulated intensity). Median age was 47 years and the majority of patients had locally advanced tumors (stage 2–8 patients. (20%); stage 3–18 patients (45%); stage 4A–10 patients. (25%); stage 4B–4 patients. (10%). Median of total dose was 74 GyE (70–76 GyE) in 37 fractions (35–38). Bilateral neck irradiation was used in all cases. Concomitant chemotherapy was applied in 34 cases. (85%). Median follow-up time was 24 (1.5–62) months.
Results
Two-year overall survival (OS), disease-free survival (DFS), and local control (LC) were 80%, 75%, and 84%, respectively. Acute toxicity was generally mild despite large target volumes and concurrent application of chemotherapy with skin toxicity and dysphagia reported as the most frequent acute side effects. The insertion of a percutaneous endoscopic gastrectomy (PEG) was necessary in four cases (10%). Serious late toxicity (G > 3. RTOG) was observed in two patients (5%) (dysphagia and brain necrosis).
Conclusion
IMPT for nasopharyngeal cancer patients is feasible with mild acute toxicity. Treatment outcomes are promising despite the high percentage of advanced disease in this group.

Similar content being viewed by others
References
Chen JL, Huang YS, Kuo SH et al (2017) Intensity-modulated radiation therapy achieves better local control compared to three-dimensional conformal radiation therapy for T4-stage nasopharyngeal carcinoma. Oncotarget 8(8):14068–14077. https://doi.org/10.18632/oncotarget.12736
Gupta S, Kong W, Booth CM, Mackillop WJ (2014) Impact of concomitant chemotherapy on outcomes of radiation therapy for head-and-neck cancer: a population-based study. Int J Radiat Oncol Biol Phys 88(1):115–121. https://doi.org/10.1016/j.ijrobp.2013.09.052
Jiang L, Huang C, Gan Y et al (2018) Radiation-induced late dysphagia after intensity-modulated radiotherapy in nasopharyngeal carcinoma patients: a dose-volume effect analysis. Sci Rep 8(1):16396. https://doi.org/10.1038/s41598-018-34803-y
Grégoire V, Ang K, Budach W et al (2014) Delineation of the neck node levels for head and neck tumors: a update DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol. https://doi.org/10.1016/j.radonc.2013.10.010(Epub 2013 Oct 31)
Lee AW, Ng WT, Pan JJ (2018) International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiother Oncol 126(1):25–36
Biau J, Lapeyre M, Troussier I (2019) Selection of lymph node target volumes for definitive head and neck radiation therapy: a 2019 Update. Radiother Oncol 134:1–9. https://doi.org/10.1016/j.radonc.2019.01.018(Epub 2019 Jan 30)
Romesser PB, Cahlon O, Scher ED et al (2016) Proton beam reirradiation for recurrent head and neck cancer: multi-institutional report on feasibility and early outcomes. Int J Radiat Oncol Biol Phys 95(1):386–395. https://doi.org/10.1016/j.ijrobp.2016.02.036
Beddok A, Feuvret L, Noël G et al (2019) Boost in proton for locally advanced nasopharyngeal carcinoma: a curie institute experience. Cancer Radiother 23(4):304–311. https://doi.org/10.1016/j.canrad.2019.01.003
Widesott L, Pierelli A, Fiorino C (2008) Intensity-modulated proton therapy versus helical tomotherapy in nasopharynx cancer: planning comparison and NTCP evaluation. Int J Radiat Oncol Biol Phys. 72(2):589–596. https://doi.org/10.1016/j.ijorbp.2008.05.065
Lewis GD, Holliday EB, Kocak-Uzel E (2016) Intensity-modulated proton therapy for nasopharyngeal carcinoma: decreased radiation dose to normal structures and encouraging clinical outcomes. Head Neck 38(1):E1886–E1895. https://doi.org/10.1002/hed.24341
Jakobi A, Bandurska-Luque A, Stützer K et al (2015) Identification of patient benefit from proton therapy for advanced head and neck cancer patients based on individual and subgroup normal tissue complication probability analysis. Int J Radiat Oncol Biol Phys 92(5):1165–1174. https://doi.org/10.1016/j.ijrobp.2015.04.031
Iwata H, Toshito T, Hayashi K et al (2019) Proton therapy for non-squamous cell carcinoma of the head and neck: planning comparison and toxicity. J Radiat Res 60(5):612–621
van Dijk LV, Steenbakkers RJ, ten Haken B et al (2016) Robust intensity modulated proton therapy (IMPT) increases estimated clinical benefit in head and neck cancer patients. PLoS ONE 11(3):e0152477. https://doi.org/10.1371/journal.pone.0152477
Malyapa R, Lowe M, Bolsi A (2016) Evaluation of robustness to setup and range uncertainties for head and neck patients treated with pencil beam scanning proton therapy. Int J Radiat Oncol Biol Phys 95(1):154–162. https://doi.org/10.1016/j.ijrobp.2016.02.016
Stock M, Gora J, Perpar A (2019) Harmonization of proton treatment planning for head and neck cancer using pencil beam scanning: first report of the IPACS collaboration group. Acta Oncol 8:1–11. https://doi.org/10.1080/0284186X.2019.1648858
Góra J, Kuess P, Stock M et al (2015) ART for head and neck patients: On the difference between VMAT and IMPT. Acta Oncol 54(8):1166–1174. https://doi.org/10.1080/0284186X.2019.1648858
Müller BS, Duma MN, Kampfer S et al (2015) Impact of interfractional changes in head and neck cancer patients on the delivered dose in intensity modulated radiotherapy with protons and photons. Phys Medica 31(3):266–272. https://doi.org/10.1016/j.ejmp.2015.02.007
Fountzilas G, Ciuleanu E, Bobos M et al (2012) Induction chemotherapy followed by concomitant radiotherapy and weekly cisplatin versus the same concomitant chemoradiotherapy in patients with nasopharyngeal carcinoma: a randomized phase II study conducted by the Hellenic Cooperative Oncology Group (HeCOG) with biomarker evaluation. Ann Oncol 23:427–435. https://doi.org/10.1093/annonc/mdr116
Cao CN, Luo JW, Gao L et al (2015) Concurrent chemotherapy for T4 classification nasopharyngeal carcinoma in the era of intensity-modulated radiotherapy. PLoS ONE 10(3):e0119101. https://doi.org/10.1371/journal.pone.0119101
Lee N, Harris J, Garden AS et al (2009) Intensity-modulated radiation therapy with or without chemotherapy for nasopharyngeal carcinoma: radiation therapy oncology group phase II trial 0225. J Clin Oncol 27(22):3684–3690. https://doi.org/10.1200/JCO.2008.19.9109
Songthong AP, Kannarunimit D, Chakkabat C, Lertbutsayanukul C (2015) A randomized phase II/III study of adverse events between sequential (SEQ) versus simultaneous integrated boost (SIB) intensity modulated radiation therapy (IMRT) in nasopharyngeal carcinoma; preliminary result on acute adverse events. Radiat Oncol 10:166. https://doi.org/10.1186/s13014-015-0472-y
Levin WP, Kooy H, Loeffler JS, DeLaney TF (2005) Proton beam therapy. Br J Cancer 93(8):849–854. https://doi.org/10.1038/sj.bjc.6602754
Ou X, Zhou X, Shi Q et al (2015) Treatment outcomes and late toxicities of 869 patients with nasopharyngeal carcinoma treated with definitive intensity modulated radiation therapy: new insight into the value of total dose of cisplatin and radiation boost. Oncotarget 6(35):38381–38397. https://doi.org/10.18632/oncotarget.5420
Funding
The work was supported by the European Regional Development Fund-Project: “Engineering Applications of Microworld Physics” (No. CZ.02.1.01/0.0/0.0/16_019/0000766).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that there is no conflict of interest, we follow the Ethical Standard Statement, and we grant the informed consent with publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiří, K., Vladimír, V., Michal, A. et al. Proton pencil-beam scanning radiotherapy in the treatment of nasopharyngeal cancer: dosimetric parameters and 2-year results. Eur Arch Otorhinolaryngol 278, 763–769 (2021). https://doi.org/10.1007/s00405-020-06175-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06175-5